Germs
introduction
We encounter germs in our everyday life without us noticing. Only when we get sick do we feel the effects of the various pathogens. In addition to bacteria and viruses, germs also include fungi, parasites and algae. Most types of germs can be divided into subgroups.
Often one group of a germ is part of the natural flora of our skin and mucous membranes (e.g. in the nose, mouth or intestine), while another group has disease-causing properties.
Microorganisms that live in and on the human body but do not cause it any damage are called commensals. In contrast to the commensals, parasites always cause damage to the body, so they are pathogenic germs.

Germs in the mouth
Under normal circumstances, the mucous membrane in the mouth is colonized with a variety of germs. Bacteria are most common there. In terms of quantity, the streptococci and the staphylococci stand out among these. Cocci are rounded structures that cluster together in piles, chains or pairs and are therefore easy to identify under the microscope.
On the one hand, staphylococci are normal skin germs, but they can also be involved in wound infections, depending on which subgroup of the germ is predominant. Streptococci can also be divided into several subspecies, they are then responsible for infectious diseases such as scarlet fever and angina (Streptococcus pyogenes) or pneumonia (Streptococcus pneumoniae, formerly "pneumococci").
Actinomycetes, rod-shaped germs that can live without atmospheric oxygen, also occur in the mouth and can contribute to the development of tooth decay. Germs that cause tooth decay are called cariogenic.Caries is caused by streptococci or actinomycetes, the most common being streptococci in the form of the pathogen Streptococcus mutans.
Furthermore, the mouth forms a gateway for a wide variety of germs. Contaminated food allows germs to get into the digestive tract and tiny droplets in the air can penetrate the respiratory tract. Oral (in the mouth) pathogens can even cause inflammation of the inner lining of the heart (endocarditis) in the heart. If left untreated, such heart inflammation leads to death. Germs in the mouth consequently lead to diseases of the entire body. Dental and oral hygiene as well as regular check-ups at the dentist should therefore not be neglected.
Germs in the nose
Moisture and warmth. In the nose there are optimal conditions for germs, which therefore mainly settle there. Bacteria such as staphylococci and rod-shaped bacteria belong to the normal skin and mucous membrane germs of the nose. Other germs, such as the pathogen Haemophilus, are also part of the healthy nasal mucosa, but some species of the germ are able to Inflammation of the meninges (meningitis) trigger. Haemophilus has the peculiarity, only in the presence of a certain germ (Staphylococcus aureus) to grow. Staphylococcus aureus causes wound infections and boil, but at the same time offers the Haemophilus nutrients so that Haemophilus can grow in the first place. This phenomenon is referred to as the “wet nurse phenomenon” because Staphylococcus aureus “takes care” of the Haemophilus like a “wet nurse”.
There are also Pneumococci, the causative agents of pneumonia, in low numbers in the upper respiratory tract. Symptoms that occur in the nose due to bacteria primarily affect the respiratory tract, as the microorganisms transmitted by droplet infection find their way into the nose when inhaled. Next Laryngitis and pneumonia play too sniff (caused by viruses) and the flu (also triggered by viruses) play an important role. Viral But pathogens belong Not to the common parts of the human body.
Germs in the lungs
Germs are able to cause great damage in the lungs. The resulting diseases are often severe or fatal. Most prominent examples of lung diseases caused by microorganisms are the pulmonary plague and the tuberculosis. Yersinia pestis, rod-shaped bacteria that caused a plague epidemic in the Middle Ages, are pathogens spread by rodents. The plague is one of the animal-borne diseases (Zoonoses).
When they are absorbed by droplets, pathogens enter the lungs via the respiratory tract, then the disease manifests itself as a cough with bloody, highly contagious sputum. If left untreated, pneumonic plague is fatal in over 90% of cases, and nowadays the disease is through Antibiotics almost exterminated, humans rarely become infected through contact with animals.
In contrast to the plague, tuberculosis is caused by so-called Mycobacteria triggered. Under the influence of oxygen These rod-shaped bacteria grow particularly well, which is why they are usually found in the respiratory tract and thus also in the lungs. Symptoms of tuberculosis are easy with those of one flu to be confused. Patients often feel dull and exhausted, but have only a slightly elevated temperature or almost no symptoms. After the symptoms of the "Primary tuberculosis"There is a possibility that the pathogen will survive unnoticed in the body for years until the outbreak of the"Secondary tuberculosis" With Coughing up blood (hemoptysis) comes.
In addition to bacterial infections, they also form Fungal infections in the lungs when the corresponding germs get there. Pulmonary mycosis (Lung fungi) are often seen by farmers (especially found in America), as they come into contact with the fungal spores while working in the fields and inhale them. In the lungs, the fungal spores then cause pneumonia, respiratory problems (e.g. coughing) and sometimes even spread to other organs (e.g. liver / spleen). Fungal infections are treated with agents that hinder the growth of the fungi (Antifungal drugs).
Germs in the bladder and urine

The urogenital system (kidneys, ureters, bladder) is responsible for the return of water and salts into the body, but at the same time also for the excretion of the urine formed. Urine is a filtrate from blood plasma, so it is also similar in its composition. In and of itself, human urine does not contain any germs. If microorganisms are found in the urine, this indicates a disease of the urinary tract, such as a bladder infection. Triggering bacteria from the genera of the Pseudomonas (rod bacteria) or the staphylococci (mostly heap cocci) migrate from the outside to the inside of the bladder via the urethra and multiply there, which leads to an inflammatory reaction.
This manifests itself as a burning sensation and pain when urinating as well as the feeling of an overcrowded bladder with a constant need to urinate. Young, sexually active women in particular are affected by bladder infections, as the corresponding germs from the external genital area and the rectal area are carried into the urethra during sexual intercourse. With 3-4 centimeters, women have a much shorter urethra than men (up to 25 centimeters), so the transmission path is also many times shorter. If a bladder infection is left untreated, the bacteria that cause it can spread to the kidneys via the ureters and cause inflammation of the kidneys (pyelonephritis) with pain-sensitive kidneys.
The bacterium Escherichia coli (E. coli) causes particularly stubborn urinary tract infections, as this rod bacterium multiplies quickly and under adverse conditions and treatment with antibiotics does not always work. In general, germs that are in the bladder and cause inflammation there are always excreted in the urine. The most important diagnostic measure in the event of a suspected urinary tract infection is therefore the examination of a given urine sample. The central stream of the morning urine is used for this, then a small amount of urine is placed on an incubation plate and incubated in the heating cabinet for a certain period of time. The doctor then uses the colonies that have grown on the plate to identify which germs are in the urine and which therapy must be used.
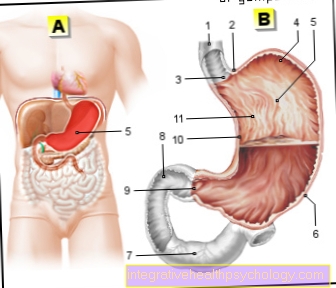
Germs in the intestines
The Intestines contains by far most of the germs in the human body. Almost all types are represented, staphylococci, enterococci, clostridia or rod bacteria and enterobactericae. The various microorganisms of the intestine play an important role both in the digestion of food and the associated absorption of it Vitamins and nutrients but also the formation of intestinal gases, which can become symptomatic as gas (flatulence).
Please also read our article on this Bacteria in the gut.
Despite their usefulness in digestive health, many of the bacteria make you sick if their numbers increase too much. The best example of this is the bacterium Escherichia Coli, a rod-shaped intestinal bacterium. If the number of bacteria present increases above normal levels, it comes to Diarrhea and one Inflammation of the stomach and intestines (gastroenteritis) with nausea and vomiting.
Such symptoms can also be caused by ingesting spoiled food (e.g. meat, especially poultry or raw eggs). In the case of food poisoning, the causative agent is usually the Staphylococcus aureus. The bacterium produces poisons (toxins) that develop their effect in the gastrointestinal tract (enterotoxins). They have a similar effect Salmonella out. They are also found in spoiled foods, such as raw eggs. Food poisoning are characterized by a short but violent course. Other pathogens, on the other hand, are responsible for the development of entire epidemics. The prime example of such an epidemic is choleracaused by Vibrio cholerae, a bacterium that still kills many people, especially children, in developing countries.
Not only bacteria cause diarrhea and vomiting, many Viruses are also able to do this. To be mentioned here are the adeno, rota and Noroviruses. The most famous virus is that Norovirus. Public institutions such as schools, kindergartens or care facilities have to close again and again because the children have become infected with the norovirus. Again, diarrhea and vomiting are the main symptoms of infectious diseases.
Germs in the blood
As a result of an infectious disease, a sepsis (Blood poisoning) occur. This happens when germs from a local focus (e.g. clostridia in the intestine) enter the blood flow and the inflammatory reaction triggered by the pathogen spreads to the whole body. Possibly (depending on the type of pathogen) poisons (toxins) are also involved in the damage to the body in the course of sepsis.
Cell damage and the death of cells lead to inflammatory reactions in the body and the release of inflammation-dependent messenger substances. In addition to the detection of the causative germ, the other symptoms of sepsis are quite clearly defined. fever over 38 degrees, rapid breathing (tachypnea), high heart rate (tachycardia) and increased Inflammation values in the blood play the main role here.
If sepsis is left untreated, the infection spreads to the organs, and many patients subsequently die from multiple organ failure. In order to be able to treat sepsis effectively, the causative agent must be known exactly.
The creation of blood cultures in the laboratory is essential for this, therapy is then carried out depending on the pathogen. Since sepsis is bacterial in many cases (rarely caused by fungi), an appropriate dose is available Antibiotic first of all.
Germs in drinking water
Many people in this country only know contaminated drinking water from television. In developing countries, however, unclean water is a real problem. Inadequate sewage systems and the lack of sewage treatment plants mean that rubbish or human waste often ends up in the water that is actually intended to be used as drinking water. If these countries also have a warm climate, nothing stands in the way of germs growing.
There are outbreaks of cholera or other illnesses associated with diarrhea. The consequences are high child and infant mortality rates. Bacteria that spread in unclean water are, in addition to Vibrio cholerae, salmonella, Pseudomonas aeruginosa or Escherichia coli. Viral representatives are noro-, adeno or astroviruses. Germs of the type are particularly persistent Legionella. They not only occur in unclean waters, but are also partly present in Europe in the pipes of older houses and thus cause a stir again and again.
Legionella belong to the genus of rod bacteria, in humans they solve the "Legionnaires' disease" out. The tricky thing about this disease is that it is only triggered by inhaling pathogens. Legionella therefore often spread in warm water sources, namely where steam is generated and the bacteria can penetrate the respiratory system. Symptoms of Legionnaires' Disease are first and foremost Pneumonia. The diagnosis includes the creation of different cultures from blood and urine, the therapy is based on the administration of macrolide antibiotics. Elderly people with underlying diseases and people with a weakened immune system (chemotherapy patients) are at risk, as they often die of pneumonia.
Germs in the hospital
Hospital infections (nosocomial infections) have increased sharply in recent years. The mostly careless use of antibiotics is also to blame for this development. Some types of bacteria have gotten used to the antibiotics that are supposed to kill them when they emerge multi-resistant pathogens, which can hardly be dealt with with conventional antibiotics (broad spectrum antibiotics).
Then come Reserve preparations used, but unfortunately there are already some strains of pathogens where the reserve antibiotics are no longer able to do anything. Germs are dangerous in hospitals with open wounds, with diarrhea diseases and for people with weakened immune system (e.g. after a chemotherapy). Wound infections and wound healing disorders are often caused by the methicillin-resistant Staphylococcus aureus (MRSA) caused. Patients found to have MRSA must be isolated in a single room and medical personnel may only enter the room in protective clothing.
The same applies to infections with resistant Escherichia Coli bacteria. The intestinal dwellers cause opportunistic Infections. An opportunistic infection is an infection with bacteria that are normally found in the body and do not harm it, but if the immune system is weakened Cause diseases. Infections with Escherichia Coli lead to diarrhea and can cause considerable damage to people whose immune systems are already weakened. In hospitals, special measures apply to outbreaks of infections caused by germs. Sick patients are often forbidden to visit, are isolated in single rooms and the medical staff must pay particular attention to the prescribed hygiene measures and also document them. Only when the patient is confirmed to be germ-free by laboratory diagnostic procedures, such as the creation of colonies of blood, urine or stool, are these measures lifted again.