Pulmonary embolism
Synonyms in a broader sense
Pulmonary infarction, pulmonary embolism, pulmonary embolism; Pulmonary artery embolism, lungs
English: pulmonary embolism
Definition pulmonary embolism
A pulmonary embolism results from a blood clot that is washed away (thrombosis) that clogs a pulmonary artery. This will increase the proportion of lung No longer supplied with blood behind the embolus (clogging plug).
The result is that the remaining blood vessels (arteries) have to compensate for the blood flow in the blocked vessel. As a result, blood pressure rises in the Pulmonary circulation. Is the Blood pressure increased in the pulmonary circulation over a long period of time, there is a risk of cardiac overload with life-threatening cardiac arrhythmias.

Frequency (epidemiology)
Occurrence in the population
In line with the incidence of pulmonary embolisms in women, women are also predominantly affected by pulmonary embolism.
In Germany approx. 20,000 - 40,000 fatal pulmonary embolisms registered.
In about 50% of all cases, if a thrombosis is present, a pulmonary embolism can also be medically proven. However, only a fraction of all emboli are noticed by the patient.
Causes of Pulmonary Embolism
Pulmonary embolism is caused by a thrombus (Clot made from blood components), which is usually washed into the pulmonary vessels from the body's large circulation and relocates them. The risk of developing a thrombus is not the same for all people - as for many other diseases, there are special risk factors and protective factors that promote or prevent the formation of a thrombus.
Much of the thrombi that cause pulmonary embolism comes from the deep veins in the legs. Thrombi form here, among other things. during long phases of not moving (please refer: Thrombosis in the leg).
The fact that someone does not move for a long period of time can occur in the course of an accident in which there are fractures and injuries in and on the legs, which mean that the patient has to lie in bed for a long time.
Read more on the topic: Burning in the legs
Another risk factor lies in prostheses on the knees, hips and other joints, since damage to blood vessels cannot be avoided here either. Thrombi can form more easily on the damage. In addition, patients after prostheses are often not able to move fully - that is why one goal of surgery is to get operated patients on their feet as quickly as possible in order to minimize the lying time and thus the risk of thrombus formation.
In addition to operations on the joints, the risk is generally increased after operations of any kind.
Another group of risk factors are genetic pathologies (unnatural expressions of genes), e.g. the Factor V Leiden mutation.
There is also an increased risk of pulmonary embolism during pregnancy. Young girls and women who use the pill also have a higher risk of developing a thrombosis and thus a pulmonary embolism. Read more on the subject at: Thrombosis risk of the pill
If there are further disorders in the hormonal or metabolic balance, it must be noted that thrombus formation is also favored here.
Smoking and obesity are not to be despised as risk factors for pulmonary embolism.
Another very relevant risk factor is immobilization of the legs during long trips. The problem here is that the blood no longer circulates properly and therefore stagnates in the legs (stasis). Should you know you are planning a long journey (e.g. Air travel), it is especially advisable for patients with other risk factors (as described above) to have a one-time heparin injection at the family doctor. This reduces blood clotting over the following days and thus the risk of developing a thrombus.
If there are known cases of thrombosis and pulmonary embolism in the family, a doctor should discuss the extent to which the patient himself has any risk factors and whether prophylactic measures must be taken.
Read more on the topic:
- Causes of Pulmonary Embolism
Emergence
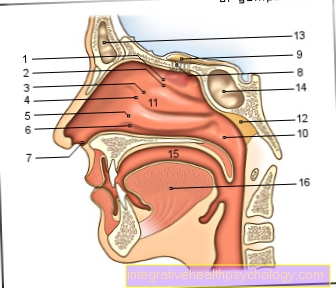
In most cases, the starting point of a pulmonary embolism is a thrombosis of the lower leg vein thrombosis (Leg vein thrombosis, approx. 60%) or Pelvic vein thrombosis (about 30%). In the early phase of thrombosis development, a thrombus is unstable and can tear itself away from the vein wall. This torn piece, which is medically known as an embolus, now swims back to the heart via the bloodstream and from there it is pumped into the lungs. There the vessels narrow again and the embolus clogs the vessel and the pulmonary bloodstream behind it.
Pulmonary embolism from flying
According to today's view, flying increases that risk for leg vein thrombosis and pulmonary embolism. The reason for this is on the one hand the longer sitting, on the other hand the lower air pressure slightly increases blood clotting. The longer the flight, the higher the risk of thrombosis occurring. In particular, people with multiple previous illnesses and the resulting increased risk of thrombosis should ensure that they get up regularly during flights and activate the leg muscles through various exercises. Also Compression stockings and compression bandages greatly reduce the risk of leg vein thrombosis and pulmonary embolism during flights.
Pulmonary embolism after surgery
Surgery increases the risk of deep vein thrombosis and pulmonary embolism. The risk of this depends mainly on the length of the operation and the subsequent restricted mobility. To reduce the risk, usually before and after an operation Heparin given in the form of infusions or abdominal injections.
Pulmonary embolisms are rare after short operations without any subsequent restriction of movement.
After major operations and a ban on standing up after the operation, leg vein thromboses and pulmonary embolisms are relatively common despite the administration of heparin. As a rule, however, a serious pulmonary embolism is diagnosed and treated in good time through a stay in the clinic and good monitoring, so that consequential damage is rare.
Pulmonary embolism after chemotherapy
Chemotherapy can increase the risk of pulmonary embolism and leg vein thrombosis because the blood is more prone to thrombosis. However, this depends very much on the drug used. For example, increase Lenalidomide- or Thalidomide-containing chemotherapies the risk mostly clearly and should therefore always be avoided from therapy with heparin to be accompanied.
Other agents, however, have little or no effect on the risk of thrombosis. It should be borne in mind that the underlying cancer usually also increases the risk of pulmonary embolism and accordingly the chemotherapeutic agent does not have to be the cause of a pulmonary embolism.
Pulmonary embolism from the pill
Anyone who uses the pill for contraception should know that most pills increase the risk of thrombosis and thus the risk of pulmonary embolism.
The active ingredients used in pills are estrogens and gestagens. Combination preparations are most frequently prescribed in Germany. The risk of thrombosis changes from drug to drug, depending on which dose of the respective active ingredient is used and which progestin the pill contains. Combination preparations with a high dose of estrogen and gestagens of the 3rd or 4th generation increase the risk by up to five-fold, while pure progestin preparations hardly influence the risk of thrombosis.
In combination with other risk factors such as smoking, the risk of thrombosis can increase significantly more.
Pulmonary embolism from smoking
Smoking not only increases the risk of various lung diseases, it also increases that Risk of thrombosis clear. This also significantly increases the likelihood of pulmonary embolism in smokers. The reason for this is that smoking changes the composition of the blood and its flow properties and causes vascular damage.
In particular, taking the pill at the same time significantly increases the risk of pulmonary embolism and leg vein thrombosis, which is why one of the two must be avoided.
If you quit smoking, the risk of thrombosis normalizes again after weeks to months.
Risk factors
As the cause of a pulmonary embolism in most cases a Thrombosis in the leg (rarely air, fat or foreign bodies), the risk factors for pulmonary embolism and thrombosis apply equally:
- Operations (esp. artificial hip joint and artificial knee joint)
- Obesity
- Smoke
- Gender (women> men)
- Sedentary lifestyle (long-distance flights = economy class syndrome)
- Childbirth
- Varicose veins (Varicosis)
- Blood disorders (leukemia)
- Heart disease (esp. Atrial fibrillation)
- Medicines (esp. Oral contraceptives ("pill”))
- Tumor diseases (e.g. prostate cancer or Pancreatic cancer)
- Hereditary diseases
- The APC resistance ("Factor V Leiden mutation") is the most common hereditary disease that is associated with a risk of thrombosis. The risk of thrombosis is 7-100 times higher (depending on heredity).
- Antithrombin III deficiency (AT III) mostly affects younger patients
- Protein C and Protein S - deficiency *
If these anticoagulant factors are reduced due to a congenital deficiency, thrombosis can occur in adolescence. - Hyperhomocysteinemia is an inherited impaired degradation ability of homocysteine with greatly increased homocysteine levels in the blood. Consequences include an increased risk of thrombosis.
All of the hereditary diseases mentioned can be diagnosed through blood tests.
- Diseases of the liver with impaired formation of coagulation factors (e.g. Cirrhosis of the liver)
Course of a pulmonary embolism
A pulmonary embolism usually has its origin in a thrombus (blood clot) that is located in a deep vein in the leg. Before this thrombus dissolves completely and triggers an acutely life-threatening pulmonary embolism, smaller blood clots are usually torn away from the thrombus. They cause tiny embolisms in the lungs, which are therefore very rarely discovered.
Symptoms such as decreased resilience, shortness of breath, coughing and dizziness can occur even with the small embolisms and should therefore be taken seriously. If the thrombus loosens completely, it usually closes a large lung vessel. This leads to sudden chest pain and shortness of breath. In addition, the affected person can suffer a shock, which is expressed by a greatly increased pulse. In this case, immediate medical attention is needed. Even with therapy initiated quickly, it is possible that pulmonary embolism will also damage the heart.
Due to the blockage of the pulmonary vessels, the heart has to pump against an extremely high pressure. However, due to the often present lack of oxygen, it is unable to do this and can decompensate (it cannot do the necessary additional work). This decompensation, which usually takes place in the right half of the heart, can cause permanent cardiac insufficiency (heart failure), which is associated with a greatly increased mortality (death rate).
Symptoms / complaints
There are no symptoms that are unequivocally or unequivocally indicative of a pulmonary embolism.
Symptoms can be:
- Racing heart
- Shortness of breath
- Chest pain, especially when you breathe in
- sudden sweat
- to cough
- fever
- Anxiety (more under: Pressure in the chest- these are the causes)
- sudden loss of consciousness
Many pulmonary embolisms, especially smaller ones, have no symptoms and can only be detected with special examinations.
Read more about Pulmonary Embolism Symptoms
First signs of a pulmonary embolism
How a pulmonary embolism manifests itself depends on various factors. These include, among other things, the size of the clot and the affected part of the lung, the remaining blood supply to the affected part of the lung, the age and previous illnesses of those affected. A small pulmonary embolism can go completely unnoticed, especially in otherwise healthy people. The typical symptoms of major pulmonary embolism are one sudden breathlessness and an associated increase in breathing and heart rates.
These symptoms usually appear from one moment to the next. Often one goes with it great fear which can develop into fear of death. A breath-dependent, developing relatively quickly pain In the affected lung segment or below the diaphragm, about 2/3 of the patients are described with larger embolisms.
Another common sign of a pulmonary embolism is to cough. Due to the death of lung tissue, the cough can also contain blood.
If the heart's performance is so severely impaired by the embolism that not enough blood is pumped through the body's circulation, kick Circulatory problems with sweats, tremors and possibly loss of consciousness.
Due to the combination of a lack of oxygen and cardiac overload, major pulmonary embolisms are life-threatening and can quickly lead to death if no therapy is initiated. The majority of severe and fatal pulmonary embolisms are intermittent. In the course of small pulmonary embolisms, dizziness, fainting attacks and palpitations occur again and again for hours or days. If the symptoms are interpreted correctly, a major pulmonary embolism can usually be prevented.
What can be typical signs of a pulmonary embolism?
Pulmonary embolism is often difficult to recognize because its symptoms are extremely unspecific and rarely all occur together. The main signs are shortness of breath and chest pain. These usually occur suddenly when the embolism becomes lodged in a pulmonary vessel. In addition to shortness of breath, so-called cyanosis can occur. This is expressed by the blue of the mucous membranes (especially lips) and possibly the fingers and comes about due to a lack of oxygen.
The lack of oxygen caused by an embolism can also damage the heart. A pulmonary embolism can also increase blood pressure in the pulmonary vessels. On the other hand, the heart has to pump more intensely, which is why it also uses more oxygen. The combination can lead to heart failure, increased heart rate and a drop in blood pressure. The combination of a drop in blood pressure and an increase in heart rate indicates a state of shock and can also trigger dizziness and sweating. Particularly unspecific signs can also be a dry cough or even coughing up blood.
Pulmonary embolism and pain
Pulmonary embolism may, but is, pain not very characteristic and usually not the main symptom. Its exact cause is not yet fully understood.
Usually occurs at the beginning Pain behind the sternum that can be mistaken for a heart attack. Over the course of days, the irritation of the lung membranes usually results in a different type of pain, the intensity of which depends on the breathing.
If pneumonia occurs, the pain may worsen. It is important that other causes should also be considered and clarified if the pain persists.
Can back pain be a symptom of pulmonary embolism?
Back pain are one of the possible symptoms of a pulmonary embolism. Mostly they occur in the area of the middle to upper back where the pulmonary embolism irritates the lung membranes and can lead to pain.
The back pain usually does not appear separately but is accompanied by other symptoms such as shortness of breath or one lung infection accompanied. They occur relatively quickly and change their character within the next few days, so that the pain usually feels different as it progresses. They often get stronger with inhalation and / or exhalation and should improve significantly after the administration of painkillers.
Cough as a symptom of pulmonary embolism
Coughing is a common, albeit very unspecific, symptom of pulmonary embolism. Especially smaller, otherwise inconspicuous embolisms are expressed in a dry cough. With larger embolisms, a bloody cough can also occur. On the one hand, the cough comes about because the stuck blood clot directly irritates the lungs. In addition, there is a reduced blood flow in the area behind the blocked vessel. This can cause inflammation in the area, which also causes a cough. In the worst case, it can even cause pneumonia.
Fever as a symptom of pulmonary embolism
Fever is a known complication of pulmonary embolism. It usually does not occur immediately at the same time as the embolism. Instead, it makes itself felt some time later. The trigger for this is in most cases what is known as infarct pneumonia, i.e. pneumonia that occurs after a pulmonary infarction. A heart attack describes a situation in which the tissue is not supplied with enough blood and as a result suffers from a lack of oxygen and nutrients. This is triggered by a blood clot in the lungs. The undersupplied area is also called the infarct area. Due to the insufficient supply, inflammation can settle there, leading to symptoms such as fever.
Night sweats as a symptom of pulmonary embolism
Night sweats are an extremely unspecific symptom, but in most cases this should be taken very seriously. Real night sweats are when someone sweats so badly at night that their pajamas and bed linen have to be changed. In the case of a pulmonary embolism, there are two possible triggers for night sweats: On the one hand, the embolism can subsequently trigger pneumonia, which is accompanied by fever and chills. Older people in particular often do not have a fever, instead they suffer from night sweats. The heart failure caused by the pulmonary embolism can also cause night sweats.
Are there any unnoticed pulmonary embolisms?
In particular, clots that only close small vessels and are then quickly broken down by the body can completely unnoticed stay or cause only mild discomfort. Those affected often attribute these to other causes.
Taken in isolation, pulmonary embolism is unnoticed or just minor not very dangerous - The tricky thing, however, is that you are often followed by other pulmonary embolisms, which are larger and can be life-threatening. Therefore should pulmonary embolism be suspected always consulted a doctor become. It is assumed that around half of all pulmonary embolisms go unnoticed.
Diagnosis of pulmonary embolism

- EKG
- Doppler sonography of the heart
- Pressure measurement in the pulmonary circulation
- Perfusion scintigraphy of the lungs with technetium-labeled albumin aggregates
- Pulmonary angiography (visualization of the pulmonary vessels)
- Spiral CT
- Digital Subtarction Angiography (DSA)
How can you recognize a pulmonary embolism?
A pulmonary embolism presents itself differently from case to case and also depends on the size of the vessels that are blocked.
Patients who present themselves have mild to severe breathing difficulties up to shortness of breath.
Other signs of a pulmonary embolism may include a new cough, Chest pain, dizziness, Anxiety with sweating, such as Circulatory failure be.
An irregular heartbeat (Cardiac arrhythmia) can also be an indication of a pulmonary embolism. If a leg is new or recently swollen, reddened, painful and overheated, it can be a Leg vein thrombosis which, in conjunction with the other symptoms described above, may indicate pulmonary embolism.
Upon admission, a simple questionnaire den Wells Scoreby asking standardized questions about how great the risk of pulmonary embolism is.
Furthermore, a blood sample can increase the D dimers (Fission products from coagulation) a suspicion can be reinforced. By a CT examination or representation of the Lung vessels in magnetic resonance (MR angiography), as well as a scintigraphy, an embolism can often be detected. Lung perfusion scintigraphy involves injecting radioactive particles into a vein; If a section of the lung is obstructed by an embolus, this part of the lung presents itself without radioactive particles, as these cannot get there via the closed vessel. Further diagnostic tools are cardiac ultrasound (Echocardiography), the EKG and the X-ray of the chest.
EKG changes in a pulmonary embolism
If there is a pulmonary embolism, then between a quarter and a half of the patients show changes in the ECG. The number shows that the ECG as a diagnostic tool is not very meaningful and has a low sensitivity.
In other words, this means that if the ECG is normal, a large number of patients still have pulmonary embolism. An older EKG, which was produced before there was any suspicion or symptoms of a pulmonary embolism, can be helpful for the attending physician. In comparison with the “fresh” ECG, individual changes in the patient can be seen and described more clearly.
The basis for changing the EKG in the event of a pulmonary embolism is that there is a volume and pressure load on the right heart. Due to the embolism of the pulmonary vessels, the resistance in the lungs increases and the right heart has to exert more force to pump the blood into and through the lungs.
Due to the greater stress on the right heart, the EKG shows a right type.
Further changes in the ECG can be the formation of an S1Q3 configuration (S wave in lead I and Q wave in lead III), a T negative for leads V1-3, and an incomplete to complete right bundle branch block.
These changes are partly differently pronounced and visible. For this reason, the diagnosis and evaluation of an ECG should only be carried out by a doctor.
Read a lot more information on this topic at: EKG changes in a pulmonary embolism
CT for pulmonary embolism
Computed tomography, or CT for short, is what it is today most important investigationif pulmonary embolism is suspected. By depicting the vessels of the lungs and, if present, the clot located in them as part of a so-called CT angiography can be very well judged whether a pulmonary embolism is present or not. If the doctors do not see any clots in the pulmonary vessels in this examination, it can be said with great certainty that the symptoms are not caused by a pulmonary embolism.
It is important that with a CT angiography Contrast media must be injected into a vein, as this is the only way to show the vascular system. The contrast medium is usually containing iodine and can one allergic reaction as well as trigger an overactive thyroid. Therefore, it must be known before the examination whether there is a known allergy to contrast media or an overactive thyroid.
D dimers
D-dimers are proteins that are released into the blood when clotted blood dissolves. A simple wound, on which the blood then clots and is broken down after a while, can therefore cause slightly increased D-dimers. However, thrombi (blood clots) that lie within a blood vessel are also broken down over time and can release D-dimers. Therefore, these proteins are an important blood value for ruling out pulmonary embolism. Since the causes of increased D-dimers are diverse, a high D-dimer value does not necessarily mean that a pulmonary embolism is present. Conversely, if the value is negative (no evidence of D-dimers), pulmonary embolism can be excluded.
Read more on the subject below: D-dimers
What is the Pulmonary Embolism Score?
With the pulmonary embolism score, patients are divided into risk groups based on various parameters. The points can be calculated from the following factors: For the age there is the number of years of life as points.The points for male sex (10 points), cancer (30 points), heart failure = cardiac insufficiency (10 points), pulse over 110 beats per minute (20 points), systolic blood pressure = first blood pressure value under 100 mmHg (30 points), respiratory rate over 30 per minute (20 points), body temperature below 36 ° C (20 points), decreased state of consciousness (60 points) and oxygen saturation below 90% (20 points) are added.
For those with less than 85 points, the risk of dying is low. Above that there is an increased risk.
Classification of pulmonary embolism

Staging of the Pulmonary embolism.
There are four degrees of severity.
- Stage I: easy
Clinic: only short-term or no symptoms.
Circulation failure: <25% - Stage II: moderate
Clinic: slight shortness of breath and accelerated pulse.
Circulation failure: 25% - 50% - Stage III: massive
Clinic: severe shortness of breath, collapse.
Circulation failure:> 50% - Stage IV: severe
Clinic: like stage III plus shock
Circulation failure:> 50%
Bilateral pulmonary embolism
The symptoms of a bilateral pulmonary embolism are basically the same as in a unilateral pulmonary embolism. However, because both lungs are affected, you may much more difficult. The severity also depends on the size of the affected vessels of the respective lung.
Only in the clinic can imaging examinations show which vessels are blocked by the clot and whether only one or both lungs are affected. The following therapy then depends mainly on the severity of the pulmonary embolism and the patient's condition.
Treatment of pulmonary embolism
The therapy depends essentially on the stage.
Therapeutic administration of heparin is necessary at every stage. Heparin is given via a so-called perfusor in a constant dose via a venous access.
From the Stage II to IV a so-called thrombolysis therapy (taking into account the contraindications, e.g. not after recent operations) can be carried out.
Thrombolytics actively dissolve the thrombosis or pulmonary embolism. Be for it Medication how:
- Streptokinase
- Urokinase
- rt-PA (tissue plasminogen activator)
given.
A major risk of this therapy is that the patient has a significant tendency to bleed during therapy.
From the Stage III to IV a so-called catheter fragmentation can be carried out. This method is only available in selected centers. A catheter is inserted through the blood vessel (artery) directly advanced to the pulmonary embolism and then mechanically crushed.
From stage IV and in absolute danger of death, an attempt can be made to remove the pulmonary embolism surgically.
In general, pulmonary embolism is followed by permanent coagulation therapy Marcumar on. Marcumar inhibits the coagulation system, which increases the time it takes for the blood to clot. This reduces the risk of developing a thrombosis.
What is first aid for a pulmonary embolism?
If acute signs of a pulmonary embolism occur, immediate first aid measures are necessary to ensure that the person concerned has a chance of survival. People who are conscious are often very restless, so they should be reassured first.
Due to the sudden lack of oxygen and the impact on the heart, the person should move and exercise as little as possible. It usually helps to lie down the person affected. The upper body should, however, be raised a little. It is important that the person concerned is spoken to so that a comfortable position can be found.
If the person is unconscious, breathing and pulse must be checked regularly. In the event of cardiac arrest, resuscitation (resuscitation) must be started immediately. This consists of alternating 30 chest compressions and 2 breath donations.
It is important not to forget to call the emergency doctor (112) in the excitement. The emergency doctor can use heparin (blood thinner) to treat the clot that caused it. In addition, oxygen and painkillers are usually required. Further treatment usually has to take place in hospital.
Lysis in pulmonary embolism
A lysis (more precisely "Fibrinolysis"Or"Thrombolysis“) In pulmonary embolism is usually carried out on patients who are in an unstable circulatory state. This can be seen, for example, from blood pressure, heart rate and the amount of oxygen in the blood. Its aim is to actively dissolve the clot and thus to open the closed vessel as quickly as possible. To do this, various drugs can be injected into a patient's vein.
A lysis always harbors that Risk of causing severe bleeding. For example, it should not be done if you have recently had major surgery or if you have a cerebral hemorrhage.
Guidelines
The 2010 guidelines hold on to that right at the beginning of a suspicion of Wells Score should be determined to assess the level of risk of pulmonary embolism.
The decrease in blood values and the determination of vital parameters such as blood pressure, pulse and temperature are always part of the basic diagnostics.
A recording is then made in Spiral CT made. In the next step, a ventilation and a perfusion scintigraphy can be performed to confirm or rule out a possible suspicion. According to the guidelines, an MR angiography can also be performed, although the informative value of this has not been fully proven. With an echocardiography (Cardiac ultrasound), an EKG and sonography (Ultrasonic) of the deep leg veins, the diagnosis can be completed.
The guidelines recommend anticoagulation after pulmonary embolism for 3 to 6 months. Depending on the cause of the embolism, anticoagulation can also be carried out for an unlimited period of time.
Duration of anticoagulation (taking Marcumar)
If a pulmonary embolism is diagnosed, Marcumar is usually used in Germany to thin the blood, also known as anticoagulation. How long the anticoagulation is necessary depends on the cause of the pulmonary embolism.
If a cause can be clearly identified that was only temporary - for example a long journey, immobility after an operation or a temporary, serious illness - Marcumar can usually discontinued after 3 months become.
If pulmonary embolism occurs in a known cancer, should lifelong or at least until Marcumar is cured.
If no cause can be determined, what to do next depends on whether a Leg vein thrombosis existed at the time of the pulmonary embolism. In the case of leg vein thrombosis in the hip or thigh close to the trunk lifelong anticoagulation should be performed. In the case of leg vein thromboses in the lower leg far from the trunk, anticoagulation can be applied 3 months be terminated.
If pulmonary embolism or leg vein thrombosis occurs repeatedly without a cause being determined, it is also recommended to take Marcumar for life. The final decision on the duration of the anticoagulation also includes factors such as previous illnesses and the risk of bleeding - that is why the duration of the anticoagulation is ultimately an individual decision by the attending physician.
Complications
Pulmonary embolism complications can include:
- Right heart failure (right heart failure)
- If the right heart is overloaded, life-threatening cardiac arrhythmias can develop, especially in severe pulmonary embolisms
- recurring small pulmonary embolisms lead to creeping right heart failure (right heart failure) with an equally unfavorable prognosis
- You can find more information on this topic under: Heart failure
- Inflammation of the breasts (pleurisy) due to poor blood circulation
- Dying off (necrosis) of the part of the lung that is not supplied with blood (lung infarction) - the result can be a bloody cough
- Inflammation of the lungs (pneumonia)
Pulmonary embolism with pneumonia
One possible complication of pulmonary embolism is the lung infection. It often develops in areas of the lungs that have at least partially died due to the vascular occlusion - so-called Pulmonary infarction.
Pulmonary infarction and pneumonia are not common in pulmonary embolism. Some of them are difficult to detect because they can express themselves very much like a pulmonary embolism. Indications that in addition to the embolism there is also pneumonia are, for example, yellow, purulent sputum, long-standing, high fever and greatly increased levels of inflammation in the blood. As a rule, pneumonia worsens the patient's condition significantly, delays recovery, or even leads to death.
Read more about this at: Signs of Pneumonia
prophylaxis
Since pulmonary embolism almost always results from a thrombosis, all prophylactic measures for thrombosis also apply to pulmonary embolism:
- Wearing compression stockings before operations or after delivery
- Use of anticoagulant drugs (e.g. heparin) during surgery or oral anticoagulants (e.g. Marcumar) after thrombosis
- Avoidance of the above risk factors
- In the case of recurring pulmonary embolisms, a so-called kava screen is inserted - a kind of sieve is implanted in the largest vein (vena cava) leading to the heart. This sieve or screen catches the floating thrombi from leg vein thrombosis and pelvic vein thrombosis so that they cannot get into the lungs.
- Regular and sufficient exercise to ensure a good blood supply to the leg veins, avoid long periods of sitting with knees bent
- Drink enough drinking enough to avoid blood thickening
Prevention of pulmonary embolism
A pulmonary embolism can affect anyone, although there are certain patient groups who are at increased risk of developing an embolism.
These risk groups can, however, reduce the risk by taking prophylactic measures. If there are diseases that increase the risk of thrombosis (like cancer, hormonal disorders, mutations around the coagulation system and others) permanent medication with anticoagulants may be indicated.
There are different drug groups here, whereby the coumarins are often used here. In Germany, the coumarin Marcumar® is the most commonly prescribed drug. Since it is oral (through the mouth) can be ingested and does not have to be injected, it is very suitable for long-term or permanent medications. When taking Marcumar® it is very important to always keep an eye on the INR value.
Read more about the topic here: INR
It is very important to wear compression stockings as this prevents the blood from building up in the legs and causing thrombi.
Especially when there are risk factors that cannot be removed, such as the Factor V Leiden mutation, unnecessary risk factors such as smoking should be avoided at all costs.
Before long trips, a doctor should be consulted for a one-time anticoagulation (Anticoagulant) with heparin - especially if the patient has one more or more risk factors.
Other very simple prophylactic measures are to avoid enough exercise and long periods of sitting. It should also be ensured that sufficient fluids are drunk.
Also read our topic: Prevention of pulmonary embolism
When can I fly again after a pulmonary embolism?
There is no clear consensus on how long not to fly after a pulmonary embolism. Mostly it is recommended about 6 months to wait before taking another flight after pulmonary embolism. However, the risk of having a pulmonary embolism again depends on many factors. Therefore should a Doctor consulted who can assess the risk of thrombosis based on the type of pulmonary embolism, the current condition of the patient, previous illnesses and the duration of the flight and advise accordingly.
In principle, however, an attempt should be made to keep the risk of a new pulmonary embolism as low as possible because the probability of serious consequential damage is high. For long periods after pulmonary embolism, care should therefore be taken to either choose travel destinations in relative proximity or to take precautionary measures to reduce the risk of thrombosis during a flight. These include, for example, compression stockings and injecting heparin.
forecast
The prognosis of a pulmonary embolism depends essentially on the size of the embolism and the duration of its existence and on recurring embolic events.
With consistent therapy, the probability of a new pulmonary embolism can be greatly reduced. The aim here is to prevent the formation of a thrombosis.
Without further therapy there is a great danger that the event will repeat itself (probability 30% !!!).
You might also be interested in: What are the chances of survival with a pulmonary embolism?
Length of hospital stay
The length of the hospital stay depends very much on the patient's condition. If the pulmonary embolism is small and treated quickly, patients usually can after a few days Stay on the normal ward to be discharged home.
Patients who are put into a life-threatening condition by a severe pulmonary embolism sometimes have to several weeks spend in intensive care until they are out of danger.
Often, despite a significant improvement in their condition, patients are a few days to monitor leave on station. The reason for this is that complications such as renewed pulmonary embolism or pneumonia occur particularly in the first few days after pulmonary embolism.
Duration of recovery
The length of time it takes to recover from pulmonary embolism varies greatly from patient to patient. After small pulmonary embolisms and therapy initiated quickly, those affected are often well again after a few days, whereas large pulmonary embolisms with late treatment can cause symptoms such as weakness, rapid fatigue and shortness of breath for weeks after hospitalization or even permanent symptoms.
Young patients usually recover faster than older patients. Pre-existing conditions of the heart or lungs can delay recovery. If complications such as pneumonia or permanent heart damage occur, recovery can also take significantly longer.
Length of incapacity for work
How long the incapacity for work lasts depends very much on the severity of the symptoms, the course of recovery and the type of job. The duration is usually decided by the family doctor based on the patient's wellbeing. In the best case, it can already be few days work to be resumed. In particular, activities that are not physically strenuous do not require a longer sick leave if the person concerned no longer shows any symptoms.
Severe pulmonary embolism can result in incapacity for work For months last for. Many sick people show rapid fatigue even weeks after their hospital stay, in the worst case permanently, after only little exertion. In the case of physically demanding activities, this can mean weeks of inability to work. Some patients even become permanently incapacitated after severe pulmonary embolism, especially if complications arise.
What are the chances of survival after a pulmonary embolism?
The chances of survival after a pulmonary embolism strongly depend on which part of the pulmonary vasculature is affected and which complications occur. The pulmonary embolism is basically divided into four degrees of severity.
In severity I, the chances of survival are best. Usually only small branches are affected and the embolism does not affect the heart function. Severity grade II is characterized by an incipient right heart failure. Somewhat larger arteries are blocked, which creates increased pressure in the vessels. On the other hand, the right ventricle has to pump, which is noticeable in a changed function. Here the survival rate is more than 75%. In severity III, the affected persons suffer a shock, the blood pressure drops, and the pulse rises at the same time. Because one of the main arteries in the lungs is affected by the embolism, the body cannot take in enough oxygen. Less than 75% of those affected survive this pulmonary embolism. The most dangerous level of severity is the fourth. Affected people need to be resuscitated because the heart stops beating due to the lack of oxygen.Less than half of those affected survived this event.
Can a pulmonary embolism be fatal and how often does it happen?
Pulmonary embolism is an extremely serious and serious condition. Depending on the severity, up to 50% of those affected die. The death rate is particularly high when large branches of the pulmonary vasculature are affected. If an embolism has only established itself in smaller branches, survival depends on the function of the heart. If the heart can compensate for the changes in the vessels, the embolism ends fatally in less than 25% of cases. If the heart is also affected, it is 25 to 50%. Very small embolisms can also cause a chronic course that is usually not noticed for years. Here the survival times are significantly longer than with acute pulmonary embolism.
What are the consequences of a pulmonary embolism?
The most dangerous consequences of a pulmonary embolism occur when the heart is also affected. Often times, a large thrombus (blood clot) blocks a pulmonary artery. This not only leads to the body taking in too little oxygen. In addition, there is a higher pressure in the pulmonary vessels, against which the right half of the heart in particular has to pump.
The combination of increased workload and less oxygen can seriously damage the heart muscles and lead to cardiac insufficiency, which in the worst case can be fatal. Another complication occurs when the lung tissue is not adequately supplied with blood (and therefore nutrients) for a long period of time. This under-supply is also known as a lung infarction. The affected areas can become inflamed, causing what is known as infarct pneumonia (pneumonia caused by a pulmonary infarction). In particular, if the lungs and heart are already weakened by the embolism, additional pneumonia can have fatal consequences.
Pulmonary embolism during pregnancy
Pulmonary embolism is one of the most common causes of death during pregnancy.
During pregnancy and after childbirth, women are at a greatly increased risk of pulmonary embolism. The reasons for this are that in the process of pregnancy the woman's body goes through extreme changes.
- On the one hand, the composition of the blood changes, which increases the risk of thrombus formation.
- On the other hand, the enlarged uterus presses on vessels in the lower abdomen and pelvic area, which changes or slows down the blood flow - this is also a risk factor for thrombosis.
- Another reason is that women simply move less and lie down more during pregnancy.
For prophylaxis, the pregnant woman can use anticoagulants (Administration of anticoagulants) become. This should be continued for a certain period of time after the birth (6 weeks if an embolism has occurred). Coumarins (Marcumar®) should not be used to inhibit clotting during pregnancy, as they can cross the placental barrier - that is, they also get through the uterus into the unborn child's circulation, where they can cause development damage.
After an embolism has expired, heparins are usually injected into the veins for a week. You can then switch to low molecular weight heparins, which have the advantage that they can be injected subcutaneously (into the subcutaneous tissue, e.g. on the abdomen or buttocks).
However, not every woman needs to be treated with heparins as a matter of principle. It is important to use it in women whose families are familiar with thromboses, embolisms and genetic diseases that favor them. It is also essential for women who have already had an embolism. They should also pay particular attention to possible symptoms of pulmonary embolism.
Read more on the topic:
- Pulmonary Embolism in Pregnancy
- Thrombosis in Pregnancy