Gingivitis
Synonyms
Inflammation of the gums
introduction
Under the term "Gingivitis“Is understood in the Dentistry an inflammation of the Gums.
The gingivitis must be technically different from the so-called Periodontal disease, the spread of inflammatory processes within the periodontium. Nevertheless, there is between gingivitis and Periodontal disease (wrongly known under the term periodontal disease) a causal connection, because in many cases an untreated inflammation of the gums sooner or later leads to inflammation of the gums.

Gingivitis is generally triggered by poor or poorly performed oral hygiene. Bacteria and / or other pathogens living in the mouth reach the depths through the smallest gaps between the tooth and the gum and trigger inflammatory processes there by secreting their metabolic end products.
As a result, the organism reacts by releasing special inflammatory factors and increasing blood flow to the tissue. First of all, this creates deep gum pockets. In preventive therapy (prophylaxis) For this reason, it is mainly about learning suitable teeth cleaning techniques.
The focus is on the targeted care of the spaces between the teeth and the edge areas between tooth substance and gums. It is now assumed that while ineffective oral hygiene is the main cause of the development of most dental (supporting apparatus) diseases, other factors also play a major role.
These factors include a genetic predisposition (this has been observed in extensive studies), frequent mouth breathing, nicotine and alcohol consumption.
Gingivitis is one of the most common diseases of all. From the age of 40, it is estimated that every third patient suffers from inflammation of the gums. However, most people do not have general gingivitis. Usually isolated areas within the oral cavity are affected.
These bodies are usually districts that are part of the dental care are difficult to access. (bridges, CrownConstrictions, nesting of the teeth). A pronounced tooth misalignment increases the risk of developing gingivitis enormously.
In addition, if bridged and / or crowned teeth are present, a regular dental check-up should urgently be carried out, as the edge areas of the dental prosthesis in particular form the ideal attachment position for bacteria.
Herpetic gingivitis
The classic clinical picture of herpetic gingivitis is a consequence of infection with type 1 of the herpes simplex virus. It occurs predominantly in children between the ages of two and four, but has also been observed in adolescents and adults. After an incubation period (= time between infection with the pathogen and the first appearance of symptoms) of 4 to 6 days, those affected develop fever, fatigue, vomiting, tendency to cramp, severe restlessness and changes in the oral cavity, which are popularly known as "mouth rot "Are designated.
Those affected tend to have bad breath, increased saliva production and swelling of the lymph nodes in the head and neck area. The gums are very red and numerous blisters form. After a short time, the blisters turn into round depressions and hurt the person concerned. The gingiva can also be covered by whitish-yellowish secretions. The viral infection can also be accompanied by inflammation of the throat and severe cough and sore throat. As is so often the case, initial illnesses in adulthood are more complicated than in early childhood.
The changes in the oral mucous membrane in the context of herpetic gingivitis regress within 10 to 14 days with symptomatic treatment. These include bed rest, antipyretic medication, copious amounts of drinking, and careful but careful oral hygiene. The use of an antibiotic is pointless as it has no effect against viruses. In particularly severe cases, the drug acyclovir is prescribed by the attending physician. After an infection, the person affected is immune to renewed illness for a lifetime.
Read on below. Herpes Simplex Virus
Ulcerative gingivitis
The ulcerative gingivitis or also as acute necrotizing ulcerative gingivitis (ANUG) usually begins suddenly in the area between the teeth. What distinguishes it from the other forms of gingivitis is the tissue-destroying nature, which is why the interdental papillae almost "melt away" within a few hours. The destroyed tissue is accompanied by a secretion coating. Crater-shaped defects in the gums are left behind, which tend to affect the rest of the gums or the gum bed and the entire periodontium.
The ANUG is associated with severe pain, bleeding and increased salivation. Those affected suffer from bad-smelling bad breath and taste a putrid taste. The surrounding lymph nodes are swollen and a high temperature is another symptom.
The ANUG often arises from an existing chronic gingivitis and due to a weakened immune system, which is why it arises as a result of diseases of the throat and pharynx. The exact composition of the responsible bacteria is not known today. It is clear, however, that the ANUG is not contagious.
In addition to therapeutic cleaning of the oral cavity, an antibiotic is prescribed to fight the bacteria. Additional rinsing with the active ingredient chlorhexidine can also minimize the bacteria in order to heal the gums. In severe cases, bed rest is appropriate for those affected. During therapy, those affected should resort to soft foods and increase their hydration.
Gravidarum gingivitis
Inflammatory changes in the oral mucosa, known as gingivitis gravidarum, occur relatively frequently during pregnancy. The tissues of the expectant mother become more flexible during pregnancy, including the gums. The gums swell, redden, and bleed excessively. This can only affect individual areas, but also the entire gum. The reduced saliva production during pregnancy and the shift in the pH value to the acidic range make it easier for bacteria to play.
It is not uncommon for tissue to multiply, so-called pregnancy hyperplasia. The tissue usually multiplies from the third month of pregnancy and reaches its greatest extent in the eighth month. The excessively formed gums are very well supplied with blood, which explains the strong tendency to bleed.
Roughly one in five to seventh women will experience these symptoms during pregnancy. Only about 20% of those affected have a severe form of gingivitis gravidarum, 80% only suffer from mild symptoms.
The cause is the shift in the hormonal balance and especially the excessive production of estrogens and progesterone. Gingivitis gravidarum regresses independently as early as the ninth month of pregnancy and after birth at the latest. Only thorough oral hygiene helps therapeutically. In particularly pronounced cases, it is necessary to clean the gums. The expectant mothers are advised to take vitamin C as a support.
Gingivitis in Pregnancy
Inflammation of the gums during pregnancy is recognized by the medical community Gingivitis gravidarum called.
Is gingivitis an indication of HIV?
Changes in the oral cavity that can resemble gingivitis can occur, especially in the early stages of HIV infection. There are often depressions in the oral mucosa in the form of canker sores. Fungal infections in the mouth and throat and hairy cell leukoplakia, which appear as a local whitish change in the oral cavity, are early symptoms of HIV infections. Also an acute, aggressive inflammation of the gums (see above under Ulcerative gingivitis) can also be an early symptom of HIV infection.
If you suspect an HIV infection, please consult your doctor immediately.
You might also be interested in: Symptoms of HIV infection
Marginal gingivitis
In the case of marginal gingivitis, only the free, unattached, marginal gingiva is affected. The term Gingivitis simplex often used as a synonym for marginal gingivitis. Marginal gingivitis often develops due to increased plaque deposits due to inadequate oral hygiene. The bacteria that build up in the plaque produce enzymes and toxins that cause the gums to become inflamed.
The inflammation appears like a garland from tooth to tooth and results in swelling and reddening. The gums are more prone to bleeding. Thorough oral hygiene and removal of the plaque will make the symptoms of inflammation disappear within a few days.
Gingivitis Desquamativa
Gingivitis desquamativa is a special term for inflammation of the gums, which was previously used to denote the severe type with swelling and injuries to the gums.
Today the term gingivitis desquamativa is used to describe inflammation that is triggered by undetectable disease-specific antibodies and cannot be assigned to any other disease. Since the majority of those affected are women between the ages of 40 and 60, disorders of the hormonal balance during menopause are suspected to be the cause.
The appearance is variable. The entire gum, both the free gingiva and the attached, firm gingiva, is often affected by severe redness, swelling and blistering. Bleeding is associated with the symptoms, and these wounds have poor tendency to heal. The diagnosis of Gingivitis desquamativa is only made if the pathology has also clarified by a tissue removal.
Gingivitis simplex
Gingivitis simplex describes a non-specific inflammation of the gums, which is associated with swelling, reddening and increased bleeding of the gums. Gingivitis marginalis is synonymous with gingivitis simplex.
Gingivitis simplex is usually caused by bacterial plaque that, if it has existed for a long time, infects the gums and leads to discomfort. In this mild form of gingivitis, only the free, marginal gingiva is affected; the attached gingiva is not infected.
Gingivitis simplex is primarily caused by poor oral hygiene, but it can also be accompanied by symptoms of influenza or during pregnancy. The bacteria can preferentially form pockets in the interdental spaces because the epithelium is detached from the tooth as a result of the infection. The bacteria can lodge in the pockets and cause bone breakdown, allowing the affected tooth to loosen. In this case, a simple inflammation of the gums would develop into an inflammation of the gums.
Causes of Gingivitis
The causes of gingivitis can be varied, but similar to caries disease, it is usually triggered by bacterial plaque and thus by poor oral hygiene. The term plaque is understood as a tough bio-film, which consists on the one hand of waste products of the bacterial metabolism and on the other hand of food deposits.
Dental plaque that sticks to the tooth surface can in many cases even penetrate under the gumline. In the deep, it settles on and around the tooth root and causes deep gum pockets in the process.
The dental plaque leads to severe inflammatory processes within these gum pockets. In the course of this, the characteristic bleeding gums occur. Gingivitis is a pure (isolated) inflammation of the gums without the involvement of other structures of the periodontium. In most cases, however, the gingivitis is not completely classified as periodontal disease (falsely known as periodontal disease) known, inflammatory disease of the periodontium. This fact is due to the fact that gingivitis usually results in inflammation of the gums if the appropriate treatment measures are not taken. Inflammation around the gums is generally easy to spot. The gums quickly lose their rosy, light color in the affected areas and become increasingly darker. Inadequate or inadequate oral hygiene is still the main cause of gingivitis today.
It has long been known, however, that a number of other factors also promote inflammatory processes in the area of the gums and the gums. In addition to poor oral hygiene, there are factors that favor a possible disease and thus promote the causes of gingivitis. These risk factors include:
- Tobacco use
- increased mouth breathing
- untreated carious teeth
- Life partner with inflammatory processes within the oral cavity
- hormonal changes during pregnancy and a general weak immune system (immune deficiency).
It has been proven that patients who suffer from diabetes (diabetes) suffer from a significantly increased risk of gingivitis.Around one in two people will develop inflammation of the gums (gingivitis) at least once in their lifetime. Long-term stress on the organism can also promote the development of inflammatory processes within the oral cavity. This is related to the stress-induced inhibition of immune cell formation and their function. In the majority of those affected, it even develops an inflammation of the gums that hold the teeth with involvement of the jawbone (periodontitis). Today it is even assumed that a genetic predisposition also plays a certain role.
Symptoms of Gingivitis
The first and most important sign of gingivitis is bleeding around the gums. Pain when brushing your teeth is also not uncommon. Typical symptoms of gingivitis also include severe redness and / or dark discoloration of the gumline. In addition, inflamed gums usually appear swollen and thickened (edema and swelling). In severe cases, so-called ulcerative decay of the affected gums can occur.
Therapy of gingivitis
Therapeutically, in all forms of gingivitis, an attempt is made to thoroughly clean the gums. Intensive cleansing can be sufficient to alleviate the symptoms, provided there is a mild form of gingivitis. In the case of severe forms, the gums may need to be professionally cleaned by the dentist / periodontist by also cleaning the pockets between the teeth.
In support of this, the person affected should use a mouthwash solution that contains the active ingredient chlorhexidine digluconate twice a day for two weeks, as this has been shown to minimize bacteria in the oral cavity.
At the beginning of the therapy, the treating dentist or periodontist will carry out a so-called professional tooth cleaning (PZR). In the course of this, every single tooth is cleaned from all sides with special instruments (curettage).
Due to their individual cut, the curettes are able to remove both soft (plaque) and hard (tartar) deposits from the tooth surface. Alternatively, teeth can also be cleaned using a "sandblaster". From a technical point of view, however, this method is more than questionable, as the small particles of the emitter roughen the tooth surface and thus create new dirt niches.
As a rule, the statutory health insurance companies only cover the costs of such a provision. The patient must therefore raise at least part of the amount himself. The price of a professional teeth cleaning varies greatly from practice to practice (on average the costs are between 70 and 150 euros).
Considering that untreated gingivitis (Gingivitis) can even lead to the loss of otherwise perfectly healthy teeth over a longer period of time, these costs are justified. However, the dental process of professional teeth cleaning is not enough to put a stop to gingivitis for a long time. Above all, the cooperation of the patient concerned is essential for the success of the treatment. Regular check-ups, if necessary a new professional tooth cleaning and, above all, an adequate oral hygiene is essential for the treatment.
In the case of herpetic gingivitis or ANUG, bed rest can also be appropriate, as the body is very weakened by the pathogens and has to regenerate. The dentist also arranges antibiotics for bacterial and antiviral drugs for viral forms of gingivitis in order to quickly rid the body of the infection. In the case of accompanying symptoms such as fever, antipyretic drugs are also conceivable, which reduce the accompanying symptoms of gingivitis.
What drugs help with gingivitis?
Depending on the severity and type of gingivitis, other medications are used.
- In the case of bacterial forms of gingivitis, in addition to thorough cleaning, antibiotics are the most effective drugs that kill the bacteria quickly.
- In viral herpetic gingivitis, antivirals such as acyclovir help render the virus harmless and accelerate the regeneration of the person affected.
- Antipyretic drugs and painkillers are used to alleviate the side effects of gingivitis. This includes, for example, paracetamol, which, in addition to its pain-relieving effect, also has a fever-lowering effect.
Homeopathy for gingivitis
With gingivitis of any kind, globules can also help to overcome inflammation more quickly and to regenerate the gums. At the same time, homeopathy also helps to rehabilitate the weakened immune system of the body and accelerate healing. For gingivitis, the drug of choice is Mercurius solubilis in globule form. Mercurius solubilis in the potency D12 helps to soothe bloody and swollen gums. The usual dosage is five globules three times a day. If you are unsure about the globules, you should consult your dentist.
Home remedies for gingivitis
Home remedies can help soothe irritated and injured gums and accelerate healing, especially in mild forms of gingivitis simplex or marginalis. If there is no significant improvement in symptoms after about a week, a visit to the dentist is urgently recommended.
- Soothing ointments for the lining of the mouth or rinses with alum or aloe vera can soothe the gums and relieve pain symptoms. The rinse should be used three times a day, while ointments or pastes should be applied specifically to local inflammation sites twice a day.
- Herbs such as chamomile, sage and cloves can also be used in rinsing solutions to counteract gum inflammation.
- Ginger is also used as a rinsing solution as a home remedy for gingivitis. With ginger, however, due to its spiciness, care must be taken not to irritate the gums further.
- In general, targeted cooling can help relieve symptoms for a short time and relieve pain.
- The most important thing, however, is thorough oral hygiene to remove the bacterial plaque that causes gingivitis simplex or marginalis and to clean the gums, because if the bacteria remain in the mouth, the gingivitis will also persist.
- For the other forms of gingivitis that are caused by viruses or hormones, home remedies are powerless and cannot regenerate the gums
Read more on the topic: Home remedies for gum inflammation
Diagnosis of gingivitis

In special cases and / or when the inflammatory processes penetrate into other structures of the tooth support system (for example the jawbone), a specialist in periodontics is recommended (Periodontists) to visit.
At the beginning, a comprehensive screening is carried out (tooth status and tooth supporting apparatus status). This means that both the condition of the tooth substance and the condition of the gums are precisely assessed. In the course of this, the depth of possible gingival pockets is also measured. This measurement is either carried out on behalf of the individual teeth for each jaw quadrant (Periodontal screening index; in short: PSI) or much more extensive in six places around each tooth.
In order to be able to determine the depth of the gingival pockets, the attending dentist guides a narrow, scaled probe between the tooth substance and the gums. The determination of the extent of the gingival pockets is usually absolutely painless and completely harmless to the function of the tooth support apparatus.
Furthermore, a microbial test can be carried out in the course of the preliminary examinations to determine the exact germs. In severe cases, it is also advisable to take an X-ray image (OPG) that shows the teeth in the jaw along with the jawbone. With the help of this X-ray, the condition of the skeleton can be assessed and the extent to which the inflammatory processes have already spread can be assessed.
The actual gingivitis therapy begins with a general prophylaxis session. In the course of this, the patient is shown with special coloring tablets at which points oral hygiene needs to be optimized. This is followed by instructions on a suitable toothbrushing technique, which is adapted to the special conditions within the oral cavity of the individual patient (for more details see gingivitis prophylaxis).
Prevention (prophylaxis)
The most effective way to protect yourself from the development of gingivitis starts at home.
Without regular, adequately performed oral hygiene, gingivitis (Gingivitis) do not prevent. The use of a toothbrush alone is in most cases not enough to completely remove all germs and plaque deposits within the oral cavity. Particularly in patients who suffer from pronounced tooth misalignments or very narrow interdental spaces, areas that are difficult to access exist.
These areas can hardly or not at all be reached by the bristles of a toothbrush. For this reason, dentists recommend the interdental brush at least once a day (synonym: Interdental brush) or to floss. This makes oral hygiene a little more time-consuming, but this seems to be the most successful method of preventing gingivitis. Since the thoroughness of the use of the interdental brushes (and also that of floss) experience shows that it decreases after a few minutes, it is advisable to start in a different quadrant every day. It can therefore be assumed that every quadrant can be completely recorded at least every four days.
Some studies have shown that the risk of developing gingivitis is reduced enormously as a result. In addition, the use of special antibacterial mouth rinses helps to reduce the number of bacteria living in the oral cavity and thus also the formation of plaque. To check the thoroughness of the teeth cleaning and to make any remaining deposits visible, tooth coloring tablets can be used at regular intervals.
Various home remedies can also have a preventive effect if used regularly.
In addition, a dental check-up should be made about every six months. Participation in special prophylaxis programs is also highly recommended. These programs include a visit to the dentist, which should be done every 3 to 6 months as needed. During the individual appointments, the teeth are coated with a special staining solution and plaque deposits are made visible. The ingredients of this staining solution react with different components of the deposits and in this way take on a specific color. These solutions are not only able to make the dental plaque visible to the eye, but can also differentiate between old and new deposits. Most of the preparations used in dental practice use a bluish dye to highlight older deposits (older than 48 hours) and a red dye around new plaque (Plaque) to make visible. Then the dentist or the trained prophylactic assistant (ZMF) tries to optimize the patient's oral hygiene through cleaning instructions. Professional teeth cleaning with removal of loose (plaque) and solid (tartar) deposits concludes such a prophylaxis session.
What are the risks of gingivitis?
The most serious risk of gingivitis (Gingivitis) is the possibility of the inflammatory processes spreading to other structures of the tooth supporting apparatus. This can lead to damage to the jawbone and bone regression. In the worst case, this results in the loss of actually completely healthy teeth. The subsequent supply of the tooth gaps with an implant is extremely difficult due to the missing bone anchor. For this reason, a bridge usually has to be supplied, which in turn ensures that new dirt niches that are difficult to clean are created. In addition, the spread of the inflammatory processes in the area of the jawbone can have damaging effects on dental health. It is not uncommon for an inflammation of the gums (gingivitis) to eventually develop into a painful root inflammation as the inflammation extends to the jawbone.
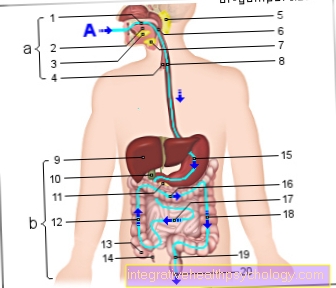
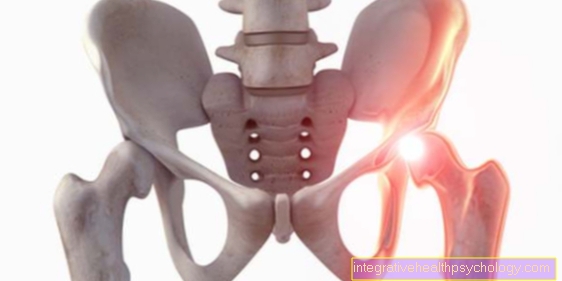
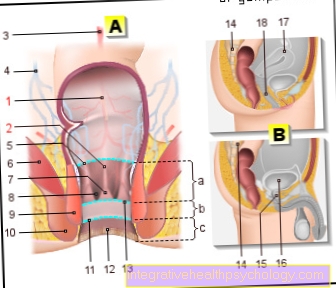
Anatomy of the gums
As part of the oral mucosa (lat. Gingiva) the gums cover the jawbone and the lower parts of the tooth substance attached to it. The gums (Gingiva) counted to the tooth supporting apparatus.
At the upper edge (in the lower jaw at the lower edge; apical) the gingiva continues into the loose oral mucosa. On closer inspection, a garland-shaped border structure can be seen between the gums and the oral mucosa, the so-called Linea garlandiformis. A general distinction is made between two different parts of the gum, the free and the attached gingiva. The free gums are located between each tooth at the bottom of the
Interdental space. Directly below is the gingiva, which is firmly connected to the bone and dental cement by connective tissue fibers ("attached gingiva“).





















.jpg)