Patellar tendon rupture
introduction
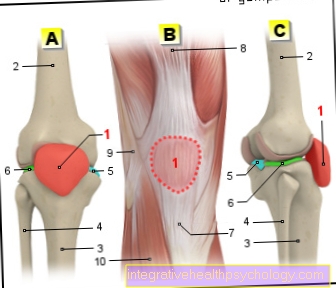
A crack (Rupture) the tendon between the lower pole of the kneecap (Patella) and the tibia (Tibial tuberosity) is known as a patellar tendon rupture. The tendon can tear as a result of various forces.

The patellar tendon rupture is one rare injurywhose faulty or incorrect treatment could lead to permanent damage or further cracks.
Younger people are most often affected by a patellar tendon rupture, which occurs in everyday life high level of mobility and activity expect, which is why the rupture must be treated medically in any case. With proper treatment, the prognosis for a patellar tendon rupture is generally very good.
anatomy
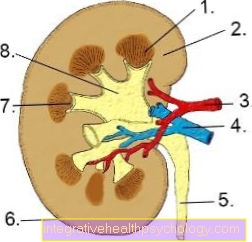
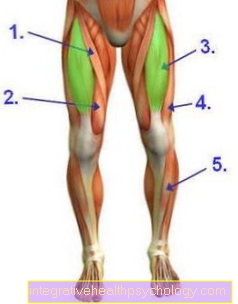
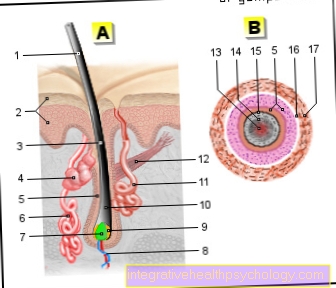
The four-headed thigh muscle (Quadriceps femoris muscle) on the front of the thigh, extend the leg in the knee joint. The four muscles end in which the kneecap is embedded and which extends to the shin. Below the kneecap, this tendon is also called the kneecap ligament (Ligamentum patellae) designated.
The tendon fixes the kneecap and serves as a central pivot point (Hypomochlion) when flexing the knee joint. The majority of the tendon fibers come from the end tendon of the rectus femoris muscle, one of the four thigh muscles. These fibers also radiate into the kneecap and partially cross it.
On the side of the patella are fibers of the other three muscles (Musculus vastus medialis, Musculus vastus lateralis, Musculus vastus intermedius)that tend to slip past the kneecap. The patellar tendon is absolutely necessary for a powerful extension in the knee joint.
Appointment with a knee specialist?
I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
The knee joint is one of the joints with the greatest stress.
Therefore, the treatment of the knee joint (e.g. meniscus tear, cartilage damage, cruciate ligament damage, runner's knee, etc.) requires a lot of experience.
I treat a wide variety of knee diseases in a conservative way.
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
Further information about myself can be found at
Patellar tendon rupture
The rupture of the patellar tendon can be caused by indirect or direct forces. The rupture of the patellar tendon is usually caused by an over-tension trauma against resistance or a strong tension in the flexion of the knee joint.
Such an accident mechanism is particularly common in sports such as tennis or skiing. Due to the relatively small lever between the pivot point of the knee joint and the kneecap, the patellar tendon has a very large cross-sectional load, in heavy people up to over 1000 kg / cm².
In rare cases, cortisone injections into the knee joint can rupture the patellar tendon.
It is assumed that a tendon that has not yet been damaged will only tear in the rarest of cases. The likelihood of a patellar tendon rupture increases with existing previous damage.
Previous degenerative damage can be found, for example, in people with Ehlers-Danlos syndrome, butterfly lichen (Lupus erythematosus), Chronic renal failure, diabetes (Diabetes mellitus), arterial occlusive disease or after surgical measures.
In adulthood, patellar tendon ruptures are most commonly found at the transition from the lower pole of the kneecap to the tendon, as this appears to be an anatomical weak point.
Often the patellar tendon rupture is also combined with a bony tendon tear, which means that a bone fragment of the kneecap breaks off due to excessive tension on the tendon.
In children and adolescents, a patellar tendon rupture usually occurs further down near the point of attachment of the tendon on the shinbone (near the Tibial tuberosity) on.
Direct violence, for example cuts or tears, can also tear the middle of the patellar tendon.
Occasional rupture can also occur due to patellar tendon irritation.
diagnosis
Three symptoms are very typical of a patellar tendon rupture. On the one hand, active knee extension is restricted and the kneecap protrudes a little upwards (Patella elevation).
On the other hand, you can feel a dent at the rupture site (palpate)which is usually palpable despite the bruise that forms.
Frequently, the kneecap can also be observed "wandering up" when the knee is flexed or when the thigh muscles are tensed, since the patella is no longer fixed to the shin bone by the torn patellar tendon.
Since the leg can no longer be actively and powerfully stretched, the affected extremity is unable to bear weight. In contrast to an Achilles tendon rupture, for example, those affected often complain of severe pain with a patellar tendon rupture, as there is often a torn tendon.
An X-ray is a good way of assessing the extent of the patellar tendon rupture, and a bony tear can also be clearly seen on an X-ray.
The diagnosis is confirmed by an ultrasound examination of the tendon.
In some cases, additional imaging tests may be required (MRI, magnetic resonance from the knee) be helpful, for example if there is a suspicion of accompanying damage to the knee joint or only part of the patellar tendon is torn (Partial rupture).
The symptoms of a (rare) patellar tendon rupture may match the symptoms of a much more common patellar fracture (Fracture of the kneecap) in which there is also a loss of extensibility in the knee joint.
In addition, in the event of a fracture, the kneecap can also be felt upright.
A lateral x-ray of the knee joint enables the two diagnoses to be reliably differentiated. This also excludes quadriceps tendon rupture, which usually manifests itself as a low kneecap with an acute extension deficit in the knee joint.
ICD-10
In the ICD-10 classification, the patellar tendon rupture is assigned the code S76.1.
therapy
The pain and swelling associated with an acute patellar tendon rupture should be treated with ice and the leg should be raised.
A complete tear of the patellar tendon should always be treated surgically, except in the case of extensive accompanying injuries or acute danger to the person's life. In these cases, after the affected person has been adequately stabilized, an operation of the patellar tendon rupture is recommended in order to restore good knee joint function in the long term.
Without surgery, only strains of the patellar tendon or small tears can be treated, which do not lead to any relevant weakening of the patellar tendon. The rupture can be located centrally in the tendon area as well as at the tip of the kneecap or at the base of the tibia.
Depending on the location, a tendon suture is carried out, near the bone this is fixed in the bone with a suture anchor.
In addition to the direct suture of the two tendon ends, a twisted wire is used (Wire cerclage) between the kneecap and the tibia, the so-called McLaughlin cerclage.
This wire completely relieves the suture of the patellar tendon, which enables functional treatment of the knee joint at an early stage after the operation. The wire cerclage can usually be surgically removed after three to six months.
The wire cerlcage very often tears during the functional post-treatment, in which case the material should be removed early.
The operation of the patellar tendon rupture is usually performed under general anesthesia and takes about 30 to 45 minutes.
The surgery can cause complications like bruising (Hematomas) and superficial infections occur.
Surgical technology
In the operation of a patellar tendon rupture, the goal is to completely restore the extension of the leg and the load-bearing capacity.
The patellar tendon consists of the terminal tendon of the thigh muscle (Quadriceps femoris), which connects the patella with the shin. The tendon attaches to the tibial tuberosity.
During the operation, the torn tendon parts are reconnected. A cut is made below the knee so that the tendon can be displayed. A hole is drilled in the kneecap and in the shin for optimal stability. These holes are connected using different wires (cerclage or Labitzke) or a transosseous suture and thus the patella is fixed in its correct anatomical position. The end links of the tendon are then sewn back together. Once optimal stability and functionality have been ensured, the wound is closed. If necessary, a drain is inserted to treat secondary bleeding.
After the operation, a splint is put on and weekly rehabilitation training is recommended.
Follow-up treatment and prognosis
After every surgical treatment of a patellar tendon rupture, it is necessary to immobilize the knee joint. Tendon tissue is not well supplied with blood, which requires a long healing period.
Immobilization is possible, for example, with the help of an extension orthosis or a thigh tutorial splint. A stretch orthosis is a mostly padded splint made of aluminum that keeps the knee stable and fixes it at a preset knee flexion angle.
A thigh tutorial splint is also used to immobilize the knee joint in which a plaster cast is applied from the ankle to the groin at a certain knee flexion angle.
With the extension orthosis on, the leg can be fully loaded again immediately after the operation, but only knee flexion of up to 30 degrees is recommended for the first two weeks after the operation.
The angle is then increased to 60 and 90 degrees for two weeks. From around the seventh postoperative week, knee training can also be carried out without a splint.
An early follow-up treatment, in which the function of the knee joint can be restored, is made more difficult by the immobilization.
Nevertheless, mobilization and strength exercises should be carried out at an early stage in order to avoid complications.
Immobilization also increases the risk of thrombosis or embolism and, in the further course, possibly muscle wasting (Atrophy) of the quadruple thigh muscle and soft tissue damage from the splint can be observed.
Here, intensive physiotherapy serves primarily to prevent thigh muscle wasting and to maintain the mobility of the knee joint.
Often there is a restriction in knee extension, which can usually be remedied through active physiotherapy exercises.
Consistent therapy and follow-up treatment of the patellar tendon rupture is necessary for a favorable prognosis. In most cases, however, the function of the stretching apparatus can be fully restored. If the knee is put under full load too early, this can have a negative effect on the healing process, which can tear the cerclage wire. A wound infection after the operation can also prolong the healing process. Renewed ruptures of the tendon can occur, especially with degenerative pre-damaged patellar tendons. If the patellar tendon rupture heals without complications, you can later play actively without any problems.