fistula
What is a fistula?
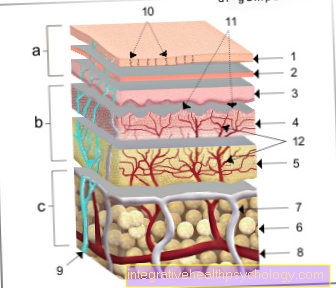
A fistula is a non-natural, tubular connection between two cavities within the human body or on the body surface.
The term "fistula" is derived from the Latin word "Fistula”Which means“ tube ”.
A fistula can occur as a result of an illness, in which case it is referred to as "pathological" (diseased).
In the course of surgical interventions, artificial connections can also be created, which are also known as fistulas.
A distinction is made between an internal and an external fistula.
In the case of an external fistula, a hollow organ is unnaturally connected to the body surface through a tubular opening.
An example of this is the so-called "enterocutaneous fistula", in which, as the name suggests, the inside of the intestine has an additional outlet to the skin.
An internal fistula is the opening between two cavities within the body.
An example of this are arteriovenous fistulas, in which the arterial and venous vessels are in contact via a tubular connection.
You might also be interested in: Fistula duct

These are the causes
A distinction must be made between a congenital and an acquired fistula.
During embryonic development, during which the organs are created, develop and take their final place in the body, malformations can occur.
These can have serious consequences.
In some cases two cavities arise from the originally same organ structure.
If they do not separate completely, connections can remain as a fistula.
An example of this is the oesophagotracheal fistula, in which the esophagus and trachea have an opening to each other that has remained from the embryonic period.
Fistulas can also arise as a result of injuries, for example during childbirth. The rectovaginal fistula, known as the perineal tear, is an example of this.
Some diseases, especially inflammation, can cause fistulas.
For example, in Crohn's disease, the inflammation of the bowel that produces pus sometimes creates a fistula.
In everyday hospital life, artificially induced fistulas can sometimes occur.
These can be created consciously as part of an operation, for example as an artificial anus, or arise unintentionally.
In this case, a failure with invasive medical supplies may result in a perforation.
It is a possible complication in endoscopic surgery.
What are the symptoms?
The symptoms of a fistula vary widely. They depend on the situation, location and extent of the fistula. In many cases they can be painful, especially if they are superficial.
An unnatural opening of two neighboring organs can lead to various symptoms and clinical pictures.
Blood, pus or any kind of fluid such as stool, urine, bile can be secreted through the fistula.
The superficial fistulas can cause local pain and discomfort.
Liquid can leak to the outside.
On the other hand, it can easily lead to local inflammation, which can also be painful and cause complications.
Depending on the organ area affected, the symptoms are very different.
A rare form of a fistula is the "aortoenteral fistula", which connects the aorta with the intestine and can cause acute, life-threatening bleeding into the intestine. Such a fistula is difficult to treat and has a very poor prognosis.
What are fistulous ducts?
If there is an unnatural connection between different hollow organs or between a hollow organ and the body surface, it is called a fistula.
The cause of the formation of a fistula is usually an encapsulated inflammation of an organ.
The resulting abscess then favors the formation of the fistulous duct, whereby the pus is supposed to be transported out of the organ.
On the other hand, fistula ducts can also be congenital or artificially created by a doctor for the treatment of various diseases.
Congenital fistulas are persistent fistulas that should originally have closed before birth.
The urachus fistula, i.e. the connection between the urinary bladder and the navel, is an example of this.
An example of an artificially created fistula is the external gastric fistula.
The doctor puts on these to artificially feed the patient during an operation.
Where are there fistulas everywhere?
Fistulas arise from various causes in parts of the body with cavities.
In rare cases, they can occur between two vessels, for example in an arteriovenous fistula.
This leads to an exchange of blood between both vessels. The symptoms here are very different.
Typical locations of fistulas are e.g. between the intestine and urinary bladder (“enterovesikal”), urinary bladder and vagina (“vesicovaginal”), urethra and vagina (“urethrovaginal”), esophagus and trachea (“oesophagotracheal”) or rectum and vagina (“rectovaginal”).
Fistulas can also appear on the teeth or gums.
The occurrence of fistulas is not limited to the hollow organs listed here, but can theoretically occur in all hollow organs.
Fistulas can also exist between organ areas or cavities and the skin.
The cavities then have a non-natural exit to the body surface.
This occurs, among other things, on the intestine ("enterocutaneous fistula"), which can be caused by inflammation or is artificially created.
A congenital or acquired hole in the skin on the tailbone (tailbone fistula) is also called a fistula or "Pilonidal sinus" designated.
Fistula in the mouth
Fistulas in the mouth are not uncommon and can be very painful. Fistula formation at the tooth root is very common as a result of inflammation.
The fistula can appear anywhere in the mouth, on the lip, on the roof of the mouth, on the gums (fistula on the gums) under the tongue or in the throat. Further fistulas in the mouth area are very rare.
In the throat, however, there can be various types of fistulas, which are often caused by an embryonic malposition.
Fistula under the tongue
Fistulas below the tongue are very rare.
Rather, aphthae often develop on the tongue, which can burn and cause pain.
This is a damaged part of the tongue lining.
The most common places for aphthous ulcers of the tongue are the edge of the tongue and the tip of the tongue.
Aphthae are rarely found on the underside of the tongue.
The cause of the development of these aphthous ulcers is still unknown.
Very rarely a tooth root inflammation can lead to the formation of a fistula up to the underside of the tongue.
Fistula on the tooth
Fistula formation on the tooth can also occur in the oral cavity as part of inflammatory diseases.
They can develop primarily at the tooth root.
A tooth root inflammation is the cause in many cases.
Such an inflammation can have many causes and it is not always the patient's direct fault.
Poor oral hygiene, an unhealthy diet or chronic illness can be the problem.
The inflammatory reaction of the body can, in unfavorable cases, lead to tooth root inflammation, which must be treated urgently.
Many try to endure the pain until it goes away.
If left untreated, however, the tooth root can die off.
The accumulated pus sometimes causes severe pain and makes its way into the oral cavity.
This leads to the formation of a fistula.
The pain then often stops quite suddenly, which in this case is a bad sign.
However, it is imperative to treat the cause of the inflammation, even though the pain has disappeared.
Fistulas in the mouth area can also occur in children, which is why adequate oral hygiene must always be observed.
Regular visits to the dentist, especially if there is pain, are important.
For more information, see: Fistula on the tooth
Fistula on the neck
A cervical fistula creates a tubular connection between the inner pharynx and an opening in the neck.
The reason for this lies in a disturbance during embryonic development.
In the womb there is a passage in the neck area between the original thyroid anlage, which is at the base of the tongue, and the end position of the thyroid gland.
Normally, this so-called thyroglossal duct recedes in the course of embryonic development.
If this does not happen, the front (medial) neck fistula forms.
The fistula on the neck can be recognized by the painless swelling of the neck.
If it becomes infected, it may cause pain, hardening, or an encapsulated, purulent accumulation (an abscess) under the skin.
Fistula on the anus
A fistula on the anus is also known as an "anal fistula" and is a very common problem.
Symptoms range from itching and pain to secretion on the surface of the skin.
However, the symptoms depend on which direction the fistula is spreading.
Congenital anal fistulas are very rare.
The coccyx fistula is located on the surface of the skin around the buttocks, but rarely has contact with the anus.
In most cases, a fistula in the anus is a result of inflammation in this area of the intestine.
Often glands are affected, which are located in the mucous membrane of the anus and can become inflamed.
When inflamed, purulent secretion is secreted, which can form an abscess (abscess on the buttocks) and cause a fistula to form if it has no opening to drain. Other intestinal diseases that come into question are "Crohn's disease", "ulcerative colitis" or "diverticulitis".
The direction in which the fistula spreads can vary.
If the fistula develops towards the back, it can reach the surface of the skin and break through.
Then there is a second anus, through which mainly pus drains.
If the fistula is directed in the opposite direction, a rectovaginal fistula can occur.
This is often noticed by vaginal drainage of pus and stool.
Otherwise, the fistula often ends blindly in the tissue.
In rare cases, anal fistulas can develop in other ways.
Tears in the anus, so-called “anal fissures”, but also tumor diseases or HIV infections are possible.
Fistula on the navel
Fistulas can also appear on the belly button.
This is also known as "umbilical fistula" or "yolk duct fistula".
A distinction must be made between an umbilical cord break ("omphalocele"), an urachus fistula and an umbilical fistula.
All three are in most cases a holdover from embryonic development.
The umbilical fistula goes back to a structure of the embryo, the so-called "yolk duct" or "Omphaloenteric duct“.
In child development, it connects the yolk duct with the developing child's bowel.
The yolk duct ends at the navel and if it persists until after birth, it forms a fistula between the intestine and the navel.
If this passage is open, the typical symptoms of an umbilical fistula occur.
Stool, bile, mucus and other intestinal contents can be directed to the outside through the belly button.
On the other hand, pathogens can penetrate the inside of the body unhindered and cause diseases and infections.
The umbilical fistula should therefore be treated so that there is no unpleasant inflammation.
More on this: Fistula on the navel
Fistula on the intestine
Fistulas can form in many parts of the intestine.
The entire gastrointestinal tract extends from the oral cavity to the anus.
Fistulas can develop in the oral cavity.
A developmental fistula to trachea can also occur in the esophagus.
There are many places in the small and large intestine for potential fistula formation.
Few of them are innate. An example of this is the umbilical fistula, which is a relic of the embryonic era.
Most intestinal fistulas arise as a result of inflammatory bowel disease.
The typical diseases that cause pus production with resulting fistula formation are Crohn's disease, ulcerative colitis and diverticulitis.>
Depending on the direction in which the fistula formation spreads, there are very different clinical pictures.
This can result in connections to the skin (enterocutaneous fistulas), connections to other parts of the intestine (interenteric fistulas) or connections to other organs such as the vagina (rectovaginal fistulas).
Under certain circumstances, intestinal fistulas, deliberate or unintentional as a result of surgical interventions, can occur.
Read more about the topic here: Fistula in the intestine
Coccyx- what is it?
A pilonidal sinus is caused by inflammation of the subcutaneous fat in the coccyx region, most often in the gluteal fold.
This is what happens - so it is assumed today - when hair breaks off in this region and grows into the skin.
This creates a hair nest in the subcutaneous fatty tissue.
The enlarged hair shaft creates black depressions on the surface of the skin.
If these pits under the skin become inflamed, this can lead to an abscess.
This can result in fistulas that grow deeper into the tissue or expand towards the surface of the skin.
Risk factors that favor the development of a coccyx fistula are:
-
thick hair
-
Obesity
-
sedentary activities
The course of the disease can take three different paths:
In the asymptomatic form, the patients usually have no symptoms.
Only the black depressions in the gluteal fold are visible.
However, the asymptomatic form can also change into an acute or chronic form.
The acute form is characterized by inflammation of the hair nest pit.
Typical signs of inflammation occur here: swelling, redness and pain.
The chronic form leads to the leakage of pus or blood from the fistula opening, especially if there is pressure on the corresponding region of the fistula opening.
What is an AV fistula?
An arteriovenous fistula is a so-called short-circuit connection between an artery and a vein.
This short-circuit connection can be innate or arise in the course of life through various diseases.
However, acquired ones are far more common, e.g. These AV fistulas arise from injuries to the corresponding artery and the vein in the immediate vicinity.
As part of dialysis treatment, an AV fistula is even created on purpose to reduce the likelihood of clots forming in the affected vein through faster blood flow.
Symptoms vary: Congenital superficial fistulas can swell and then look red-brown.
An acquired AV fistula, if left untreated, can lead to low blood pressure, which can cause fatigue or drowsiness.
This is because the short-circuit connection results in excessively high blood pressure in the vein due to the faster blood flow.
The high blood pressure causes the vein walls to widen and consequently the blood pressure drops.
The heart must counteract this low blood pressure, which is why the heart rate and stroke volume increase.
If the heart is overwhelmed, it can lead to heart failure.
The so-called steal syndrome or bleeding phenomenon occurs when the AV fistula “sucks” so much blood that symptoms such as numbness, cramps, and pain develop.
Can a fistula also heal on its own?
Fistulas usually cannot heal on their own.
However, if there is a fistula, surgery does not necessarily have to be carried out.
Depending on the doctor's diagnosis, it may also be possible to wait.
So-called thread drainage is a good alternative to surgery.
In the case of anal fistulas, for example, silicone threads are inserted into the fistula so that the fluid in the duct should drain off and the fistula dries out.
How are fistulas operated?
There are various surgical options that are used depending on the location, the organs involved and the cause.
In a fistulotomy, the fistula is either split lengthways or peeled out, then exposed and finally cleaned.
The fistula ultimately heals through the subsequent open wound healing.
However, the foci of infection should also be treated, as otherwise a fistula can again form.
Furthermore, silicone threads can be placed in the fistula duct, which is known as thread drainage.
This means that the fluids that have accumulated in the fistula can drain away and the fistula duct heals.
This method is often used in inflammatory bowel disease, Crohn's disease.
In this way, recurrent fistula can be combated.
As an alternative, the fistula can also be cleaned first and then removed sparingly.
This method is called a fistulectomy.
Abscess vs. Fistula - What's the Difference?
An abscess is caused by an accumulation of bacteria in the affected tissue.
This creates an encapsulated cavity filled with pus at this location.
This so-called focus of inflammation (place of inflammation) can now lead to the formation of a hollow tube from the place of the abscess to the surface of the body so that the accumulated pus can flow away.
This is known as a fistula or fistula duct.
Thus, an abscess can lead to the formation of a fistula.
The causes of a fistula development are not limited to abscesses.
The tubular connection between hollow organs or between a hollow organ and the body surface can also be innate, as is the case, for example, with the palatal fistula.
Furthermore, a fistula can also be artificially created by the doctor, e.g. the AV fistula as part of dialysis treatment.