Life-support-machine
definition
The heart-lung machine is a device used to relocate the heart and lung functions outside the body. It takes over the pumping function of the heart and the oxygenation function (=Oxygen enrichment) of the lungs while the heart is being operated on. To a heart-lung machine (short HLM) different high medical technology demands are made, as it is involved in crucial processes of the body.

Functions
The heart-lung machine has several functions.
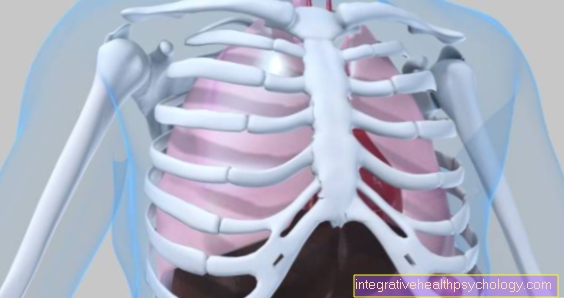
First, their main task, the venous blood return to the heart at the Vena cava and on the main artery (aorta) to be released again in enriched form (i.e. rich in oxygen). The organs The heart and lungs are drawn from the bloodstream except, making operations on these organs possible. But you have to between two bloodstreams distinguish: one hand move through both organs per minute 5-6 liters of blood (the so-called circulation volume), on the other hand, heart and lung tissue are also supplied with blood, after all, they have to be supplied with oxygen. Only the circulation volume is cut, the blood supply to the organs themselves remains, otherwise they would die.
That happens in the heart-lung machine deoxygenated, used blood from the body, and is initially from CO² (Carbon dioxide) purified. This is created as a normal “breakdown product” in the cells, similar to how CO² is produced in a car by burning energy (gasoline). Once this is done, the blood will with it O² (i.e. oxygen) supplied, i.e. oxygenated. At this point it is also possible to do that To warm or cool bloodwhich may be necessary for longer heart operations.
The enriched oxygenated blood is now pumped back via tubes from the heart-lung machine into the body, more precisely into the main artery (aorta). From there it is distributed as usual through the Arteries in all areas of the body like brain, Kidneys , Muscles, etc.
During operations, the heart-lung machine is usually a few meters away from the patient, operating table and surgeon, and is operated by a specially trained cardiac technician. This monitors the function of the heart-lung machine throughout the operation and changes its parameters in consultation with the surgeon and anesthetist (anesthetist).
Secondly, the heart-lung machine offers the anesthetist the opportunity Anesthetic gas to conduct into the blood, and so a relatively precise control of the anesthesia to achieve. There are extra devices and valves on the device.
Third, the filter function. In patients with terminal kidney failure a filtration can be carried out in the heart-lung machine, which works on the principle of a Dialysis machineso washes the blood. These are Filters and membranes interposed in the bloodstream. In a certain way, this is also necessary because plastic parts can always detach from the tubes, or blood clots from the vessels, and embolisms (i.e. blood clots) can form in the body. Of course, both the device and the tubing are subject to the highest medical demands and standards, but even microscopic particles are sufficient to lead to vascular occlusions. (For more information, see? Risks and side effects)
Also can undissolved gas bubbles filtered out of the circulating blood, so becomes one Air embolism, in which an air bubble collects in the vessels.
Fourth, in the heart-lung machine, blood can be added or diverted and stored. This is especially true with operations increased blood loss makes sense. In this way, the circulating volume can be reduced at the beginning of the operation and blood can be stored in a bag in the HLM. If there is later increased blood loss, this blood is supplied again, and if necessary by donated blood of the same blood type added.
How long do you have to be connected to the heart-lung machine?
How long you have to be connected to the heart-lung machine depends very much on which heart operation is being performed.
In general, it can be said that this time is kept as short as possible in order to avoid complications as well as possible.
At the beginning of the operation, the chest is opened and the heart is shown clearly. After the necessary preparations, the heart is connected to the heart-lung machine and then the heart is artificially brought to a standstill using a potassium-rich cardiopure solution. While the heart-lung machine takes over the function of the now silent heart, the operation on the heart can take place. Once all the steps in the operation have been carried out, the heart is stimulated again so that it beats independently and less blood is gradually passed through the heart-lung machine until it can be completely removed.
This procedure is roughly identical for most operations, so that the duration depends largely on the surgical method and can be very different. Periods of two to three hours on a heart-lung machine are considered safe, as no permanent damage remains to the heart during this time.
What is the maximum length of time you are connected to the heart-lung machine?
A heart-lung machine can take over the function of the patient's heart for several days. This is used when the heart cannot resume its entire pumping function after the surgical steps that have taken place.
Connecting to the heart-lung machine for several days supports the heart until it is fully functional again. Periods beyond this turn out to be problematic as they are associated with increasing side effect rates.
Maximum connection time after a heart attack
In addition to acute therapy, bypass surgery can be carried out in a later phase of a heart attack.
Such an operation is carried out when three coronary vessels distant from the trunk or two vessels near the trunk are partially or completely closed and this has led to symptoms such as a heart attack. The necessity of the heart-lung machine for this operation is discussed in more detail under “Maximum connection time for a bypass operation”.
Maximum connection time after bypass surgery
A bypass operation is performed when one of the coronary arteries is no longer sufficiently permeable so that the supply to the heart cannot be guaranteed. While a new artery or vein is sewn onto the heart and connected to the trunk of the coronary arteries, in classic surgery the heart is shut down and connected to a heart-lung machine. The entire operation takes about 4-8 hours, which is influenced by a wide variety of factors.
During this period, however, the heart is not connected to the heart-lung machine all the time, but only as long as the blood vessels are operated on. Newer minimally invasive surgical methods even get by without an artificial cardiac arrest and heart-lung machine. The section to be operated on is held in place with a U-shaped bracket and can be stabilized in such a way that an operation on the vessels is possible.
coma
The heart-lung machine represents a pure replacement cycle and cannot keep the body alive for a long time. This substitute is only sufficient for the basic functions of the body and is only used during anesthesia or an artificial coma. Coma or anesthesia are an integral part of therapy with a heart-lung machine. People are usually only awakened from the coma after normal body functions have resumed.
Contraindication
Emergencies that require a connection to the heart-lung machine often do not offer the time to evaluate the patient's medical history. The heart-lung machine is an extreme situation for the body, but it is often the only chance for those affected. Although the risk is significant, failure to do so can cost many people their lives.
The risk-benefit assessment, which also takes other pre-existing diseases and the general condition of the patient into account, must be carried out carefully during planned interventions.
Risks and Side Effects
An intervention on the heart in the natural one great intervention, and holds one Multitude of risks. In addition to the "usual" risks that arise during an operation, there is still the risk of using the heart-lung machine
of the Microembolization: Microscopic particles detach from the device or from the vessel wall, coagulate (i.e. clump), and clog the device, or Vessels in the patient. Therefore filters and anticoagulants are always used. The latter make the patient's blood more fluid and less prone to clumping, but also cause problems for the surgeon, since bleeding is logically more difficult to stop. So fine tuning is required here.
an oxygen deficiency. While the lungs with their billions of Alveoli provides a total area of almost 200m² for oxygenation of the blood, in a heart-lung machine it is only 2-10m² due to the design. The diffusion surface at which blood and oxygen come into contact is therefore much smaller, and the oxygenation function of the lungs is only incompletely replaced.
One Immune reaction. Since hoses and devices are foreign to the body, it reacts with an immune response to the supposedly harmful components in its circulation. Signal substances are released to combat it, which can lead to an inflammatory reaction and, in an emergency, even death.
- Of the Edema formation. Due to the pressure conditions between blood and tissue, more water flows from the vessels into the surrounding tissue - the blood thickens and the tissue swells. One speaks of Edema. After the operation, the patients are severely edematous and have a lot of water stored in their legs and arms. Only after completion of the operation can the body withdraw the water from the tissue and send it back into the blood - which suddenly forms too high a volume. So the kidneys have to excrete the excess water from the blood (similar to a dryer that flings wet clothing to draw the water out of it), which is especially true in patients with Renal failure is problematic.
Complications
Taking over the heart-lung function with the help of the heart-lung machine is a serious intervention in the body and can bring with it a multitude of complications. The blood is moved through the machine's artificial circuit and this material is completely different from natural blood vessels. If the blood is not diluted sufficiently with medication, thrombi can form. These thrombi can get stuck in smaller vessels and lead to strokes and other infarcts.
Furthermore, the blood components can change and certain components can become too few. These include, for example, the coagulation factors in the blood. The water and salt balance can also shift during therapy with the heart-lung machine and trigger life-threatening complications. In addition to the blood's own thrombi, air bubbles in the machine can also get into the blood and also trigger circulatory disorders. Kidney and lung function can also be impaired. The altered blood flow can also directly cause neurological damage from an insufficient supply of oxygen. The complications depend on the general condition of the person affected and the underlying disease.
You might also be interested in this topic: Air embolism
application areas
The heart-lung machine can be used in a variety of operations that require surgery on the heart. This includes Flap replacement (Mitral, aortic valve) , Heart transplants, Artificial heart installation,Bypasses, Heart defect corrections and Plastics of the large supplying and draining heart vessels. But also with one Lung transplant if necessary, a heart-lung machine is used.
costs
In the medical fee schedule, the use of a heart-lung machine is estimated at € 1,850 as the basic fee. The amount increases depending on the duration of the therapy. The treatment is fully covered by all statutory health insurance companies. A heart-lung machine is already an expensive machine to purchase which is only available in a few large clinics. In addition to medical supervision, there is always a technician on site who is familiar with the machine.
Miniaturized extracorporeal circulation (MECC)
This is a scaled-down version of the heart-lung machine with fewer side effects. Since the use of the HLM posed a number of risks, it was further developed and sought after less invasive, and less risky mechanism. By downsizing the device, the foreign body surface that comes into contact with the circulating blood has also been minimized, which reduces the risk of an immune response. The filling volume of the MECC system is only 500 ml (heart-lung machine with blood depot: over 2000 ml), which means that the volume red blood cells sinks less. MECC systems are also smaller and more portable, in contrast to heart-lung machines, which are roughly the size of a desk. The MECC was primarily developed for coronary bypass surgery, as this represents the majority of operations in which extracorporeal support systems are necessary. Through the Heparin coating of the device, the risk of blood clumping is reduced. Heparin is an active ingredient that thins blood and belongs to the class of anticoagulants. In summary, the MECC is a further developed, scaled-down form of the heart-lung machine, which is mainly used in Bypass surgery is used. Various risks could be reduced and the complication rate decreased.
history
The heart-lung machine was first used in 1937 by the American surgeon John Gibbon. He managed to divert the blood from the vena cava into an oxygenator and then to return the oxygen-rich blood to the patient. After many failures, on May 6, 1953, he succeeded in an operation on a patient Atrial septal defect. For a period of 26 minutes, the blood was passed through the heart-lung machine while Gibbon closed the hole between the two atrial chambers. His operation is considered formative and pioneering for the entire field of cardiac surgery.















.jpg)







-mit-ten-(titanic-elastic-nail)-oder-sten.jpg)
