Kneecap jumped out
Synonyms
Kneecap fracture, Patellar fracture, pneural disc tendon, patellar tendon, patellar tendon, chondropathia patellae, retropatellar arthrosis, patellar dislocation, kneecap dislocation
Medical: patella
English: patella
introduction
This topic is a continuation of the kneecap topic.
You can find more information on the subject of the kneecap jumped out under Kneecap Dislocation

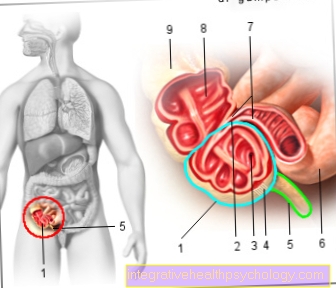
Figure kneecap

- Kneecap -
patella - Femur -
Femur - Shin -
Tibia - Fibula -
Fibula - Inner meniscus -
Meniscus medialis - Outer meniscus -
Lateral meniscus - Kneecap ligament -
Ligamentum patellae - Hamstring muscle -
Rectus femoris muscle - Iliac-tibial tendon -
Iliotibial band - Tibia anterior muscle -
Tibialis anterior muscle
You can find an overview of all Dr-Gumpert images at: medical illustrations
Knocked kneecap
The Kneecap is a V-shaped bone in front of the knee joint. It is embedded in the tendon of the thigh muscles, which enable stretching and which pull from the thigh over the knee to the lower leg. On the knee side it is in a so-called bearings of the thigh bone, the shape of which is ideally adapted to the kneecap. Due to its special shape, the kneecap (patella) to transfer the pull of the thigh muscles while protecting the knee joint to the lower leg and thus a maximum Elongation to allow in the knee.
The doctor describes the condition of a popped kneecap as Kneecap or patellar luxation or Kneecap or patellar dislocation. Such a dislocation of the kneecap is relatively common, although two basic mechanisms by which it can arise must be distinguished.
For one thing, there is traumatickneecap dislocations caused by an accident (which are mainly found in adolescents), on the other hand there is the type that is conditioned by the patient and occurs without a special preceding event (habitual). On average are Women affected somewhat more often by this second form, men somewhat more frequently by the first.
Factors that are believed to contribute to the development of habitual kneecap dislocation include the following:
- a little pronounced Knee bearing,
- a faulty system the kneecap itself (Patella dysplasia),
- a Patellar high (mostly due to an accident),
- a too straight trained kneecap,
- a general Connective tissue weakness,
- Knock knees (Genu valgum),
- if the thigh muscle tendon attaches too far to the outside of the lower leg,
- incorrect installation of the gliding groove of the kneecap (Trochlear dysplasia)
- a displacement of the patella for Opposite side.
If one of these factors or even a combination of several of the above is present, it is easy for the kneecap to pop out, even if it is not subjected to excessive stress or is involved in an accident.
In contrast, traumatic patellar dislocation requires prior to an accident with a considerable violence have come. This is particularly common in the context of sporting activities before when the athlete is stretched leg experiences a kick in the knee if he has not tensed the thigh muscles or only slightly. For example, she comes very often Footballers in front.
In general, the kneecap almost always slides outward through its slide rail and the Tapes on the inside of the knee tear. As a result, the kneecap is too far out on the knee, and the joint looks in a very typical way deformed out. Regardless of the cause, however, the symptoms and treatment options for the popped kneecap are almost the same.

First of all, this has the tendency spontaneous jump back to their original position as soon as the victim extends their leg. The injury is extreme painful. This pain is usually greatest below the knee and on the inside of the kneecap, as this is where the ligaments have been damaged. Often one forms shortly after the event massive swelling of the knee joint by one Joint effusion, which comes about because the ligament is injured Bleeding leads. The pain and swelling also cause a Restriction of movement in the knee joint. Injured people tend to keep the leg in a slightly flexed position, as this is the least painful. In some cases, in addition to the dislocation of the patella, it also breaks off small fragments of cartilage or bonethat can become trapped anywhere in the joint and make the pain worse. These can later be added to Cartilage damage and / or one arthrosis of the knee joint.
In order to diagnose a dislocation of the kneecap, apart from the detailed taking of the medical history (anamnesis) and the physical examination, one must be prepared X-ray image of great importance. Here you can see the dislocation well and also identify any existing risk factors. In addition, a Jointoscopy (Arthroscopy), because you can not only get a closer look at the situation in the joint, but also fix parts of the problem directly by doing a Joint irrigation and small pieces of cartilage or bone are removed.
An even more precise assessment offers a Magnetic resonance imaging (Magnetic resonance tomography, MRT), which, however, is not one of the standard procedures in primary diagnostics due to the large amount of time and cost involved.
Successful treatment of the Kneecap dislocation is of the utmost importance. If this does not jump back into its correct position on its own (self-repositioning), which luckily it usually does, a doctor or an experienced sports trainer must do this.
Thereafter, therapy must take place, depending on the cause of the dislocation, the extent of the injury and the individual circumstances of the person concerned (such as the risk profile, age, sporting activities and personal wishes). In some cases she can come in conservative with the help of rails, Bandages and physical therapy while in other cases one of a variety of operational procedures must be used.
Successful treatment is of such immense importance as long-term complications may otherwise arise and the kneecap may persist instability otherwise often tends to pop out again and again. While with an early treatment still about 80% the patient can be put back into a state of perfect health, this is only possible to a certain extent after multiple dislocations 20%. The urgency of treatment becomes more than clear.















-de-quervain.jpg)