MRSA
definition
The abbreviation MRSA originally stands for "Methicillin-resistant Staphylococcus aureus" and not, as is often wrongly assumed, for "Multi-resistant Staphylococcus aureus". Staphylococcus aureus is a gram-positive, spherical bacterium that can be found almost everywhere in nature and in many people (around 30% of the population) Population) is also part of the natural flora of the skin and upper respiratory tract.
This means that these people are colonized (= colonized) with the germ without showing any symptoms under normal circumstances. In principle, however, Staphylococcus aureus is a pathogenic bacterium, which means that it is able to trigger a large number of different diseases. If it can spread under favorable conditions or if it encounters a weakened immune system, it can become dangerous for humans with the help of various so-called pathogenicity factors.
Read more about the topic here: multi-resistant hospital germs

Symptoms
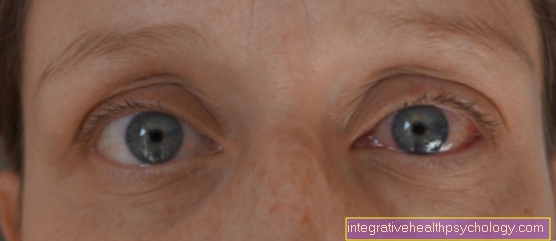
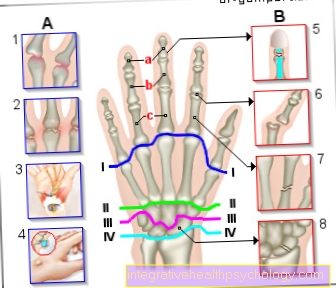
The most common symptoms include skin infections (often purulent: folliculitis, boils, etc.), food poisoning, and muscle or bone diseases. In worse cases, however, this bacterium can also cause pneumonia, endocarditis (inflammation of the innermost layer of the heart), sepsis (colloquially blood poisoning) or the Toxic Shock Syndrome (TSS) specific to this germ and can even be life-threatening.
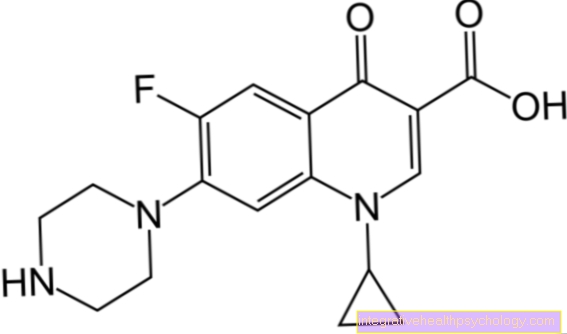
Staphylococcus aureus usually responds well to a variety of antibiotics, which is why a simple disease with this bacterium can usually be treated well with a 1st or 2nd generation cephalosporin (e.g. cefuroxime). The special thing about the MRSA strains is that they do not respond to the usual broad-spectrum antibiotics. It is said that this germ is resistant to these antibiotics.
The resistance to methicillin comes from the fact that the bacterium changes its surface structure in such a way that the antibiotic can no longer bind as well to its surface, which would, however, be necessary in order to develop its effect. Unfortunately, the resistance is only rarely limited to methicillin, but also affects various other antibiotics that can otherwise be used. Hence the common term multi-resistant Staphylococcus aureus. As a result, infections with MRSA are difficult to treat and require different treatment than the standard Staphylococcus aureus. It is usually done with glycopeptides such as vancomycin. This gives rise to the special significance of this germ: in its spectrum of diseases it corresponds roughly to the other strains, but diseases cannot be cured so quickly and thus put patients in greater danger.
Nosocomial infection

Infection with MRSA is of particular relevance in hospitals and care facilities, especially in the context of so-called nosocomial infections (infections that are temporally related to an inpatient medical task and that did not already exist before).
It is assumed that the prevalence of MRSA in the general population is around 0.4%, in nursing and old people's homes around 2.5% and in hospitals as much as 25%.
For this reason, a distinction is made between two groups of MRSA:
- The MRSA Infection That Hospital Acquires: Hospital aquired MRSA. The elderly and those with weak immune systems are at increased risk for this type of infection
- The MRSA Infection That Occurs Outside the Hospital: Community Acquired MRSA c-MRSA. This form is comparatively rare and also occurs in younger people. It is also associated with a slightly different clinical picture, for example necrotizing pneumonia and is found more frequently in people who have a certain gene.
transmission
Most commonly, MRSA is transmitted through direct human-to-human contact. Since many people wear it on their skin, a simple handshake is often enough to pass the germ on to the other person. Both in hospitals and in nursing homes, many people are in a relatively limited space where there is frequent skin contact (between nursing staff or doctors and patients), which is why a high MRSA rate in these facilities seems logical.
Even a person who is contaminated with MRSA and does not show any symptoms can infect another symptomatically, which results in an additional problem.
In addition, the germ can also adhere well to different surfaces. As a result, it can also be transmitted via liquids or contaminated objects (catheters and breathing tubes are the most common options here). The first symptoms usually appear around 4 to 10 days after infection. These are similar to those caused by the normal Staphylococcus aureus.
infection
MRSA is primarily through direct Skin to skin Transfer contact. Infection via fabrics, clothing, objects, surfaces or even ventilation systems in the form of a Droplet infection possible.
However, not every short-term colonization of the skin is synonymous with a permanent MRSA infestation, let alone a symptomatic infection. Rather, the pathogen usually does not succeed in gaining a foothold on the skin or mucous membrane of healthy people, as it is fended off there by the normal bacterial flora of the skin. Accordingly, MRSA is especially a problem for all people who have either immune weakened are, especially old and sick people.Or whenever the germ is offered a particularly suitable gateway.
This is classically the case in the context of operations or hospital stays in general. As part of an operation, the normal protective barrier is broken, and surgical instruments are inserted into the body. It is therefore not surprising that longer hospital stays or operations carry a certain risk of becoming infected with MRSA.
The more complex the medical care is, the more so, above all, are at risk Intensive care patients, or dialysis patients People. Every artificial access, be it the intravenous cannula, the ventilation tube or the dialysis catheter, represents a potential access route for germs.
Unfortunately, MRSA adheres particularly well to plastic and stainless steel, i.e. the materials most frequently used in hospitals. Unfortunately, MRSA infections are also relatively widespread among people who need long-term care and thus in many nursing homes.
Therefore, as a relative, you should also pay attention to hygiene measures, such as hand disinfection, when visiting nursing homes or hospitals. As mentioned above, however, not every contact with the MRSA pathogen is synonymous with infection. However, frequent and close contact with infected people increases the risk.
The pathogen can also be transmitted from animal to person. Infection is particularly possible in agriculture, when there is close contact with pigs. If the infection or carrier status is known, one can contact depending on the location of the infection Gloves and or Mouthguard protect against transmission. You should also pay attention to this in your private environment, e.g. also with relatives in need of care.
therapy
Aside from treatment with the special antibiotics already mentioned, such as clindamycin, further measures must be taken in a patient with MRSA. Not only when the germ has become symptomatic, but also when an asymptomatic colonization has been proven, the rehabilitation of patients (and staff!) Should be carried out. This means that, depending on the location of the contamination, you have to use a special antiseptic soap (Skinsan Scrub) or a nasal ointment (Mupirocin) every day to get rid of the germ. The success of this treatment can be determined with the help of a smear, which the doctor takes from a previously colonized area at the earliest 3 days after the start of therapy.
In addition, any work surfaces or equipment that the MRSA patient has come into contact with must be disinfected at regular intervals. In addition, the patient is isolated. This means that he is usually given a single room in the hospital. This may only be entered by people who wear a face mask and a protective gown. Before and after leaving the room, it is absolutely necessary to carry out hygienic hand disinfection correctly. Disposable items from the patient must be removed in a special garbage.
There are also special guidelines that must be followed for operations on MRSA patients. While an extra operating room is not required, an operation should, if possible, be carried out at the end of the day and special disinfectants must be used. With all these rules of conduct, one tries to keep the spread of the multi-resistant germ as low as possible.
MRSA test
To take a test on MRSA the corresponding samples must first be taken.
A swab is used to smear the affected areas of the skin with a cotton swab. In many clinics, this is already done routinely at the time of inpatient admission. Usually the sample is taken from a few representative body regions, especially the nose and throat, as well as the groin area.
If MRSA is suspected to be colonized by bladder or venous catheters, a sample is taken directly from them, or parts of the removed catheter are simply sent in directly. There are then various methods for the actual detection of MRSA. The classic method is the cultivation of the samples in the lab. However, due to the incubation times until the bacterial colonies grow, this takes a few days. Bacteria are grown on a blood-containing agar medium in microbiological laboratories.
At first only one infection can be identified Staphylococcus aureus prove, which is characterized by a certain colony shape and growth behavior. Whether it is then, however, one MR staphylococcus aureus, i.e. a Staphylococcus aureus strain that is methicillin-resistant (or colloquially multi-resistant) must then be determined with further tests. With the help of antibiotic platelets and the so-called agar diffusion test, or by creating dilution series, the resistance level of the cultivated pathogens is determined.
Alternatively, you can also use culture media that already contain an appropriate antibiotic, so that only on them Resistant staphylococci Trunks grow. The disadvantage of this method is clearly that cultivation takes several days, but it is comparatively cheap and easy to carry out. Alternatively, there are newer developments that support the MRSA directly, by means of so-called PCR prove. At this P.olymeraseKetten-R.action (PCR), DNA fragments of the bacterium are duplicated and then detected. This allows the bacterial DNA of the MRSA pathogen to be detected directly without the detour of cultivating colonies.
This procedure is much faster and gives a result after 2-3 hours. It is therefore mainly used to quickly rule out colonization. This is particularly helpful when people have had contact with MRSA, in order to quickly rule out an infection.
Rehabilitation of the MRSA germ
Remediation is not always easy due to the resistance.
A distinction must be made between the treatment of a symptomatic infection with MRSA itself and colonization of the skin or mucous membranes. With such a colonization, the measures are mainly limited to external applications.
Before treating MRSA, however, the remedial ability should be checked. So should be in front of a drug rehabilitation no more catheters or feeding tubes are present. Open wounds or skin infections must also have been treated in advance as far as possible in order to increase the chances of success of the rehabilitation.
The renovation itself then takes about 5 - 7 days. In this phase, on the one hand, antibiotic nasal ointment (e.g. Mupirocin ointment) Applied 3 * daily. In addition, there is oral and dental care with a disinfectant approved for mucous membranes, such as Octenidol.
In addition, the whole body and hair must be washed with a disinfectant washing solution, such as B. Octenisane getting washed. In addition, all objects and surfaces used must be disinfected and towels must be cleaned immediately after use.
A smear is used as a control for success 48 h after completion of the renovation and then again after 6 And then to 12 months carried out. MRSA remediation has only been successful if all smears are negative. Another problem area is one symptomatic MRSA infectionthat is to be treated systemically with an antibiotic.
Due to the resistance of MRSA to the otherwise very frequently used group of ß-lactam antibiotics, you have to fall back on some antibiotics from the group of so-called reserve antibiotics. The exact antibiotic to be used is then determined by means of an antibiogram and based on clinical experience. In the antibiogram it is determined in advance to which agent the respective MRSA strain is most sensitive. Often antibiotics come from the group of Glycopeptides (e.g. Vancomycin) or newer preparations such as Linezolid, or Daptomycin to use.
Often also in combination with e.g. Rifampicin, Clindamycin or Gentamicin. Before the actual treatment, removable sources of infection, such as catheters, must be removed if possible. The additional rehabilitation of the body surface and the mucous membranes is also important.
Patients with an MRSA infection are given an isolation room and special attention must be paid to hygiene measures.
prophylaxis
So that the spread of MRSA does not get out of hand in hospitals, patient screening is now carried out before admission. Here, with the help of a questionnaire, various risk factors for infection with MRSA are recorded (e.g. age and previous antibiotic therapy). Risk patients are then checked for an infection. In some European countries, however, hospitals have even started testing a smear for the presence of MRSA on every patient they admit.
Since 2009, the detection of MRSA in blood or cerebrospinal fluid (liquor) has been subject to mandatory reporting in Germany.