Mammography
Synonyms in a broader sense
Digital mammography, magnetic resonance mammography, galactography, mammography screening
introduction
Mammography is a so-called imaging procedure. Usually an X-ray image is taken in two planes (from two different directions) chest made. To do this, each breast is pressed together between two Plexiglas plates for a few seconds. The compression ensures that the tissue is spread out and is easier to assess because less tissue is superimposed. The examination is carried out while standing. The Result the mammography is based on the BI-RADS classification (Breast Imaging Reposting and Data System) assessed:
Level I: No findings
Stage II: Findings that certainly benign are (e.g. cysts in the breast)
Stage III: Findings that probably benign are; a check is required
Stage IV: Findings that probably malicious are; a biopsy (= tissue sample) is required
Level V: Very suspicious Findings, a biopsy is required
Level 0: Diagnosis not feasible
Mammography Accuracy
Mammography has a sensitivity of 85-90%. Sensitivity is the sensitivity of a test to a disease. In other words, it describes the quality of a test to identify sick people as sick. A sensitivity of 85-90% means that 10-15% of breast cancer patients will not be detected with this method. Mammography therefore has a relatively good sensitivity.
However, it is relatively unspecific. The specificity indicates the number of true negative results of a method, i.e. how many healthy people are correctly recognized as healthy. Fibroadenomas (benign breast tumors), cysts in the breast or calcifications can look like breast cancer in the mammography, so a check-up should always be carried out after a certain time or a tissue sample (biopsy) should be carried out if the result is questionable.
Read more on the subject at: Breast biopsy
Radiation exposure
Like any x-ray examination (roentgen) mammography also exposes the body to radiation. In mammography, due to the special technology, these stress values are even higher than in an X-ray of the bones. Especially at a young age, breast tissue (Female breast) very sensitive to this type of radiation. Women under the age of 20 should therefore not undergo mammography. In women between the ages of 20 and 35, the risk should be weighed very carefully and, if necessary, other diagnostic methods should be used.
In addition, according to the current state of knowledge, screening mammography (for an explanation see below) is of no advantage for women under 40 to 50 years of age, since the younger a woman, the higher the proportion of false positive results. One of the reasons for this is the higher tissue density of the breasts in younger women (which also makes the general assessment of the X-ray more difficult). So benign changes are not recognized and an actually unnecessary and painful biopsy is carried out, quite apart from the emotional stress in the time until the negative biopsy result (negative means: no cancer).
Applications of mammography
1. If changes or lumps are noticed during the self-examination or the examination by the doctor, these can be examined further with the mammography.
2. In Germany there is also the "Mammography screening". Women who have no risk factors should have a routine mammogram every two years between the ages of 50 and 69. In women with risk factors (e.g. breast cancer diagnosis in close relatives or breast cancer in their own medical history), the mammography should be carried out earlier and annually (see Breast cancer risk).
Of the Mammography Screening Success is controversial. Proponents say it leads to a reduction in breast cancer mortality by around 25% to 30% after 5 to 6 years for women between the ages of 50 and 70. Critics point to new data evaluations and criticize the fact that the information from 25% - 30% relates to the relative risk reduction.
This relative risk reduction is demonstrably often misunderstood by patients but also by doctors, or the expected benefit for the participants is overestimated. In absolute terms, it means (absolute risk reduction):
- Without mammography screening, 4 out of 1000 women die of breast cancer during 10 “screening years”.
- During 10 “screening years” with mammography screening, the number of deaths falls from 4 to 3 in 1000 women
In relative terms, this is a 25% reduction. In other words: out of 1000 women who take part in the serial mammography five times over a period of 10 years, 999 women will have no benefit because they will not die of breast cancer anyway (996 women) or because they will still die of breast cancer (3 women). The absolute risk reduction so is only 0.1%. However, one in 1,000 women is saved by screening mammography.
Digital mammography
The principle of digital mammography is like "normal" mammography, the difference being in the images that are produced.
While in "normal" mammography the familiar X-ray images are created according to a principle similar to that of a camera, in digital mammography the images are not projected onto a film, but are converted directly into a computer file.
Advantages arise from the digital post-processing of the images, which is made possible in this way and the possibility three-dimensional images of the breast to make. If one compares the resolution and the richness of contrast of the images of the different methods, the advantages of conventional mammography currently still predominate, although Microcalclessions (please refer Breast cancers) are easier to see with the digital method. The radiation exposure is somewhat lower with digital mammography, but it causes high costs for the clinics due to the need to purchase new equipment, and the doctor must first learn how to assess the images. Overall, however, digital mammography is on the advance.
Magnetic resonance mammography

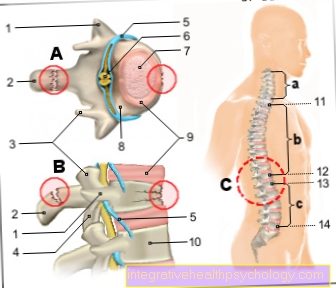
The Magnetic resonance mammography (MRI mammography or MRI of the chest) is a process in which different sectional images are made with the help of strong magnetic fields, which can later be put together to form a three-dimensional image of the breast.
Before the actual examination in the so-called "tube", a magnetic resonance mammography Contrast media Injected into the body through a vein in the arm.
Then the patient has to lie prone for 30 minutes in the magnetic resonance tomograph (MRI), if possible without moving too much.
You can find much more information about breast MRIs at: MRI of the chest
Info: magnetic resonance imaging (MRI)
Although the examination is completely painless for the patient, many patients still feel one MRI examination as uncomfortable; many suffer from claustrophobia and the noise during the examination. For this reason, hearing protection (provided) is part of the examination. In urgent cases, sedation with medication is possible and necessary. Since strong magnetic fields are used during the examination, it must be ensured that the patient does not have any metallic objects on the body (belt buckle, hair clips, etc.) or in the body (Pacemaker, artificial joints, insulin pump). Radiation exposure occurs to a lesser extent during this examination and not from the actual imaging, but from the injected contrast agent.
Magnetic resonance mammography has the highest sensitivity and accuracy in the detection of invasively growing breast tumors. In the case of dense glandular tissue, the combination of X-ray and Magnetic resonance mammography the highest level of diagnostic certainty to rule out breast cancer. With experienced examiners the sensitivity of the examination is approx. 90%, however there are also approx. 20% “false malignant (n)” findings. But even with this most complex method, not every cancer can be found.
Note: MRI reliability
Absolute security cannot be achieved with any procedure. Terms such as “the glass chest” used in some brochures or websites raise false hopes.
The quality of the examination varies greatly, which is why the health insurers only reimburse the examination in a few selected clinics. Because of the great effort involved in the investigation and the high costs, the MRI mammography is not a routine examination and is not suitable as a screening method, most health insurances only pay in special cases and on request.
MRI mammography is used as a supplement for findings that cannot be clarified by other examinations, especially in the case of non-palpable findings, also in the event of residual suspicion after an inconspicuous cell / tissue sample (biopsy) and if several cancer foci in a breast are suspected. In some studies, MRI mammography has been used with great success Early detection of relapsesi.e. Used when the cancer returns after treatment, or to diagnose a second, very small carcinoma in the other breast if there is an existing breast cancer finding.
As an alternative to digital mammography, magnetic resonance imaging can be used if a patient has very dense breast tissue or Breast implants Has. Radiation-free magnetic resonance mammography can also be used instead of digital mammography for high-risk patients (for example, if there is a particular family history).
Galactography
This examination is an extension of the classic mammography. It can be used especially if there is unilateral or bloody leakage from the nipple was observed.
In galactography, a contrast medium is injected into the milk ducts by inserting a very thin probe through the nipple. The milk duct system can be shown on the chest x-ray. Inserting the cannula can be uncomfortable or painful. Through this examination, so-called intraductal processes be made visible, i.e. Masses of space that up to this point have mainly grown within a milk duct and can thus be localized.
However, the examination cannot determine whether the mass is benign or malignant. Galactography is a total method rarely used and not infrequently unsuccessful because it is difficult to carry out.
However, specialized examiners hardly have any problems. The reliability of the diagnosis is good if carried out well. In part, the galactography has been replaced by sonography or the examination of the escaping fluid for cells by the pathologist.

















.jpg)