Are polyps of the uterus dangerous?
introduction
Uterine polyps (uterine polyps) are benign changes in the lining of the uterus that are usually harmless. Polyps can appear at any age, and they are more common during or after the menopause. Many women are affected by polyps, but do not necessarily need therapy if they are free of symptoms. With adequate therapy, polyps can be completely cured.

Definition of polyps
The term "polyp" describes a swelling of the mucous membrane that is visible to the naked eye and which often grows stalky, sometimes over a wide area, into a hollow organ. In principle, polyps can be benign or malignant and occur, for example, in the uterus, intestines, stomach or sinuses. Uterine polyps are almost always benign and can be present in both the body of the uterus and the cervix.
Polyps on the cervix
When polyps of the uterus on the cervix, the so-called Cervix uteri, occur, one also speaks of cervical polyps. These are far more common than polyps in the body of the uterus. If they block the entrance to the uterus, they can sometimes cause problems. They can be an obstacle to childbirth or cause problems in getting pregnant. In addition, polyps of the cervix can lead to bleeding outside of the menstrual period. This type of bleeding is known as intermenstrual bleeding. In rare cases, large polyps can also lead to painful intercourse.
Can polyps of the uterus be cancerous?
Polyps are considered benign growths of the inner lining of the uterus. However, there is also a small risk (0.5%) that they can become malignant and develop into a tumor. Polyps of the cervix generally have a slightly lower risk of being malignant.
Because of this risk, polyps should be checked regularly for growth. If in doubt, they should be removed and examined with tissue (biopsy). In this way one can safely determine whether the polyps are benign or malignant tissue. In the event of intermenstrual bleeding and other complaints, removal of the polyp is generally recommended.
cancer

Polyps are initially benign growths of the uterine lining that often remain symptom-free for a long time. As with any cell proliferation, however, there is a small risk that a precancerous stage can develop in the course of the process. In general, polyps rarely lead to uterine cancer or cervical cancer. The growth of the polyps is dependent on the female hormone, estrogen, so that spontaneous growth can occur during the menstrual cycle with complete regression during the monthly bleeding. These polyps are harmless and cannot become malignant. However, all other polyps have the potential to become precancerous. In rare cases, a cancerous ulcer of the uterine muscles can hide behind it. Even benign polyps, depending on their size, can cause enormous discomfort, such as constant intermenstrual bleeding up to miscarriage or premature birth.
Removal of the uterine polyps is therefore recommended in younger patients. In older patients, the risk of an operation should be weighed against that of a malignant degeneration of the polyp. For the time being, a biopsy can be taken in a small operation to determine whether it is a benign or malignant growth. In the case of a benign finding, monitoring may then be sufficient.
If in doubt, you should always get a second opinion from another gynecologist who is very familiar with polyps. It is also important to know exactly where the polyps are. Polyps in the area of the cervix are almost always benign, whereas polyps in the area of the uterine body can degenerate and become a malignant cancer in every 2000th woman.
How dangerous are polyps in the uterus?
Polyps in themselves are not dangerous as they are benign growths that very, very rarely, become malignant.
therapy
If polyps are found in the uterus but are not causing symptoms, they do not necessarily need to be removed. The question of whether or not therapy should be given should be clarified by the doctor and patient after weighing the advantages and disadvantages. Most of the time, however, it is for safety reasons that the decision is made to remove the polyps from the uterus. An intervention becomes unavoidable if there is a suspicion of a precancerous stage or further pathological findings emerged during an examination.
Usually polyps can be removed with a scraping (curettage) are removed. This operation is performed under general anesthesia and, if necessary, can be combined with an endoscopy. If cancer is suspected in polyps of the uterus, a larger, conical piece of tissue is removed as part of a so-called loop conization. Depending on the results of the tissue (histological) examination, further treatments may then be necessary.
When is scraping indicated?
The scraping, which is also called Abrasion is used for diagnostic and therapeutic purposes.If polyps in the uterus cause discomfort, such as intermenstrual bleeding, discharge or pain, it is advisable to scrape them off. The polyps are removed and then examined histologically. The subsequent examinations under the microscope can determine whether the polyp was benign or malignant. Furthermore, one often carries out a fractional abrasion. This involves removing parts of the mucous membrane from the cervix and the uterine cavity individually and then examining them more closely. This procedure is also recommended for symptoms such as intermenstrual bleeding in order to determine the cause of the bleeding.
Read more on the subject at: Uterine scraping.
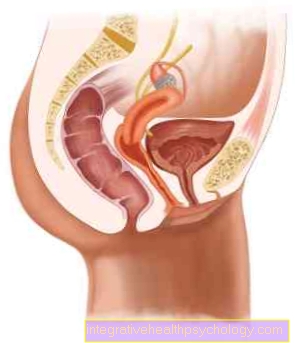
Figure polyps of the uterus

Polyps of the uterus
(Uterine polyps)
- Polyps - Polyposis uteri
- Uterine tip -
Fundus uteri - Fallopian tubes - Tuba uterina
- Uterine cavity - Cavitas uteri
- Uterine lining -
Tunica mucosa - Cervical canal -
Canalis cervicis uteri - Cervix - Ostium uteri
- Sheath - vagina
- Uterine body - Corpus uteri
- Cervix - Cervix uteri
Causes:
A - menopause
(during or after the menopause -
Change in hormonal balance)
B - mental stress
(Stress)
C - weakened immune defense
(other diseases, income
certain drugs)
D - Poor intimate hygiene
E - vaginal inflammation
or uterus with human
Papillomaviruses
You can find an overview of all Dr-Gumpert images at: medical illustrations
OP / removal

Polyps in the uterus (uterus) are initially benign growths of the mucous membrane. These are found in a large number of women of all ages, but particularly often in patients after and going through menopause.
Depending on when and with what symptoms the polyps appear, it can make sense to have them removed by surgery. Depending on the size of the polyp, it can be removed in different ways, often even a small operation is enough to remove the polyp from the uterus. If a gynecologist discovers a small, superficial polyp during a routine examination, he can remove it directly under local anesthesia and without major surgery. The procedure is comparable to removing a mole.
However, there are many gynecologists who cannot perform such an operation in their practice, or the polyps are too deep for such a removal. You can then be referred to a gynecological clinic, where the polyps are removed in a small operation. The operation is carried out on an outpatient basis, which means that after the polyps have been removed, the patient can leave the clinic after a few hours and does not have to stay there overnight.
During the operation, the patient is placed under general anesthesia so that he does not notice anything about the operation. Since this is a very short procedure of around 10-15 minutes, general anesthesia only numbs for a short time and has few side effects. During the operation, the doctor scrapes off the lining of the uterus and can thus remove the polyps. These can then be sent for a histological examination, which will now analyze whether the polyp is harmless or whether it is already cancer. With the help of a so-called hysteroscope, the gynecologist can take another close look at the lining of the uterus to see whether everything has been removed and the lining is now looking regular again. Since this is a short routine procedure, the patient can usually leave the clinic after a few hours. However, due to general anesthesia, side effects such as nausea or abdominal pain can occur, which may mean that the patient may have to spend a few days in the clinic until the symptoms have subsided and the patient feels able to go home go.
Surgery is not always indicated; small polyps in particular can initially only be monitored or treated with medication such as hormone preparations or GnRH agonists. However, surgery should be considered, not only because the polyps in the uterus can degenerate into cancer, but also because they can cause intermenstrual bleeding, pain during intercourse, or infertility. To avoid this, the patient is operated on.
Read more on the topic: Endoscopy
How long are you on sick leave after an operation?
After polyp removal or scraping, sick leave for a few days is common. How long you are on sick leave depends on various factors. In most cases, activities that are not physically stressful can be resumed after 2 to 3 days. In the case of physically demanding work, it can also be that you are on sick leave for 1 to 2 weeks. In addition to the activity performed, the length of the sick leave also depends on the general physical condition of the woman and the course of the operation. As a rule, these are minor interventions without complications. However, it can sometimes lead to increased bleeding or infections and increased pain. In these cases, a sick leave is issued until recovery.
homeopathy
If one wishes to take homeopathic remedies to treat polyps of the uterus, do so as soon as possible as soon as symptoms appear. The earlier you start taking, the better the chances of getting better. Various homeopathic remedies are recommended for supportive treatment. The homeopathic remedy Thuja recommended if the polyps cause pain during intercourse, Sanguinaria however, it is more effective on polyps that bleed easily. Another remedy is that Conium. This helps with polyps that cause sharp pain. In order to find the right homeopathic remedy for the individual complaints, one should seek advice from a pharmacist or alternative practitioner with experience.
course
The progression of polyps in the uterus is generally very good. If they are noticed at all by symptoms, then these can be completely eliminated in almost all cases in the course of an operation. In only a few exceptions, uterine polyps develop into malignant findings.
How fast do polyps grow?
Polyps mostly develop during menopause. Their growth goes unnoticed as it doesn't cause any discomfort. How long a polyp takes to complete its growth is not known. It can develop over a few weeks or several months. In addition, its growth is subject to hormonal influences, so that there can be a constant build-up and remodeling of the mucous membrane tissue.
size
Polyps in the uterus usually occur in women during menopause, i.e. the menopause, and can take on different sizes. Usually only one polyp develops, but it can also be that several (multiple) polyps accumulate in the uterus and take on different sizes.
Usually the polyps are only a few millimeters in size. The polyps count as small polyps up to 2 cm and are usually very easy to remove.
However, there are also polyps that grow stalk-shaped and significantly exceed 2 cm in length, but they very rarely become 5 cm or even larger. From this size at the latest, the polyps in the uterus cause clear symptoms and are therefore removed.
causes
Polyps ultimately result from the cells in the uterine lining dividing too quickly. However, why exactly this happens has not yet been conclusively clarified. The most important factor that affects cell growth is the female sex hormone estrogen. This is why women in particular are affected by polyps during or after the menopause, as a change in the woman's hormonal balance takes place at this time.
Other circumstances that can promote the development of polyps are psychological stress or stress, a weakened immune defense (for example due to other existing diseases or the use of certain medications such as cortisol), poor intimate hygiene or inflammation of the vagina or uterus with the human papillomaviruses.
prophylaxis

You cannot really prevent the development of polyps in the uterus. You can only switch off some risk factors, for example by avoiding the papillomavirus infection with the help of protected sexual intercourse or by strengthening the immune system. In addition, women should appear regularly for gynecological checkups, which means that the polyps can almost always be detected and treated at an early stage.
Symptoms
Polyps in the uterus often cause no symptoms at all and are therefore a chance diagnosis when an examination is carried out for another reason. Sometimes they are not detected at all, for example polyps are found in around 10% of all wombs that are removed.
Symptoms that may occur are
- Intermenstrual bleeding that is either permanent or irregular
- Discharge (light to dark brown)
- Foreign body sensation.
Occasionally, labor-like abdominal or abdominal pain also occurs, which can become worse, especially during sexual intercourse. Especially with large polyps, it can happen that they grow out of the cervical canal and thus become visible from the outside.
Bleeding
With polyps in the uterus, the bleeding in some women can be increased enormously, so that the woman's period is not only uncomfortable but also painful. However, this bleeding in itself is not a bad thing and does not have to mean that the polyps in the uterus are malignant. However, bleeding usually only occurs when the polyps in the uterus have already reached a certain size or when there are several polyps. In this case, the patient should think about having the polyps removed, otherwise the bleeding will recur and can be triggered without mechanical irritation. In addition, the cycle may shift and periods may or may not occur more frequently. However, it can also be that there is no bleeding but reddish-brownish discharge. Excessive bleeding from the polyps in the uterus can lead to anemia (anemia) or an iron deficiency.
However, it is important to know that bleeding can return for a short time even after an operation on the uterus. This in no way means that the operation was unsuccessful, but rather a reaction of the injured mucous membrane, similar to having a small wound on the skin that bleeds briefly and then closes again.
If you suffer from bleeding after your menopause, find out more about the causes and therapy in our article: Bleeding after menopause
Pain

Uterine polyps or endometrial polyps cause different symptoms. In addition to infertility and irregular or heavy bleeding, other unpleasant symptoms can occur. Most polyps, however, remain undetected for a very long time, on the one hand because they cause hardly any or no symptoms and on the other hand because many patients from a certain age visit the gynecologist less often.
However, it can be due to the polyps in the uterus (uterus) experience labor-like pain. This pain is caused by the fact that the uterus recognizes the polyps as foreign and tries to push them away with the help of "contractions". These pains caused by polyps in the uterus are extremely rare, but do occur and are definitely a reason to visit the gynecologist at the latest, otherwise the pain will keep recurring.
Some women also complain of feeling pain after or during intercourse due to irritation of the mucous membrane and polyps. This is also a reason for a gynecological evaluation.
However, it is important to know that most polyps do not cause any pain, but that the other symptoms mentioned above should be looked out for, as these are much more common and are more specific for the polyps.
Read more on the topic: Pain in the uterus
Can polyps cause back pain?
Back pain is not one of the typical symptoms that uterine polyps can cause. They are also not in close proximity to the spine or important nerves that could cause back pain. Uterine polyps are only a few millimeters in size, so that they could not lead to such painful complaints due to their growth in size.
diagnosis
Polyps are often discovered by chance during a pelvic exam. If they grow out of the cervix, the doctor may occasionally see them when examining the vagina. A closer look is made possible by the colposcopy, in which the polyps can practically be viewed with a "magnifying glass". Other polyps are usually found during a palpation examination.
If these methods do not detect anything, but uterine polyps are still suspected, an ultrasound (Sonography) carried out. If no abnormalities are discovered here either, because the polyps are very high on the body of the uterus, for example, a reflection of the uterus (Hysteroscopy) respectively.
This method has the advantage that the polyps can be viewed very precisely and it is possible to distinguish them from similar changes, for example the fibroids.
Nevertheless, a cell smear and tissue samples should be taken to confirm the diagnosis and to identify the rare but possible malignant degeneration early on and treat it appropriately.
Recognize polyps on the uterus
Polyps in the uterus do not always cause symptoms and are therefore not always recognizable to the layperson. Unfortunately, older women in particular go to the gynecologist less and less (Gynecologist), which is why they do not recognize the polyps in the uterus for a long time. Only with specific symptoms such as frequent intermenstrual bleeding, excessive menstrual bleeding or irregular menstrual bleeding does the patient notice that something is wrong. Other symptoms such as pain and bleeding during sexual intercourse can also be a warning signal, which then leads to the symptoms going to the gynecologist, who then recognizes the polyps in the uterus.
It is important to know that the polyps in the uterus cannot be recognized from the outside because they emerge from the mucous membrane (Endometrium) in the womb (uterus) and are therefore only recognized by the gynecologist with specific devices. As an affected patient, polyps in the uterus can only be recognized by the symptoms. However, since the polyps only cause symptoms if they are a certain size or a certain number, it is possible that many patients who do not regularly go to the gynecologist for checkups may not recognize the polyps in the uterus at all. This usually has no effect as the polyps rarely develop into uterine cancer. However, at a young age, infertility can occur in rare cases. This is why it is very important at any age and regardless of whether you have a partner or not to go to the gynecologist and have yourself checked, as only he can clearly identify the polyps in the uterus.
Polyps and the desire to have children - what are the risks?
Uterine polyps may make having children more difficult for couples who want to have children. Depending on the location and size of the polyp, there may be difficulties with fertilization and implantation. Similar to a copper coil, the polyp can prevent the fertilized egg cell from implanting. Polyps can not only prevent implantation, but also block the cervix. So the sperm cannot even enter.They can also block the passage from the fallopian tube into the uterine cavity, preventing pregnancy.
Women with symptomatic polyps in particular should remove them before a planned pregnancy. By doing this, they increase the chances of getting pregnant. In sterile women who do not have typical symptoms of polyps, it is advisable to seek clarification for asymptomatic polyps. About 3-5% of women who do not become pregnant and have no symptoms of a polyp will find an asymptomatic polyp after searching.
How do polyps behave during pregnancy?
Polyps that are already known before a planned pregnancy are usually removed beforehand to avoid complications during pregnancy. Even if the polyp is benign as such, it can lead to bleeding during pregnancy, pain or even an obstacle to childbirth. Implantation during pregnancy can also be difficult. In the worst case, the risk of a miscarriage can be increased. However, this does not always have to be the case and is very much dependent on the location of the polyp and its size. If a polyp only develops during pregnancy, it must be considered individually how best to proceed. In some cases, the polyp can be removed during pregnancy. However, if it is deep in the uterus or on the sensitive cervix, removal is not possible. The polyp is then often observed and, if necessary, it is recommended that the pregnant woman take physical rest. Mechanical stress, such as sexual intercourse, can then be more difficult or should be avoided during the pregnancy. The procedure, however, depends heavily on the individual pregnancy and the type of polyp.