Anesthesia at the dentist
introduction
In order to make the treatment as pleasant and painless as possible for the patient, there are various anesthetic options available at the dentist. They range from local anesthesia using a syringe to sedation and anesthesia.
General anesthesia, in which the patient is not aware of the treatment, is very rarely used by the dentist and only in exceptional cases.

General anesthesia at the dentist
Under general anesthesia (also called intubation anesthesia) not only pain perception, but also reflexes, awareness and the ability to move are switched off. The patient “sleeps” and needs ventilation and close supervision. This is why general anesthesia is used during operations and under the supervision of an anesthetist. A normal dental practice is usually not equipped for this.
In almost all cases, dental treatment does not require general anesthesia, especially since ventilation makes it difficult to access the mouth.
Sedation is more common. The patient is in a “twilight sleep”, not really awake, but still responsive. You can breathe normally under sedation and respond to prompts, but you don't remember the procedure. Sedation also has an anti-anxiety effect. In order to prevent the transmission of pain at the same time, analgesic sedation is used. It can be done in the dental office and does not require the presence of an anesthetist.
The dentist needs further training in order to be able to offer sedation. In Germany, midazolam sedation via intravenous access is widespread, while nitrous oxide sedation is popular in English-speaking countries.
Read on below: Anesthesia - you should know that
Indications for general anesthesia at the dentist
General anesthesia for dental interventions is an exception that must be strictly justified. The prerequisite is that treatment under local anesthesia is not possible. Examples of possible indications are
-
costly restoration of teeth if there is a lack of willingness to cooperate
-
mental disorders that prevent the patient from cooperating
-
mental disability
-
previous physical illness
-
Toddlers
The dentist must decide whether the treatment is only possible under general anesthesia or whether sedation is an option and consult with the family doctor and anesthetist.
General anesthesia in the child for dental treatment
The anesthetist is responsible for carrying out and monitoring general anesthesia in children during dental interventions (also in outpatient use).
Children under 12-16 years of age are usually not sedated, but treated under general anesthesia if local anesthesia is insufficient or the child is not cooperative. This can be the case with small children or disabled children.
As with adults, general anesthesia should only be used if it is necessary, as it involves risks. Patients often complain after waking up from anesthesia
- Nausea,
- Headache and
- Confusion.
- Children sometimes suffer from diarrhea after anesthesia.
You might also be interested in: General anesthesia in children
Local anesthesia at the dentist
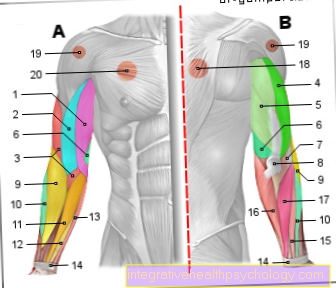
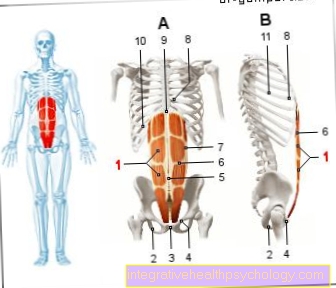
The most common form of pain relief at the dentist is local anesthesia. The local anesthetic is injected into the tissue surrounding the nerve fibers. The local anesthetic diffuses to the nerve fibers and there temporarily blocks the transmission of pain stimuli.
However, the patient can still feel pressure and movement (e.g. jolting the drill).
Depending on the treatment planned and the affected area in the mouth, the dentist can choose between different types of local anesthesia.
-
The surface anesthesia works without a syringe and only works for a very short time and not in deeper tissue layers. It is therefore rarely used.
-
Infiltration anesthesia is typical for treatments in the upper jaw or lower anterior region. 1-2 teeth and small areas of the mucous membrane are numbed. To do this, the dentist pricks the fold between the root of the tooth and the lip. In the area of the maxillary canines in particular, the infiltration anesthesia can also numb the outer part of the nose, lip and cheek. The patient feels a tingling sensation on the skin.
-
Conduction anesthesia is most commonly used for the lower jaw. 30-50% of a jaw and superficial parts of the tongue are anesthetized. This local anesthetic lasts the longest.
Because local anesthesia does not affect the consciousness and, if used correctly, has no effect on the cardiovascular system, the patient can leave the dental practice immediately after treatment and does not have to be observed first, as is the case with sedation or general anesthesia.
It is recommended that after local anesthesia, people eat and drink again only when the numbness has subsided, so that one does not injure oneself unnoticed. From a medical point of view, there is no reason not to drive a car after receiving local anesthesia. However, in the case of a traffic control it can be irritating if the language is impaired or the lip is still drooping numb.
Learn more at: Conduction anesthesia at the dentist
What are the advantages and disadvantages of local or general anesthesia?
Advantages of local anesthesia at the dentist:
-
easy
-
Dentists are very experienced
-
quick onset of action
-
Patients no longer need to stay or be observed after treatment
-
you don't have to be sober
-
usually free of charge for patients
Disadvantages of local anesthesia at the dentist
-
does not relieve anxiety
-
the patient remembers the procedure
-
the dentist depends on the patient's ability to cooperate
-
after longer treatments you have to inject
-
Local anesthesia works poorly in the inflamed tissue
Benefits of general anesthesia
-
the patient does not notice anything (good for children and anxious patients)
-
complicated interventions can be carried out
-
the practitioner is not dependent on the patient's willingness to cooperate
Disadvantages of general anesthesia
-
complex procedure
-
Anesthetist with equipment is necessary
-
is usually not paid for by the health insurance company
-
Risks and side effects should be considered
-
Patients must be fasted and monitored after surgery
Side effects and risks of anesthesia at the dentist
General anesthesia is a safe procedure that is used daily in hospitals. A mixture of different drugs is given to help regulate body functions.
These have side effects that become apparent after waking up from anesthesia, e.g. as
- Nausea and vomiting,
- A headache,
- Confusion and
- Express tremors.
- Intubation for ventilation can cause hoarseness.
Learn more at: Aftermath of anesthesia
In addition to these quite harmless but uncomfortable short-term side effects, there are also risks that the patient should be aware of. This includes e.g. Allergies to components of the drugs used, malignant hyperthermia, a genetic change that can lead to life-threatening conditions under general anesthesia, and the escape of contents of the esophagus into the airways (aspiration). The latter can be avoided by sobriety before the procedure and correct positioning.
One of the risks and side effects of sedation is
- the loss of protective reflexes,
- Unconsciousness or
- To mention respiratory and circulatory depression.
Local anesthesia can lead to infections at the injection site. If the nerve is hit directly, it can lead to partially permanent numbness. If the local anesthetic is administered into a blood vessel, it affects the cardiovascular system. It can also lead to intolerance or allergic reactions.
As with all other narcotics, the maximum dose must not be exceeded.
also read: Risks of anesthesia
Anesthesia at the dentist during pregnancy
You can also undergo general anesthesia during pregnancy. However, it should be noted that only urgent dental procedures should be performed during pregnancy and elective procedures should only be planned for after delivery. Emergency treatments can then also take place under local anesthesia.
If dental treatment under general anesthesia is unavoidable, the procedure must be carefully planned by the anesthetist, gynecologist, and dentist to prevent complications. The same applies to analgesic sedation during pregnancy. Propofol is used during pregnancy for deep sedation (e.g. in intensive care medicine), but a risk-benefit assessment must always be carried out, as most treatments can be postponed until after the birth .
Local anesthesia is usually not a problem for pregnant women. For the local anesthetic, the dentist can choose an anesthetic that does not penetrate the placenta and that is tolerated during pregnancy, e.g. Articaine or Bupivacaine. There are no known negative effects of local anesthetics on mother or child during breastfeeding.
For more information, see: Anesthesia during pregnancy
Recommendations from the editorial team
You might also be interested in the following topics:
- Anesthesia in the elderly
- Anesthetics
- Sedation
- Wake up time after general anesthesia
- Local anesthesia at the dentist










.jpg)