Intubation
What is intubation?
Intubation is the term used to describe the introduction of a ventilation tube into the windpipe or the throat of a patient during an operation or in an emergency to secure the airways and breathing.
Various ventilation systems are available for intubation, which can be selected depending on the planned procedure and individually depending on the patient.
Read more on the topic: Intubation anesthesia

What is the correct procedure for intubation?
After the medication has been administered, the patient has to be ventilated because he is no longer able to do this himself due to the muscle relaxant administered. The head is overstretched and a mask is used for ventilation. Now the laryngoscope is carefully advanced and the tongue is pushed to the side. You should now be able to see the vocal folds and glottis. If this is not the case, you can get a better view with a pressure on the larynx or use a video laryngoscope. Now the tube is pushed along the laryngoscope between the two vocal folds into the glottis and blocked with a blocker syringe, i.e. the cuff on the tube is inflated so that it cannot slip. Now the stomach and lungs are monitored with a stethoscope to make sure that the tube is properly seated in the windpipe. In order to prevent the tube from moving, it is also secured with a fastening strap. A capnometer is then connected, which measures the CO2 in the exhaled air. If this cannot be measured, the tube is probably positioned incorrectly. If everything is correct, the tube is connected to the ventilator, on which the required parameters are then set.
You can find additional information at: Induction of anesthesia
What is intubation anesthesia?
Intubation anesthesia is a form of general anesthesia. Here, after the anesthetic medication has been administered, an endotracheal tube (a type of ventilation tube) is inserted into the patient's windpipe in order to ensure ventilation.
In the case of general anesthesia, in addition to hypnotics and painkillers, muscle relaxants are also used, the effect of which the patient can no longer breathe himself. It also makes it easier to insert the tube (intubation) through which breathing is controlled during the operation. Intubation anesthesia is required if local anesthesia is insufficient or the affected area cannot be anesthetized in this way, e.g. Operations in the chest and abdomen, on the heart, on the head, emergency interventions, etc. One advantage of intubation anesthesia is the secure airway. The tube is unlikely to result in aspiration, i.e. for foreign bodies or food residues to enter the airways. Disadvantages are the risk of injury to the teeth, larynx and trachea.
What is an e-mac intubation?
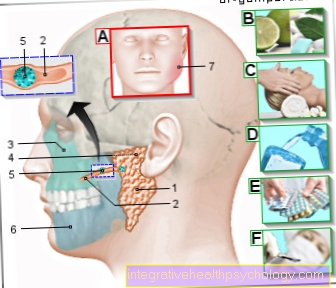
During intubation, the anesthetist places the tube between the vocal folds and then pushes it into the windpipe. This can only be done safely if the glottis is clearly visible. Therefore, a laryngoscope is used for insertion, with which one can push the tongue to the side and lift the lower jaw. However, it can still be the case that the glottis cannot be seen, e.g. in obese patients or chest deformities. A C-Mac video laryngoscope can help here.It has a built-in camera and an associated monitor, with the help of which one can see the glottis and insert the tube safely even in difficult patients. In addition to the intubation under visual control, the patient is monitored in order to rule out that the tube has accidentally entered the esophagus. In addition, a capnometer is connected, which measures the CO2 that flows through the tube during exhalation.
What does the intubation set include?
The intubation set consists of several parts and, in addition to intubation before an operating room in a hospital, is mainly used by the emergency services. It includes: endotracheal tubes of various sizes; a laryngoscope with a light spatula; Introductory stylet, which is inserted into the tube for intubation to make it more rigid and thus facilitate intubation; after successfully inserting the tube, the stylet is removed again; a blocker syringe with which the tube is blocked to prevent it from being easily torn out; Block clamp; Lubricant (e.g. gel) to make it easier to insert the tube; a fastening strap so that the tube cannot slip and a Guedel tube. The Guedel tube is used to fix the tongue of unconscious patients so that it cannot be swallowed and thus helps with mask ventilation. The intubation should always be performed by a doctor.
What medications are used during intubation?
Three different types of medication are used intravenously during intubation: a hypnotic (anesthetic), an opioid (pain reliever), and a muscle relaxant. First the opioid, e.g. Fentanyl. It suppresses the pain stimulus and has a slightly sedating effect on the patient. Then the hypnotic is given, e.g. Propofol. This leads to a loss of consciousness in the patient. Lastly, the muscle relaxant is administered, e.g. Rocuronium. The skeletal muscles become paralyzed and the patient now has to be ventilated and intubated. During the operation, the anesthesia is maintained by anesthetic gases or intravenous medication.
Read more about this under: What anesthetics are there?
What are the complications of intubation?
Complications during intubation are e.g. a misintubation in which the tube is inserted into the esophagus instead of the trachea. As a result, the patient is not ventilated and receives no oxygen. If the incorrect intubation is not recognized in time, the lack of oxygen can lead to permanent damage and even death. Complications in the form of damage to the tube can also occur during intubation into the trachea. Examples of this are a dislocation of the arytenoid cartilage in the larynx or other damage to the vocal cords, e.g. intubation granuloma, which can lead to hoarseness and difficulty breathing. Damage to the trachea (windpipe) is also possible. This can lead to a subglottic stenosis, which can make breathing difficult. Another complication is the injury or loss of teeth due to incorrect use of the laryngoscope. In long-term ventilated patients, the tube can injure the mucous membrane of the trachea and even necrosis.
You can find additional information at: The risks of general anesthesia
What is an intubation granuloma?
Intubation granuloma is a type of vocal cord granuloma, which can occur as a complication of long-term endotracheal intubation. It is a pseudotumor, i.e. a tumor that occupies space, but otherwise does not have the characteristics of a real tumor. Another example of a pseudotumor is warts. A vocal cord granuloma is usually preceded by an injury to the vocal cord. In the case of intubation granuloma, this is intubation. Symptoms are cough, hoarseness, a foreign body sensation, and difficulty breathing. The treatment is carried out by surgical removal of the granuloma, since the surgery injures the vocal fold again, and recurrences are not uncommon.
Can intubation cause epiglottitis?
Inflammation of the epiglottis (epiglottitis) is most common in young children, but in rare cases adolescents and adults can also be affected. Since sterile instruments and materials are used during intubation, this is unlikely to be the cause. There is a vaccination against the pathogen Haemophilus influenzae, which is also recommended for every child. Since epiglottitis has a fairly high mortality rate of 10-20%, it is important to administer antibiotics quickly. In an emergency, intubation must even be performed to secure the airways.
Read more on the subject at: Epiglottitis
Hoarseness after intubation
In the case of endotracheal intubation, a tube is placed in the windpipe to ensure ventilation of the patient. This can also cause various intubation damage. One of the most common complaints after awakening from anesthesia is hoarseness. However, this should go away again after one to two days after the operation. In some cases, e.g. by moving the tube, lead to additional irritation of the vocal cords, which makes the hoarseness last longer. Long-term intubation increases the chances of injuring the vocal cords and developing intubation granuloma, which in turn can cause hoarseness until it is removed. In rare cases, muscles and nerves that are responsible for moving the vocal folds can be injured during intubation. This can then lead to paralysis of the vocal folds and prolonged hoarseness. Basically, endotracheal intubation does not have to be performed for every procedure. If necessary, ask the anesthetist about possible alternatives.
Read more on the topic: Fear of anesthesia / general anesthesia
Laryngeal mask (LMA)
The laryngeal mask is a so-called oropharyngeal tube, i.e. that it comes to rest behind the larynx after being introduced through the patient's mouth.
This is to ensure that the airways are kept open so that the patient can then be ventilated through the mask.
The laryngeal mask is used when an operation does not last longer than two hours, another type of intubation was not possible or the patient needs emergency ventilation.
Before the laryngeal mask is inserted, the patient is put under anesthesia to avoid the gag reflex and larynx cramps.
It can then be inserted through the patient's mouth with the patient's head overstretched and fixed in the correct position.
Contraindications
It is important that the patient is sober, as inserting the mask behind the larynx can induce vomiting, which can result in aspiration of the vomit into the lungs.
In contrast to other intubation procedures, the laryngeal mask offers no protection from this.
In addition, the laryngeal mask is not suitable for very overweight people (BMI> 35), as well as interventions in the chest or head area.
Risks
Inserting the laryngeal mask can damage the tongue ligament and damage the teeth.
Read more on the topic: Laryngeal mask
Laryngeal tube (LTS)
The laryngeal tube is an alternative to the laryngeal mask.
In contrast to this, it offers a higher one Aspiration protectioni.e. he can better prevent vomiting from breathing in.
The laryngeal tube can also be used if other intubation proves difficult and can also be used for emergency ventilation be used.
After insertion, the laryngeal tube also comes to rest under the larynx, but it also has an opening in the esophagus flows out and over the one Nasogastric tube can be inserted for suction of stomach contents.
Despite this higher aspiration protection, the laryngeal tube should, if possible, not be used on non-fasting patients.
Risks
Even when the laryngeal tube is inserted, the tongue ligament or the oral mucosa can be injured.
If a tube that is too large is selected, ventilation may not be possible.
Guedel tube
The Guedel tube is like the laryngeal mask oropharyngeal Tube.
It is used to facilitate mask-bag ventilation. The Guedel tube is inserted through the mouth of the unconscious / anesthetized patient and comes to rest in the pharynx.
This prevents the airways from being obstructed, e.g. by a slack tongue.
The Guedel tube cannot be used in awake patients, otherwise it will be inserted Protective reflexes triggered that too Vomit and subsequent aspiration.
To choose the correct length, the distance between the corner of the mouth and the patient's earlobe is based.
Helical tube
The helical tube, like the Guedel tube, facilitates mask-bag ventilation.
However, he is a nasopharyngeal Tube, i.e. it is pushed through the patient's nose into the pharynx.
This means that it can also be used with awake patients. To select the correct length, use the distance between the tip of the nose and the patient's earlobe as a guide.
Endotracheal intubation
Endotracheal intubation is the procedure of choice Emergency interventions or not-sober Patient. It is used for operations on the head, neck, chest and abdomen.
In principle there are no contraindications, especially not in the case of emergency interventions.
With endotracheal intubation, a ventilation tube is inserted into the windpipe of the patient.
For women, tubes with a thickness of 7.0-7.5mm are used, for men, tubes with a thickness of 8.0-8.5mm are used. When intubating small children, the thickness of their little finger is used as a guide for the thickness of the tube to be selected.
Action
In advance, the patient is ventilated with a mask so that his blood is sufficiently enriched with oxygen. After giving one muscle relaxing Drug (Muscle relaxant) the so-called Laryngoscope Be pushed towards the larynx.
There is a camera on it, through which the anesthetist can see the larynx. With the laryngoscope the Epiglottis be raised until the view of the vocal cords given is.
The ventilation tube can then be inserted past the vocal cords into the windpipe and ventilation can begin. A bite guard can be used retrospectively so that the patient does not accidentally bite the tube. The tube is then fixed to the mouth with plaster strips.
Complications
Due to certain anatomical conditions, in some patients the vocal cords are not easily visible. In such a case, an attempt is first made to improve the visibility by carefully pressing the larynx up and right.
This procedure is called BURP maneuver (English: backward, upward, rightward pressure). If intubation is still not possible, alternative methods may have to be used.
Fiberoptic awake intubation
The fiberoptic awake intubation is the method of choice for difficult intubation conditions.
There is also a flexible Bronchoscope available that can be inserted into the trachea when the patient is awake with protective reflexes preserved.
As a result, the patient's spontaneous breathing is maintained.
Since the procedure can be very uncomfortable for the patient, it is important that the mucous membranes are sufficiently in advance stunned become.
Then the bronchoscope with the threaded tube can be pushed through the nose or mouth up to the entrance of the larynx.
The bronchoscope has an additional opening through which anesthetic can be applied to the vocal folds.
Once this has been done, the tube can be inserted further into the windpipe. Only when the tube has been securely placed in the windpipe is anesthesia initiated.
Cricothyrotomy
The cricothyrotomy is the last resort to secure ventilation for a patient. It is only used for so-called "cannot intubate, cannot ventilate"Cases applied, i.e. in patients who cannot be ventilated either with a mask or with conventional intubation.
This is an emergency as the patient is otherwise at risk of suffocation.
The cricothyrotomy is a surgically invasive procedure in which the ligamentum conium (therefore the name), a ligament between the cartilage parts of the larynx, is opened from the outside with an approximately 3cm long incision.
A ventilation tube can then be introduced through the opening, via which the patient's oxygen supply is ensured. However, this procedure is only used to bypass the oxygen supply in emergency situations.
As soon as the situation permits, an alternative intubation procedure should be switched to.
Read more on the subject at: Tracheal incision
























.jpg)