migraine
Synonyms in a broader sense
Migraine attack, attack-like headache, hemicrania, hemicrania, unilateral headache, migraine attack, unilateral headache
English: Migraene
definition
Migraines are usually a pulsating headache that occurs like a seizure and is unilateral in nature. The pain usually begins on one side in the forehead, temple and eye area. In almost all cases, the headache attack is preceded by a so-called aura. These are visual disturbances that show up as flickering or jagged light phenomena or loss of field of view. In many cases, the headache is accompanied by symptoms such as vomiting and dizziness. Headaches with nausea or headaches with abdominal pain also often occur together.
Please also read: Pain over the eye
Epidemiology / gender distribution
Large studies have shown that around 10% of the Central European population suffer from migraines. The female sex is more often affected with a distribution of 2: 1.
For the first time, the half-sided headache usually occurs in the puberty or early adolescence, with girls and boys being affected about the same frequency in childhood.
The first occurrence of a migraine almost always takes place between the ages of 10 and 30. A first onset after the age of 50, however, is rare and must always be investigated for alternative causes of the headache.
Medical history / pathogenesis

Ultimately, the pathogenesis of migraines has not been clarified. There are currently various more or less reliable approaches / theories of the development of migraines.
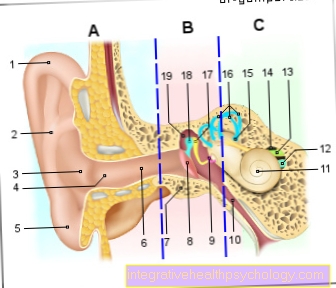
It is known that the human brain has no pain receptors. Headache pain occurs exclusively through the meninges (dura mater = hard meninges and pia mater = soft meninges), which surrounds the brain and spinal cord and their blood vessels (arteries and veins).
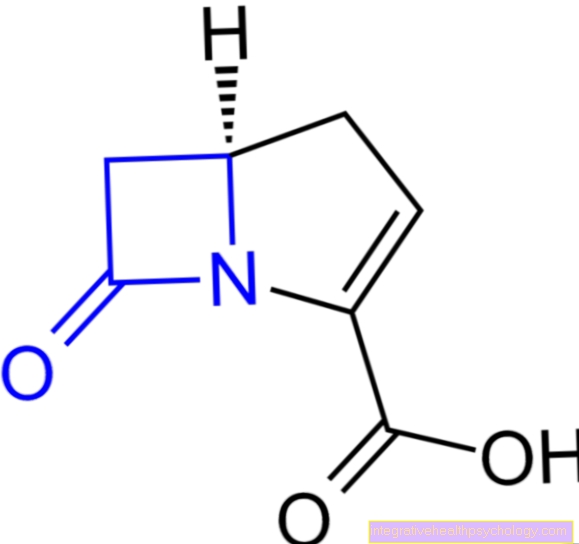
Many migraines start in the morning from sleep. A disturbance of the sleep-wake rhythm can lead to a migraine. An important substance of this sleep-wake rhythm is the messenger substance serotonin (5 HT or 5-hydroxytryptamine). This messenger substance can be released from the blood platelets (thrombocytes) by alcohol, especially red wine, and provoke an attack.
Other food-related triggers are said to be chocolate via the ingredient phenylatyalmin or cheese via tyramine.
Furthermore, the “stress hormones” adrenaline and noradrenaline have an important influence on the development. Both hormones regulate the size of the vessels in the brain.
One theory of the development of migraines describes a temporally and locally limited circulatory disorder of the brain. This leads to a narrowing of blood vessels in the brain and meninges, which can lead to neurological symptoms.
This circulatory disorder can be proven with highly specific examinations such as positron emission tomography (PET). The frequent evidence of a circulatory disorder in the back of the brain leads to the assumption that there is a so-called migraine center.The circulatory disorder can typically be detected before the actual migraine and coincides with the phase of the aura (see below).
Read more on the topic: Positron emission tomography
Another theory describes a temporary permeability of the vessel walls for blood components into the brain environment, which activates the body's own breakdown system (macrophages). This vascular permeability is caused by an extreme vasodilation that follows the phase of blood vessel constriction. As part of these breakdown processes, there is a localized inflammatory reaction around the blood vessels of the meninges. Since the meninges are very sensitive to pain, the severe headache develops, which is therefore partly perceived in synchronism with the pulse. That means the pulse beat causes a throbbing pain. This form of inflammation is sometimes referred to as neurogenic inflammation.
It seems certain that there is a disorder of a certain calcium channel (P / Q - calcium channel) in the brain. A voltage can be generated through the exchange of calcium ions inside and outside the cell, whereby brain cells are able to “communicate” with other brain cells. a disruption of the calcium channel leads to a disruption of communication with the following neurological symptoms and headaches.
Note
Based on the many theories you can understand that the origin of migraines has not yet been conclusively clarified and that the disease is certainly a combination of the different theories.
aura

An aura can occur at about every 5th -10th Migraine sufferers (10-20%). These are neurological deficits in the eye 10 to 60 minutes before the start of the actual migraine attack. In exceptional cases it can last for several hours. The cause is said to be a temporal and local circulatory disorder in the brain.
Read more on this topic at: Migraine attack
Typical neurological symptoms of the aura are:
- blurred / blurred / distorted vision (shimmering scotoma)
- Visual field loss, which means that parts of the visual field of the eye go blind, which is often not noticed directly, as the brain replaces lost areas
- Double vision
- Sensory disturbances
- Speech disorder
- partially up to hemiplegia and numbness (read also: numbness of the head and scalp)
When the headache starts, the symptoms of the aura are usually gone.
Risk factors
Risk factors that promote the development of migraines are:
- Hormones: especially the female sex hormone estrogen seems to play an important role in it. This assumption is based on the observation that children have a gender distribution of 1: 1, while after puberty the sex ratio shifts “in favor” of the female sex as the estrogen level rises. Typically, there is an attack in estrogen withdrawal (women before or during menstruation (menstrual bleeding). This form of migraine is particularly difficult to treat because it responds only unsatisfactorily to drug therapy and the phase of the migraine attack lasts particularly long Menopause (menopause) a decrease in migraines can be observed after the age of 50.
- stress (Adrenaline seems to have an important influence on the development of migraines. Over adrenaline or Norepinephrine will include the Vessel width of the arteries). Especially in the relaxation phases on the weekend, after a long sleep or on vacation when the adrenaline level drops.
- food, especially red wine, which leads to the release of serotonin from the blood platelets, chocolate or cheese are said to promote the development of migraines. Heavy caffeine consumption also increases the risk.
- Medication e.g. Nitrates like Digitoxin etc .. These drugs affect the size of the vessels.
- Hereditary factorsif a family history of migraine is known, especially if the father or mother is sick, there is an increased risk of getting sick themselves. An inheritance of up to 50% from parents to children can be proven.
- Alcohol, especially red wine, can provoke migraines
- Disturbance of sleep rhythm, Both too short and too long sleep (for example on the weekend - see also stress) can be a triggering factor. Air travel with a time difference is also considered a risk factor.
- other triggering factors can Hypoglycaemia (Hypoglycemia), Lack of sleep, sleep deprivation, or caffeine deprivation)
Symptoms
Typical Symptoms a migraine are:
- Hemiplegia headache
- stomach pain and nausea (80%)
- Vomiting (40%)
- often start in the morning
- Duration several hours to days
- Pulsating / knocking character of pain
- Increase in complaints under stress
- Aura before the onset of migraines
- Photophobia (60%)
- Noise shy (50%)
- Ringing in the ears / Tinitus
- rarely paralysis of the arms and legs
- Frequency 1 - 2 times a month
- Pain behind the eye
to form
Migraines with aura
This form of migraine is found in 10-20% of all cases.
Migraines without aura
This form is the most common. Typical migraine symptoms are found without having neurological deficits prior to the migraine.
childhood migraines
Children's migraines - also known as migraines in children - are characterized by a number of peculiarities. The seizure duration is usually shorter and the accompanying symptoms such as nausea and Vomit are often more pronounced than in adults. In some cases, pronounced neurological symptoms such as speech disorders or Hallucinations described in terms of an aura.
Status migraine
By definition, the headache typical of migraine lasts for more than 3 days. It responds particularly poorly to medication. The migraine status is often found as a hormone withdrawal headache, in women during their period (menstruation).
Migraines without a headache
Especially at the beginning of the migraine illness, the typical migraine symptoms can occur without the typical half-sided headache occurring. As a rule, the full picture of the migraine develops with further attacks.
Diagnosis
The diagnosis of migraine disease is usually based on the medical history (anamnesis).
Imaging procedures such as X-rays, CT or MRT are normal. In the early phase of a migraine, positron emission tomography (PET) can detect increased blood flow in certain brain stem areas. This gave rise to the theory that there is a migraine center.
You can find out more about diagnostics under: How do I recognize a migraine?
Read on on the topic Migraine Therapy