Epidural anesthesia at birth
definition
An epidural anesthesia (PDA) is an anesthetic of the abdominal and pelvic area, which is used on request during the birth, especially in the case of severe pain in the birth. In contrast to spinal anesthesia, the anesthesia does not completely switch off the motor functions, which means that the patient can usually still move her legs, albeit with restrictions. With PDAs, the anesthetic is injected into the epidural space, the space between the vertebral bodies and the hard skin of the spinal cord, and thus not directly into the spinal cord or the spinal fluid.
You might also be interested in: How can birth pains be alleviated?

When should the epidural anesthesia be applied before the birth?
The PDA is usually put on at the request of the expectant mother. In most cases, the decision can be made spontaneously if the pain of labor is unbearable for the patient. However, it makes sense to at least inform the doctor about the risks and process before the onset of labor or at the beginning of the labor activity if a PDA is an option. In this way, the information can be explained in a more relaxed environment and questions can be clarified and the anesthesia can be set quickly in an emergency.
The prerequisite for placing the PDA is that the patient can hold still for several minutes despite contractions. The entire PDA procedure takes an average of 10 minutes. A pause in labor is used to insert the catheter to ensure that the patient is relaxed and not moving. Since the effect occurs after a few minutes and reaches its maximum after about 15 minutes, the PDA can theoretically be used at any time before the birth, as long as the actual birth process (expulsion phase) has not yet started.
You might also be interested in: Birth from breech position
What are the risks for my child?
As with any anesthetic that the patient takes during pregnancy and childbirth, the anesthetic in the PDA also enters the child's bloodstream via the umbilical cord and placenta. This can lead to the baby being more sleepy after birth than children born without an epidural. As a rule, however, the PDA is well tolerated by the newborn and has fewer side effects than, for example, general anesthesia.
Since births under the PDA take a little longer on average, the birth itself can be more stressful for the child. In addition, a PDA makes it difficult for some children to turn into the correct birth position, so that more so-called “stargazers” are born, children who are born face up instead of down.
This birth position can lead to bruises in the child and the birth must be supported more often than in the normal position using a suction cup or forceps. This can also lead to bruises and swelling, especially in the child's head area, which in most cases will disappear after a few days.
What are the side effects for me?
The most common side effect in the patient is a drop in blood pressure. This comes about by widening the vessels in the anesthetized area. To prevent this, an infusion can be attached and the blood pressure is checked regularly. A PDA can therefore be dangerous for patients with previous heart diseases, but the personal risk should always be discussed with the doctor.
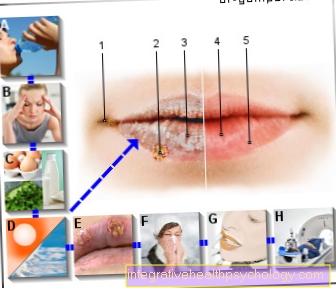
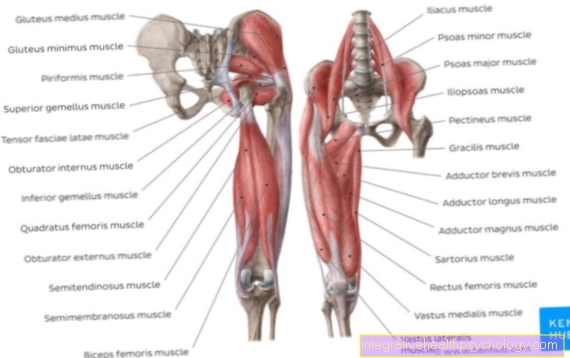
In addition, headaches can occasionally occur. This is caused by pushing the needle too far forward and thus damaging the hard skin of the spinal cord (Dura mater) and leakage of cerebrospinal fluid. If the injury is not noticed and the anesthetic is injected into the spinal space, spinal anesthesia can inadvertently result, in which the entire motor function of the abdominal and leg muscles is switched off.
In rare cases, a spinal cord or nerve injury can occur. Since the PDA is placed very far below the end of the spinal cord in obstetrics, this complication is unlikely.
A bruise can also occur at the puncture site. If a vein is struck in the epidural space during the procedure, bleeding can occur in it. The resulting pressure can damage the spinal cord.
You might also be interested in: Complications of an epidural anesthesia
Is delivery painless with an epidural?
The birth under a PDA can take place without pain. The doses of anesthetic required for this usually also severely limit the mobility of the legs, so that the patient cannot walk around on her own. In addition, if you are completely free of pain, you can no longer feel the contractions.
This means that the woman does not feel the natural urge to push during the expulsion phase, making active cooperation more difficult. For these reasons, the anesthetic is usually dosed a little lower in a PDA, so that the birth is not completely painless.
The aim, however, is to reduce the pain to such an extent that it remains at a tolerable level for the patient and she can rest better in the opening phase.
You might also be interested in: Birth pains
Common side effects of PDA in childbirth
Common side effects with the PDA are a slight drop in blood pressure, especially in the first half an hour after applying the PDA. This can lead to dizziness and nausea. About 23% of women get a fever from the PDA. It can also lead to a slowed pulse. This is why the patient is monitored by a doctor, especially in the initial phase.
In addition, urination may be difficult because the bladder area is numbed. It may therefore be necessary to insert a urinary catheter in order to empty the bladder. This can lead to infections, especially of the bladder.
Numbness and tingling in the legs are also relatively common.
If the hard skin of the spinal cord is injured by the needle and liquor escapes, it can lead to severe headaches that last for several days.
Disadvantages of a PDA at birth
One difference to births without anesthesia and narcotics is that the birth process takes longer on average for a birth with a PDA. This is primarily due to the fact that the mother-to-be can no longer perceive the rhythm of labor and pressure exactly and the ideal time to press and thus promote the birth is not used.
It also happens more often that the child does not turn into the correct birth position and is born face up instead of face down. On the one hand, this can lead to bruises in the head area of the child and, on the other hand, it is a situation that often has to be supported with forceps or the suction cup. This obstetrics can lead to vaginal injuries in women and often has to be supported by a perineal incision.
An epidural does not increase the risk of needing a caesarean section. However, if a caesarean section is necessary, general anesthesia can often be dispensed with and the PDA can be dosed higher so that the mother can consciously experience the birth and then take the child in her arms.
Back pain after childbirth after PDA
Back pain after giving birth with epidurals is no more common than after giving birth with other pain relieving medications. However, slight pain can cause bruises at the puncture site after the PDA has been placed, but these will subside after a few days.
Duration of an epidural at birth
The preparation of the PDA and the placement of the pain catheter usually take 10 minutes with good cooperation from the patient. However, since in most cases a pause in labor is waited for the actual puncture so that the woman can hold still, it can take a few minutes longer to sit down.
The analgesic effect of the anesthetic already sets in after a few minutes, and it reaches its maximum after about 15 minutes. The effect usually lasts 2-3 hours, the anesthesia subsides completely after 4 hours at the latest. In order to ensure a longer effect during labor, which often lasts longer, a catheter is therefore usually inserted, through which pain medication can be injected at any time as required without having to perform another procedure. In this way, the duration and strength of the anesthetic can be individually adapted to the needs of the patient.
Prepare for the PDA
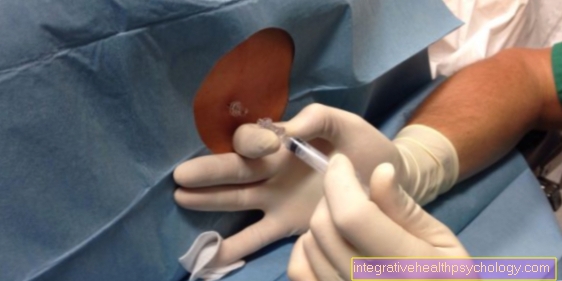
The PDA is put on while sitting or lying on the side. The skin is disinfected and the puncture site is locally anesthetized so that the puncture itself can hardly be felt. Ask the patient to arch her back and relax her shoulders.
Process of the PDA
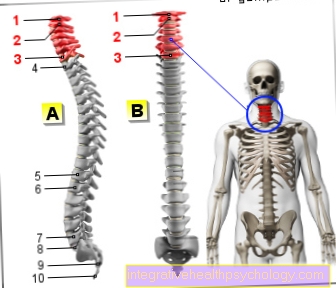
In the lower area of the spine, the point between two spinous processes is palpated and a hollow needle is inserted there, which is connected to a syringe filled with liquid.
If this liquid can be injected without resistance, the ligaments between the vertebral bodies have been passed and the syringe is located in the epidural space, i.e. between the vertebral bodies and the hard skin of the spinal cord. Then a small tube, the catheter, is inserted through the hollow needle, through which the painkiller can be administered at any time. The needle is removed and a bandage is applied. The procedure is usually not painful and most of the time only pressure is felt in the back area when the needle is inserted. The first dose of pain medication is usually a test dose, a small amount of pain medication, to test the effect on the patient. It also looks at a response in blood pressure and its effects on mobility. If everything is normal, a larger amount of anesthetic can be administered.