Medicines for high blood pressure
General

High blood pressure (= hypertension) belongs firmly to the group of so-called "common diseases". In the western world it is estimated that 30% of the population is affected. As the word high blood pressure correctly suggests, it is about excessive pressure in the blood. Since this high pressure is mostly expressed in the vascular system, especially in the arteries, one speaks of arterial high blood pressure or arterial hypertension. How it is created can be easily imagined using the model of a garden hose. In order to be able to water flowers properly, a certain water pressure is required at the end of the hose. You can get the pressure either by putting more water in the hose or opening the tap more or by sending the same amount of water through a thinner hose.
Transferred to our vascular system, this means that blood pressure depends on how much blood flows through the system and how narrow our vessels are. All of our organs can only be properly supplied with a sufficient amount at the end of the blood vessel system with a pressure that is neither too high nor too low. The amount of blood that flows is controlled by the heart by pumping more or less forcefully, or simply beating faster or slower. And the narrowness of our vessels is controlled by nerve tracts around the vessels. These nerve pathways control whether the muscle cells in the vessels tense and constrict or whether they relax and the vessel widens.
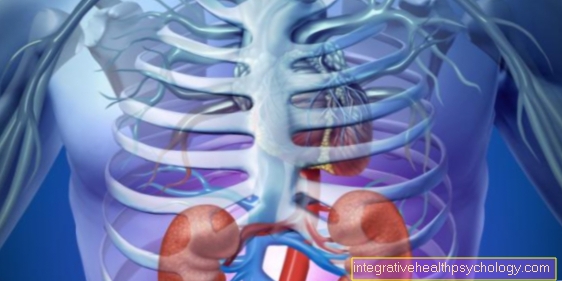
These mechanisms are used in drug therapy for high blood pressure in order to normalize the "abnormal" blood pressure again. A systolic "upper" value of is the limit for high blood pressure 140mmHg (mmHg = millimeters of mercury: unit of blood pressure measurement) and a diastolic "lower" value of 90 mmHg. The risk of suffering late damage caused by increased blood pressure without being noticed increases rapidly with increasing blood pressure values. To such late damage Vascular system, heart, brain, Kidneys and many other organs, a consistent treatment of high blood pressure is imperative.
The basic therapy of every treatment consists of general measures such as weight normalization, low-salt diet (max. 6g table salt per day), Mediterranean food (lots of fruit, salad & vegetables with little animal fat), no blood pressure-increasing medication (e.g. cortisone, pill) and change lifestyle habits (no coffee, hardly any alcohol, no cigarettes, learn relaxation techniques). 25% of patients with mild high blood pressure can be helped sufficiently and their blood pressure values can be improved enormously in this way, so that no further therapy is necessary.
Play alongside these general measures Medication a prominent role in therapy. As a rule, this is a long-term therapy. Unfortunately, this often means lifelong medication for those affected. The drugs can either be used alone as a so-called Step therapy or as Combination therapy administered. In the case of step therapy, you stick to one preparation first and only if the effect is insufficient are other preparations used and combined until the desired effect occurs. It is different with combination therapy: Here, different drugs are combined from the start in order to achieve the target blood pressure. When selecting the drugs, five groups of active substances in particular have prevailed. First choice drugs are so-called Diuretics, Beta blockers, ACE inhibitors, AT1 blocker and Calcium channel blockers.
Different classes of drugs
Many different drugs are used in high blood pressure therapy. However, one cannot say that one drug group is the best across the board.
Depending on the cause and especially depending on the existing comorbidities, the best medication for the individual case must be selected from the group of so-called antihypertensive agents.
Basically one differentiates:
- Diuretics
- Beta blockers
- ACE inhibitors
- AT1 blocker
- Calcium channel blockers
- Reserve drugs
which are each based on different operating principles and are described below.
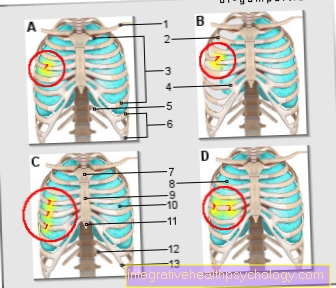
Diuretics
Diuretics are drugs that increase the body's excretion of water and salt in the kidneys. You also will be diuretic drugs called. Due to the increased loss of fluid, the blood volume in the body decreases and, similar to the model of the garden hose, by turning off the tap a little, the pressure in the hose or in the body's vascular system drops and the blood pressure drops. The additional loss of salt supports this effect. Salts have the property of binding water to themselves. If you lose salts (especially sodium) via the urine, additional water is excreted.
However, dehydrating drugs are usually not used alone for the treatment of high blood pressure, but as a combination with other active ingredients, e.g. From the group of dehydrating drugs, the so-called drugs are particularly suitable Thiazides. They are effective for a very long time and of medium potency, which makes them very suitable for long-term, moderate drainage. Unfortunately, they are only reliably effective if the kidneys are functioning properly. At kidney-damaged patients often no effect occurs and other diuretics must be used. Well-known representatives of the thiazides are Hydrochlorothiazide (HCT) or also Xipamide, a substance chemically related to thiazides.
In addition to the draining effect, they also have a direct effect on the vascular system after a longer period of therapy. This becomes less sensitive to the constricting nerve impulses and thus remains more relaxed. Since this effect only occurs with a delay of about 1-2 weeks, the effect can only be reliably assessed after 3-4 weeks of therapy. Side effects are rare with treatment with thiazides. If you come up, you mean to call nausea, Vomit or complaints in Digestive tract emerged. With most of the diuretics there is also the risk of derailing the body's salt balance. The kidney is a central organ regulating salts in our body. sodium, potassium, calcium and chloride are the most important substances here. By interfering with this sensitive system, many diuretics cause a loss, primarily of potassium. For this reason, the potassium level should be checked regularly. Especially in the elderly, this check should be carried out every 7-14 days by taking a blood sample at the beginning. If the potassium concentration is stable, this monthly check is sufficient.Potassium-rich diet (e.g. nuts, cocoa, broccoli, kohlrabi, dried fruit, bananas, currants) or the intake of potassium tablets can often prevent the potassium level from dropping too much.
If more dehydration has occurred than that desired with thiazides, this also occurs Loop diureticse.g. Torasemid for use. They are still effective even with impaired kidney function when thiazides no longer have any effect on the kidneys. Loop diuretics work in one part of the kidney, the Henle's loop, hence the name loop diuretic. Due to their strong and rapid dehydration, they are especially well suited for a derailment of blood pressure to extremely high values. In contrast to the thiazides, they are much more often fraught with side effects. The most important are Circulatory problems, a headache and thirst. In addition, the body's salt balance (= electrolyte balance) can get more confused than other diuretics due to the high level of dehydration and, above all, a lack of potassium (=Hypokalemia) can ultimately be dangerous for the heart.
Beta blockers
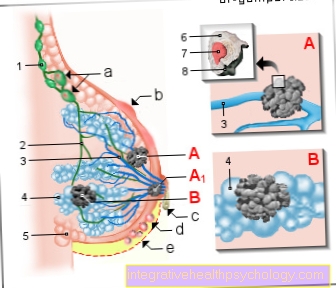
Beta blockers are especially indispensable in patients with weak pumping of the heart (= heart failure) or in patients who have had a heart attack. Beta blockers get their name from receptors at heart. Receptors are something like translators of cells and organs. Messenger substances dock on them and cause a predetermined change. The so-called beta receptors are located on the heart, among other things. They receive signals from our vegetative nervous system, here the so-called sympathetic nervous system.
It is activated during physical exertion and stress and makes our body more efficient. It increases the heart rate in the heart and makes it beat faster. It expands the bronchi so that we can breathe better and it inhibits the bowel movement in order to be able to provide as much energy as possible for performance.
The signals of the nervous system are received and converted by various receptors / translators. A distinction is made between alpha and beta receptors (Greek name for the letters A and B). Alpha receptors are located, among other things, on the vessels and cause constriction, while beta receptors are mainly found on the lungs and heart. Beta blockers prevent the driving sympathetic nervous system from working by blocking the beta receptor for its transmitter. The result is a heart that is beating less quickly and more forcefully. If the heart beats slower and less forcefully, less blood is pumped into the vascular system and blood pressure can drop.
In addition to the beneficial effect on high blood pressure, beta blockers also have the great advantage of lowering the oxygen consumption of the heart through slower and less powerful beating, because less work means less energy consumption. This benefits patients with diseases of the coronary arteries (= vessels that supply the heart and lie around it like a wreath), because in these patients the vessels are no longer able to transport enough blood to the heart muscle due to calcifications and insufficient blood flow and not Finally, heart attacks are the result. Particular care should be taken in therapy with beta blockers for those with asthma or others obstructive pulmonary disease like COPD required. Since the heart's receptors are also found in a similar variant on the lungs, stimulation of the receptors can not only have an effect on the heart, but also trigger an attack of shortness of breath, as the airways narrow due to the blockage of the beta receptors.
In further development, more selective beta blockers were developed which, in lower doses, have more effect on the heart than on the lungs, and so this complication is usually excluded. Examples of these so-called cardioselective (Cardio = heart) Beta blockers are metoprolol and atenolol. In addition to the asthma attack, the most important side effects of all beta blockers are weight gain at the beginning of treatment, malfunctions in male potency, drop in blood pressure up to circulatory collapse, an increase in the cholesterol level and an increase in the risks of diabetes mellitus. Diabetes or a heart that is permanently beating too slowly (= bradycardia) are therefore contraindications (=Contraindications) against taking a beta blocker. You can often recognize beta blockers by the ending "-olol“In the name of the active ingredient.
You can find much more information at: Beta blockers
ACE inhibitors

ACE inhibitors attack a completely different mechanism in the body. ACE inhibitors get their name from an enzyme that blocks them from working, the AC enzyme (=Angiotensin converting enzymes). This enzyme causes the body to release a substance that constricts the blood vessels, the so-called angiotensin, which translates as "Vascular tensioner". Since the ACE inhibitors block this AC enzyme and thus fewer substances that constrict the blood vessels are produced, the vessels remain wide and the blood pressure cannot rise too high.
Since the effect depends on the activity of the enzyme, the effect of an ACE inhibitor is often difficult to predict. Therapy should therefore be started at a low dose and under medical supervision. The activity of the enzyme is particularly high when diuretics are administered at the same time. Here the effect of an ACE inhibitor will be very strong. Combination therapy with these drugs should therefore only be started very carefully. In addition to this effect on the blood vessels, ACE inhibitors also have a beneficial effect on the course of heart failure. With this pumping weakness of the heart, they prevent a remodeling process that makes the heart more and more inefficient. A frequent complication of the therapy is a dry, irritating cough, which about 5-10% of the treated patients get.
Since this phenomenon is not limited to a single active ingredient from the group of ACE inhibitors, a change of the active ingredient does not make sense, but a complete change to another class of antihypertensive drugs is indicated. Therapy is usually chosen with the help of an AT1 blocker. Skin rashes and swellings, so-called edema, kidney dysfunction and sharp drops in blood pressure can also occur during treatment with ACE inhibitors.
ACE inhibitors are not allowed in cases of kidney damage, heart valve defects or during pregnancy. Here you have to switch to other preparations. The best-known representatives from the group of ACE inhibitors are captopril, the original substance of the ACE inhibitors, enalapril, a more effective and longer-lasting preparation. Newer preparations have an even longer duration of action, so that of the three times daily administration of captopril and the twice administration of enalapril, only a single dose is required here each day. The representatives of the ACE inhibitors can be recognized by the word ending "-pril“At the end of the active ingredient name.
Read more on this topic at: ACE inhibitors
AT1 blocker
AT1 blocker Like ACE inhibitors, they attack the body's angiotensin mechanism, but in different places. ACE inhibitors prevent the development and formation of angiotensin. AT1 blockers do not prevent the development of angiotensin, but rather the transmission of the angiotensin signal to the receptors for the angiotensin. Here, too, the consequence is that the actual effect of the receptor is not triggered. This means that the vessels cannot become narrow, but remain very wide so that the blood pressure can be kept lower. AT1 blockers will too Sartans called. They have been on the market since 1996 and are alongside the Ursubstans Losartan Some more members of the group are available today.
Well-known representatives of this group are Losartan, Valsartan, Candesartan or Eprosartan. The main differences to the ACE inhibitors are their side effects, despite the similar principles of action. In contrast to ACE inhibitors, sartans trigger dry coughs much less often. This makes them a very good alternative for affected patients who suffer from a dry cough. The therapy begins with the smallest dose and is then slowly increased to the target range. While losartan had to be administered several times a day, with the newer substances such as candesartan a once-daily dose is sufficient. The reason for this is the longer duration of action in the body, as the substances are broken down more slowly. Most common side effects of sartans are a headache, fatigue and dizziness.
Calcium channel blockers

Calcium channel blockers also reduce the narrowing of blood vessels in the body. They owe their name to the way they work in the body: calcium leads to constriction in the vessels. Here, too, there are structures that, in response to a certain messenger substance, lead to the opening of a channel, a kind of door to the cell. This opening ensures that calcium can flow into the cell, causing the vessels to constrict. If you block this channel through which the calcium flows, this stimulus is missing and the vessel remains wide. There are various chemical substances in calcium channel blockers, all of which prevent the influx of calcium.
The main representatives are
- Nifedipine
or - Amlodipine
from the chemical group of the dihydropyridines. Its side effects are essentially an increased, faster pulse and water retention in the legs, so-called edema.
Other substances of the calcium channel blockers also have an effect on the calcium balance in the heart, so that it beats more slowly and with less force and thus can be supplied with sufficient oxygen more easily. The group of calcium channel blockers, which includes the active ingredients verapamil and diltiazem from the chemical group of phenylalkylamines and benzothiazepines, is used in addition to high blood pressure therapy in patients with coronary artery disease or cardiac arrhythmias. The main side effect of nifedipine and verapamil is a slowing down of the heartbeat (= bradycardia: "brady" = slow) and cardiac arrhythmias. Common side effects of all calcium channel blockers are headache, dizziness, and facial flushing combined with a feeling of warmth and, like most other drugs, allergic reactions can occur.
Read more on this topic at: Calcium channel blockers
Reserve drugs
In addition to the drugs mentioned above, there are a few other drugs that are the second choice of high blood pressure therapy. Second choice because studies have not shown any improvement in the survival prognosis. Nevertheless, they lower high blood pressure. An important drug is, for example, clonidine, which acts directly on the nervous system and prevents the activity of our activating nervous system (= sympathetic nervous system), which is normally responsible for the congestion of blood vessels. It is used even more frequently in the emergency therapy of a high blood pressure crisis (= hypertonic crisis). Alpha-methyldopa is used for hypertension during pregnancy. Read more about the topic here: Lowering blood pressure during pregnancy
Minoxidil or dihydralazine are drugs that dilate even the smallest vessels by relaxing the muscles in the vessels that constrict them. However, since they make the heart beat faster, they should be given together with beta blockers.
Important rules for lowering blood pressure are:
- slow decrease in blood pressure
The body is used to high blood pressure and a too rapid pressure drop can mean an insufficient supply of the tissue and it can be damaged. The main side effects of lowering the blood pressure too quickly are headache, tiredness and dizziness. When choosing the right drug, concomitant diseases must always be taken into account. For example, asthma patients must not be treated with beta blockers without further ado, as these also work on the lungs and the bronchial tubes, which are narrow in asthma sufferers, would further constrict and thus cause shortness of breath.
At the start of treatment, you should always work with small doses as possible and keep the therapy schedule as simple as possible. Combination therapies should only be used if the result of the simple therapy is unsatisfactory. Regular checks are important and necessary, in which those affected are asked about their condition and possible side effects. The controls should also be carried out outside the practice. Home measuring devices and protocols are well suited for this in order to record blood pressure regularly.