neuralgia
introduction
Neuralgia is the technical term for nerve pain and describes pain that occurs in the supply area of a nerve. It is triggered by an injury to the nerve itself, rather than damage to the surrounding tissue.
Mechanical effects such as pressure, inflammation, metabolic disorders, chemical effects such as chemical burns and radiation damage can be responsible for nerve damage.

What are the underlying causes of neuralgia?
Neuralgia results from damage to a nerve. The nerve fibers are irritated and irritated in different ways, which then cause the pain. The mechanisms that trigger the pain can have different reasons. For example, the insulating layer of the nerve may have been damaged, which is why ongoing excitement also transfers to the pain fibers and activates them. Furthermore, the nerve can be blocked by an injury, which leads to a lack of information in the brain and consequently to pain.
It is also possible that the nerve is no longer supplied with enough blood as a result of the damage, which is why there is an undersupply, metabolic products accumulate in the nerve cells and pain occurs as a result.
The causes that lead to nerve damage and the pain associated with it are diverse, including:
- Mechanical influences e.g. by crushing in an accident.
- Nerve inflammation such as a shingles
- Metabolic diseases like diabetes.
- Chemical influences e.g. Nerve pain occurs as a result of severe burns or radiation damage.
Read more on the topic: Nerve pain
Neuralgia on the face
If neuralgia occurs on the face, it is extremely uncomfortable for the person concerned. Even small touches of the skin or movements, such as those when speaking or chewing, cause pain.
If this sensitivity to pain increases to its highest level, even a gust of wind blowing across the face can cause pain.The strength with which the pain occurs in facial neuralgia is enormous. When patients are asked to rate pain intensity on a scale from 1 to 10, the score is almost always 9 or 10.
A particularly common nerve pain in the face is trigeminal neuralgia. The damage or irritation occurs in the trigeminal nerve, a cranial nerve that is responsible for the sensitivity in the face. The pain sensations are also conducted via this nerve. The nerve pain is described by the patients as attack-like and extremely intense.
Treatment of trigeminal neuralgia is difficult because conventional pain medication has little or no effect. For this reason, carbamazepine, an anti-spasmodic, is often used, which is also used in the drug therapy of epilepsy. The remedy lowers the stimulus threshold for pain sensations and thus has a preventive effect. Surgical treatment of neuralgia on the face, in which parts of the causative nerves are severed, is at high risk of consequential damage. Often lifelong sensory disorders remain in the face. However, an operation is the last resort and is only considered if the patient is extremely distressed.
Neuralgia on the ear
In the vast majority of cases, neuralgia in the ear is post-herbal neuralgia. Here it comes after a zoster oticus, i.e. a herpes disease in the ear, to persistent pain. The type of pain and the duration of the attacks are similar to those of the other forms of neuralgia: recurring periods of intense, shooting pain lasting seconds to minutes. In addition, trigeminal neuralgia can manifest itself predominantly in the ear if the branches of the trigeminal nerve leading to the ear are affected.
Neuralgic pain in the ear can also occur in the context of occipital neuralgia. The occipital nerve, i.e. the nerve for the back of the head, is the culprit. The ear can then be affected as some branches of the nerve pull into the ear and carry pain information from the ear to the brain. Again, violent pain attacks lasting a few seconds to several minutes occur again and again.
Neuralgia on the jaw
Neuralgia in the jaw is based on damage to the nerve tracts that run in the jaw to the teeth. This can be triggered by tooth decay, inflammation or other dental diseases, but it can also be the result of dental treatment.
The neuralgia manifests itself in the form of shooting pains that radiate from the tooth into the palate and jaw. The pain attacks are usually triggered by chewing, cold or warmth. If you have any such complaints, a dental examination as soon as possible is urgently recommended. Too long hesitation can cause the process to progress, which should be prevented. Long-term use of painkillers cannot replace a visit to the dentist. Firstly, this does not eliminate the cause, but only suppresses the symptoms, and secondly, long-term use of painkillers can have significant side effects, such as stomach ulcers.
Trigeminal neuralgia also sometimes manifests itself in the form of neuralgic pain in the jaw. This is the case when it affects branches of the trigeminal nerve that run in the skin above the jaw.
Neuralgia on the teeth
The surface of the teeth is not equipped with nerves and is therefore not sensitive to pain. But to the chagrin of many concerned, this does not apply to the tooth pulp (Tooth pulp) and the neck of the tooth. If an inflammation develops in these inner parts of the tooth or if a caries disease penetrates to the pulp, the nerves running there are directly irritated. In this way, the typical, extremely unpleasant neuralgia pains arise, which most of those affected describe as "shooting in" and very severe.
If you experience such discomfort on your teeth, do not wait and see a dentist as soon as possible. For the reasons described above, the complaints are a sign that the disease has already penetrated the inside of the tooth and requires immediate treatment.
What is trigeminal neuralgia?
Trigeminal neuralgia is one of the most common forms of neuralgia. In this clinical picture, the trigeminal nerve is affected, the numerous branches of which "sensitively supply" the skin of the face, as the expert says. This means that all sensory information from the facial skin, i.e. information about touch, temperature, but also pain, is transmitted to the brain via this nerve.
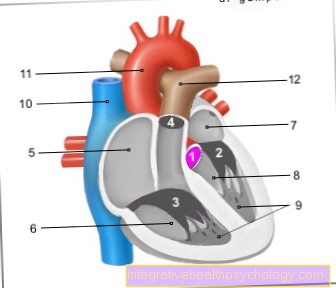
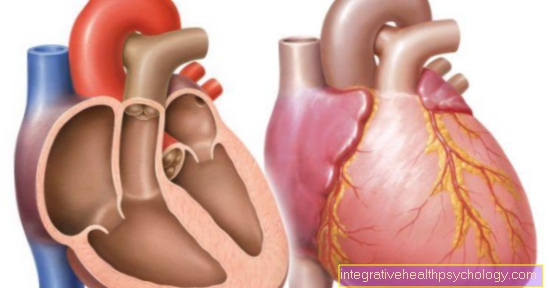
The cause of trigeminal neuralgia can be too close contact between the nerve and blood vessels: the rhythmically repetitive expansion of the vessel produced by the heart leads to a breakdown of the nerve sheath surrounding the nerves over time. This makes the nerve inappropriately sensitive and sends violent pain signals to the brain, even though there is actually no reason to do so.
It is therefore typical that the pain attacks are triggered by facial movements such as Chew. Since the face is constantly in motion, such as when talking or smiling, trigeminal neuralgia with its shooting, violent attacks of pain often represents a high psychosocial burden for those affected, which can lead to secondary diseases such as high blood pressure or depression.
Conservative (drugs such as carbamazepine) and surgical (inserting a Teflon layer between the vessel and nerve) options are available for therapy.
Read more on the topic: Trigeminal neuralgia
Neuralgia on the head or scalp
Neuralgia on the head or scalp is often associated with an enormous amount of suffering in those affected. The smallest movements or touches of the head trigger extreme pain. Combing your hair, moving your face or even putting on an item of clothing becomes a real ordeal.
The cause is irritated or damaged nerves. The background can be more or less serious and therefore more or less treatable. A strong cold stimulus or too tight-fitting headgear are causes of painful nerve irritation that can be quickly resolved.
Real diseases that require significantly more complex treatment and are usually associated with a protracted course of the disease are special neuralgia such as trigeminal or occipital neuralgia and shingles.
Trigeminal neuralgia occurs on the face and forehead, while occipital neuralgia refers to nerve pain in the back of the head. Both diseases are often of unknown cause, since the nerve damage itself or the reason for it cannot be found. The therapeutic approaches are varied and range from conventional medical measures to alternative medicine. With some patients acupuncture helps, with others affected an improvement of the symptoms is achieved through a medication.
Shingles usually appears in a belt shape on the torso of people who have had chickenpox once in their life and who have the virus that breaks out again. After the initial infection, the virus settles in a nerve node and remains there for life. If the virus is located in a nerve node in the head, the scalp may also be affected by the rash and neuralgia that the virus characteristically causes. Shingles can only be treated symptomatically. Drugs against epilepsy such as carbamazepine, because they reduce nerve excitability, and strong pain relievers provide relief. These include opioids such as tramadol and oxycodone, which, however, have a certain potential for dependence and should therefore only be taken with care.
Read about this too Burning in the head
Neuralgia on the back of the head
Neuralgia-like pain in the back of the head is usually the result of occipital neuralgia. Occipital nerves are affected, which are responsible for transmitting pain signals from the skin of the back of the head to the brain. For many of those affected, the shooting pain attacks are primarily triggered by turning their head.
The cause of the damage to the nerve can be, for example, a fall on the back of the head or tension in the neck muscles. Often, however, no specific cause can be determined.
Treatment essentially includes pain medication and carbamazepine, as well as physiotherapy and massages to relieve possible neck tension. In rare cases in which a herniated disc in the cervical spine is the cause, surgery can also be considered.
Meralgia paresthetica
This cumbersome technical term describes the complaints that result from compression of the nerve that is responsible for transmitting pain and contact information from the lateral thigh. On its way from the skin of the thigh to the spinal cord, the nerve runs under the inguinal ligament, among other things, where there is an increased risk of pinching the nerve. Risk factors for such a so-called bottleneck syndrome are obesity, diabetes mellitus, Professions with predominantly standing work as well as intensive strength training of the thigh and hip muscles.
Burning nerve pain and tingling sensations on the lateral thigh are typical of Meralgia paresthetica, which often improve when the hip joint is bent (i.e. the leg is lifted). In more advanced stages, numbness can also occur, on the other hand touch can become so painful that even wearing pants is perceived as extremely uncomfortable. In the treatment of meralgia paresthetica, the elimination of risk factors is of great importance, and pain medication is also used.
The nerve can also be immobilized by injecting local anesthetics and glucocorticoids (cortisone). If none of these measures lead to a satisfactory improvement, surgical decompression of the nerve can be considered.
Read more on the topic: Meralgia paresthetica
Intercostal neuralgia / intercostal neuralgia
Nerves called intercostal nerves run between the ribs. These nerves can also be damaged and trigger a neuralgia, an intercostal neuralgia.
The belt-shaped pains are characteristic of the chest or back area (nerve pain in the back) and are of a persistent form. Due to pressure increases in the chest, e.g. coughing intensifies the pain like an attack and describes it as very intense by patients. Due to the localization on the chest, which many people associate with problems of the heart or the lungs, additional breathing difficulties and anxiety attacks often occur. Sensory disturbances in the nerve supply area can also occur.
Intercostal neuralgia is more of a symptom than a disease in itself. Such neuralgia can occur in many different diseases of the spine, rib bones, pleura or lungs. Shingles can also develop intercostal neuralgia. In rare cases, the nerve pain is triggered by diseases of the spinal cord, aortic narrowing or tumors.
In the diagnosis, care must be taken that no disease other than intercostal neuralgia is misinterpreted. Problems with the heart, stomach, liver or gallbladder can also trigger similar pain symptoms.
Read more on the topic Intercostal neuralgia
Neuralgia on the back
Various diseases can lead to nerve-related back pain.
These include degenerative (wear-related) changes in the spine or herniated discs. Both can result in the spinal cord or the nerve roots becoming trapped and thus damaged.
In addition to the neuralgic pain, there are often also neurological functional restrictions (e.g. numbness, disorders of movement coordination).
Another possible cause is shingles, or so-called herpes zoster. This usually occurs as a result of a weakening of the immune system, e.g. by a flu-like infection, to a reactivation of herpes viruses, which then spread along a back nerve. Here, the neuralgic pain is usually accompanied by a vesicular rash on the trunk.
Read more on the topic: Nerve pain in the back
Neuralgia in the genital area
If the genitofemoral nerve is damaged or irritated in a man, attack-like, shooting pains occur in its innervation area. This results in attack-like pain in the groin and scrotum.
Would you like to learn more about this topic? For detailed information, see: Spermatic neuralgia
Neuralgia in the feet
A sore foot puts a lot of stress on the person concerned and is usually caused by injuries of various kinds.
However, the pain can also have a nerve cause. Since in many cases this form of pain can only be relieved to a limited extent by classic pain medication, the cause of the nerve damage should be treated first.
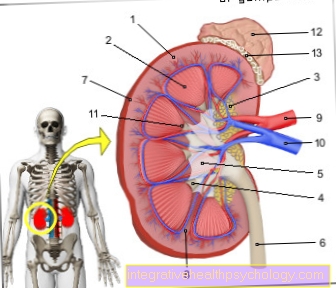
The most common cause of nerve pain in the foot is diabetic neuropathy. Longstanding diabetes mellitus, which is common to many older and overweight people, first causes damage to the vessels in the outer parts of the body. On the one hand, the nerves are damaged by the subsequent insufficient supply, which then triggers pain, on the other hand, the increased blood sugar level itself also causes damage. In the foot, nerve injuries or irritations are often triggered by bruises. These arise, for example, from wearing tight shoes or from unnatural foot positions, i.e. through wearing high heels. This is also the reason why young women are particularly plagued by such a pain syndrome. A flat shoe model with enough freedom can already lead to an alleviation of the symptoms, whereby the nerve needs time to recover.
The neuralgia can also be triggered by a so-called tarsal tunnel syndrome. This is a syndrome that is caused by compression or constriction of certain nerves in the leg.
Another more common form of neuralgia is Morton's neuralgia. At the beginning, those affected usually report sensory disorders such as tingling or falling asleep of the feet and especially the toes. Later, there are recurring, shooting pains and sometimes radiating pains into the leg. The mechanism of development of this disease is based on a compression of the foot sole nerves between the heads of the metatarsals. Over time, this stress on the nerve can lead to the formation of new connective tissue around the nerve, which is supposed to protect the nerve. Although this is “well meant”, it almost always leads to an additional entrapment of the nerve. The diagnosis can usually be made relatively reliably based on the symptoms described and the physical examination and is confirmed by an ultrasound or MRI examination.
Read more about the topic here: Morton's neuralgia.
Post-zoster neuralgia
For shingles (Herpes zoster) herpes viruses reactivate, which then attack a spinal cord nerve, usually as a result of a weakening of the immune system, for example in the context of a flu-like infection. The typical rash on the trunk usually disappears within 2-3 weeks with adequate treatment, but the characteristic pain persists for months afterwards in some sufferers (approx. 10-20%). These complaints are based on damage to the nerve by the herpes viruses and are known as post-herpes neuralgia.
For most of those affected, it manifests itself as a burning constant pain, which is supplemented by recurring, shooting, electrifying pain attacks.
Therapy for post-herbal neuralgia is usually medicated. Antidepressants such as amitriptyline or anticonvulsants such as gabapentin have proven effective, and pregabalin is also often used successfully. In addition, pain-relieving gels with locally anesthetic ingredients (especially lidocaine) can be used. As is so often the case, however, the best therapy is prevention: early and adequate treatment of shingles can significantly reduce the risk of developing postherpetic neuralgia.
Read more about this on the main page Shingles
Is there also a psychosomatic neuralgia?
This question can be answered with a “yes and no”.In a narrower sense, neuralgia actually describes a disease in which damage to a nerve leads to characteristic pain attacks. Consequently, according to this definition, there can be no psychosomatic neuralgia.
Nevertheless, there are psychosomatic illnesses in which attack-like, shooting pains occur, which can hardly be distinguished from those of "real" neuralgia. For this reason, it is not entirely wrong to speak of psychosomatic neuralgia.
The distinction is important for the treatment: In psychosomatic neuralgia, learning relaxation techniques and psychotherapy play an important role, which is not the case with organic neuralgia (i.e. when there is a clearly demonstrable trigger such as a herniated disc).
What is the difference between neuralgia and neuritis?
Even if the terms neuralgia and neuritis are sometimes used synonymously, there are some differences in their meaning. Neuritis is initially just the technical term for an inflammation of the nerves. As a rule, it manifests itself in persistent, pulling, increasing and decreasing pain.
Neuralgia, on the other hand, describes a disease in which damage or irritation of a nerve leads to nerve pain. Since inflammation is one of the possible causes of nerve damage in addition to mechanical irritation, the neuralgia can therefore be the result of neuritis.
As a rule, however, in contrast to neuritis, neuralgia manifests itself in the form of recurring, shooting attacks of pain lasting a few seconds to a few minutes.
Read more on the subject at: Duration of an inflammation of the nerves - what you should be aware of!
therapy
Before a therapeutic measure can be selected, extensive diagnostics should be carried out in order to rule out other diseases and to locate the affected nerve.
The treatment of neuralgia does not lead to freedom from pain in all those affected. The German Pain Society has developed certain therapy goals that are intended to guide the treatment. The aim is to reduce pain by 30 to 50%, improve the quality of life and sleep, and ensure participation in professional and social life. Before starting therapy, the patient should first change their way of life, largely avoid alcohol and cigarettes, allow themselves enough rest and avoid stress and illnesses.
One way of treating nerve pain is through a drug setting. Various pain relievers, anti-depression drugs, antidepressants and epilepsy drugs, so-called anticonvulsants, are used.
Strong pain relievers, such as morphine, are used for attack-like pain. The use of antidepressants and anticonvulsants makes sense because they intervene at different points in the development of pain. Anticonvulsants reduce the excitability of the nerves and thus lower the pain threshold, while antidepressants influence pain processing. Often a combination of the different drug groups makes the most sense.
Other treatment approaches are physiotherapy and osteopathy, which start with the musculoskeletal system and try to relieve tension or bad posture. Thus, the irritation of the affected nerve can be relieved and the pain can be alleviated.
Alternative medical methods also have many supporters in the therapy of nerve pain. For example, some doctors use acupuncture or homeopathy to treat the causes of the neuralgia or the pain themselves. Acupuncture in particular can relieve tension that irritates the nerve.
In the rarest of cases, surgical treatment of the neuralgia is necessary or even possible. Severing or irradiating nerves is tricky as all functions of the treated nerve can be lost. Only in the case of trigeminal neuralgia is an operation used comparatively often, since the patient's suffering can barely be reconciled with the consequences of the operation.
Homeopathy for neuralgia
Even from the point of view of experienced homeopaths, neuralgia must primarily be treated by a doctor. However, he can use the homeopathic natural remedies as a supportive therapy element.
A herbal remedy that has already proven itself in the therapy of mild depression is St. John's wort. This is taken in the form of a capsule or applied as an oil to the painful areas. Other herbal remedies that can be used for neuralgia are Cantharis (Spanish fly) and Cedron (bitter ash family).
Cyclamen (cyclamen) and Verbascum (mullein) are supposed to help with trigeminal neuralgia. Certain Schüssler salts are also said to have a healing effect on neuralgia. This concerns the salt Calcium phosphoricum (No. 2) and Ferrum Phosphoricum (No. 3), the salt Kalium phosphoricum (No. 5), as well as the salts Magnesium phosphoricum (No. 7) and Silcea (No. 11).
In addition to herbal remedies, many homeopaths recommend various relaxation techniques, as patients with neuralgia often suffer from stress. Possibilities are yoga, autogenic training or meditation.
Construction therapy is often mentioned in the treatment of neuralgia, but is not recommended from a conventional medical point of view. In this form of therapy, tiny wounds are stabbed in the skin with needles, and various oils and solutions are then applied to the skin. The skin and the surrounding tissue should therefore be supplied with more blood, but through the wounds many germs can penetrate and cause infections.
Read more on the topic Homeopathy for nerve pain
diagnosis
Before the diagnosis of neuralgia is made, the patient often goes through a wide variety of diagnostic methods. First of all, all other causes that could be responsible for a pain in the affected area are excluded. For this purpose, both neurological and physical examinations as well as imaging procedures such as X-rays, CT or MRT are carried out.
Sensitivity and muscle strength, reflexes and pain perception are tested. The latter is attempted with the help of questionnaires and drawings, whereby an objective assessment is complicated. This is compounded by the fact that the extent of a pathological change does not have to correlate with the patient's subjective pain perception.
Pain is a sensation that is much influenced by each patient's experience and personality. Neuralgia cannot be diagnosed like a broken bone. Many different factors come together here, which, however, when combined as a whole, produce a relatively reliable picture. Through targeted examinations, the correct treatment path can therefore also be taken in the case of diagnostically complex neuralgia.
What are the symptoms of neuralgia?
Neuralgia is characterized by characteristic pain symptoms. The pain occurs only in the supply area of the affected nerve and is also triggered by this.
The pain symptoms can occur in the form of permanent pain or attacks and are often accompanied by paresthesia and tenderness of the surrounding muscles.
Hyperesthesia, i.e. excessive sensitivity to pain, and in rare cases allodynia are particularly typical. This describes the perception of pain in the case of non-painful stimuli such as touch.
The form in which the pain occurs in neuralgia is usually described similarly by a wide variety of patients. Those affected are the first to report an unnaturally strong experience of pain that has never occurred before. The medical term "annihilation pain" is often used as a synonym for this worst possible pain stimulus.
If the symptoms consist primarily of persistent pain, in many cases these are perceived as burning or piercing.
Pain peaks are more likely to be reported in attack-like nerve pain. These sudden onset of pain attacks are described as electrifying and stabbing. Patients are overwhelmed by the pain and are often unable to do anything else at the moment of the most severe pain experience.
The primary pain symptoms can result in secondary symptoms. These are not caused by the neuralgia, but are increasingly developed as part of the disease. Classic side symptoms are difficulty concentrating and tiredness.
Because of the pain, which can also occur at night, the body does not get the rest it needs. On the one hand, this causes permanent tiredness in the patient, on the other hand, the difficulties in concentrating, which already exist due to the severe pain, are exacerbated. Another, often serious side symptom, is depression. Due to the constant suffering and the reduced quality of life, which is often caused by the pain symptoms, those affected can get into a depressive episode that should be observed and treated.