Portal hypertension
Synonyms in a broader sense
Medical: Portal hypertension
Liver, Cirrhosis of the liver
Definition of portal hypertension
Portal hypertension (portal hypertension) is the chronically increased pressure in the portal vein (vena portae) above a certain limit value.
This increase in pressure is caused by an obstruction of the blood flow through the portal vein or the liver, which can have various causes. In 80% of cases, however, cirrhosis of the liver is the cause, which in turn is caused in most cases by alcohol abuse.
Cause of the disease
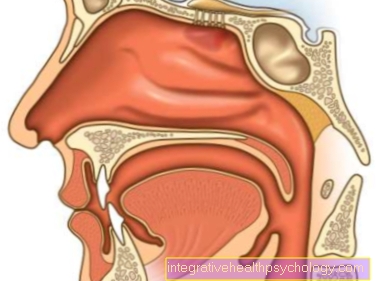
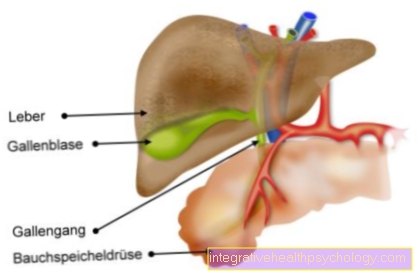
The portal vein (Vena portae) transports the venous blood from the digestive organs of the gastrointestinal tract to the liver. This venous blood is low in oxygen, but contains (after meals) all the substances absorbed (nutrients, medication, etc.). The liver now has the task of storing or converting the nutrients and disposing of toxic substances.
If pathological processes (e.g. liver cirrhosis, viral hepatitis, thrombosis) obstruct the blood flow through the liver, the blood inevitably builds up in the supplying blood vessels, which leads to an increase in blood pressure (high blood pressure). This phenomenon is known as portal hypertension.
Liver disease is not always the cause. In the so-called congested liver, blood backs up in the liver because, in the context of a right heart failure, the blood cannot be pumped into the pulmonary circulation and therefore backs up into the liver. In this case, heart failure is responsible for the increase in portal pressure.
Learn more at: Congested liver
Although two different vessels supply blood to the liver (the hepatic artery with oxygen from the aorta and Porta vein with nutrients from the Gastrointestinal tract), only the increase in pressure in the portal vein is fraught with complications, since in the portal vein, as in all veins, a significantly lower one Blood pressure than prevails in arteries and thus significantly greater effects can be triggered by slight pressure differences. Due to the congestion and the subsequent increase in pressure in the portal vein reverses the direction of blood flow. The blood looks for another drainage route to the right one heart to get. There are smaller connections between the entrance area of the portal vein and other veins that flow directly into the right heart (the so-called portacaval anastomoses). As with a traffic jam on the road, these alternative routes are not designed to cope with the increased load and are therefore typical Complications.
Complaints / symptoms

- hemorrhoids
A bypass route leads through the venous plexus of the anus. This venous plexus flows both into the portal vein and via the lower one Vena cava (Inferior vena cava) straight into the right heart. If too much blood chronically flows through the plexus of small veins due to portal hypertension, they widen excessively. They then protrude into the intestinal canal and burst easily (hemorrhoids). This is very painful for the patient, he loses venous blood here blood (dark red color). There is another, more common, form of hemorrhoidsthat may develop due to weak connective tissue and veins. In this case, however, it is arterial, i.e. oxygen-rich blood, which is bright red in color.
- Esophageal variceal bleeding
Also the veins of the esophagus (Esophagus), connected by the venous plexus of the stomach, form a possible escape route. Here, too, the chronic overload leads to swelling of the veins, which gradually tear. The tearing is promoted by the strong mobility of the esophageal wall during the transport of food into the stomach.
When the vessels are damaged, the blood is lost through the esophagus and thus through the digestive tract. This is life threatening for the patient as he seldom realizes that he is bleeding here. On the long way through the intestines, the blood coagulates, turns black from the stomach acid and mixes with the stool. This causes blood to be lost unnoticed (occult bleeding), often in large quantities. The patient becomes anemia (anemia), the cause of which is not so easy to find.
An important method is the use of a hemoccult test strip. The patient has to place a little stool on the test strip. If there is clotted blood and thus the blood pigment hemoglobin in the stool, this can be seen on the test strip.
You can find out more about this at Esophageal variceal bleeding.
- Medusa head (Caput medusae)
Another bypass route is through smaller veins in the skin of the abdomen near the navel. These veins also flow into the right heart via the inferior or superior vena cava. In case of Portal hypertension wear them out and become visible. Their appearance is reminiscent of the ancient shape of the Medusa head. In contrast to the other bypass routes, there are no life-threatening complications here.
Diagnosis of portal hypertension
For the detection of portal hypertension one cannot orientate oneself directly to the definition, since one cannot do the locally in the portal vein Measure blood pressure can. Rather, the diagnosis is based on various other criteria. This includes proof of Bleeding in the esophagus (Esophageal varices) on an endoscopy, evidence of a Slowing of blood flow in the portal vein by Ultrasonic, the Thickening of the spleen (Splenomegaly) also by ultrasound or the presence of free fluid in the abdomen (Ascites). Furthermore, efforts are made to prevent the disease causing portal hypertension (Cirrhosis of the liver, thrombosis), as this must also be treated.
Therapy of portal hypertension
First, you have to understand the reason for the Portal hypertension find that purely symptomatic therapy can only help in the short term. Depending on the cause of the underlying disease, the Alcohol consumption be stopped immediately, the thrombus dissolved, etc.
The bleeding from the esophagus must be acutely breastfed through an intervention with an endoscope and the administration of hemostatic drugs. Long-term attempts are made to use antihypertensive tablets (Beta blockers) to lower the increased pressure in the portal vein
The accumulation of free fluid in the abdominal cavity is initially attempted through rather unspecific measures such as reduced fluid intake, administration of drainage tablets (Diuretics) and limiting salt intake. As a further measure, the liquid can also be withdrawn with a syringe (puncture, therapeutic paracentesis).