Staphylococcus aureus
introduction
The term Staphylococcus aureus refers to a gram-positive bacterium that lives in facultative anaerobic conditions (meaning that it can survive in the presence of or without oxygen). As the name suggests, it has the round shape of cocci, which are usually found in clusters. It is differentiated from other staphylococci using the coagulase test. This is positive in Staphylococcus aureus. The bacterium is facultatively pathogenic. This means that under the right conditions, such as a weakened immune system of the infected person, it can cause various diseases. It is not a spore-forming agent and is not mobile. In hospitals, Staphylococcus aureus usually occurs as the hospital germ MRSA, which is resistant to various antibiotics.
Learn more about the Staph infection
You can find out more about the other bacteria belonging to the staphylococcal group on our website Staphylococci

I recognize an infection by these symptoms
The bacterium Staphylococcus aureus can cause a variety of diseases, which is why there are few symptoms that clearly indicate an infection with a Staphylococcus aureus. Typical symptoms are the classic signs of inflammation
- Redness,
- Swelling,
- Pain,
- Overheating and
- Function restriction.
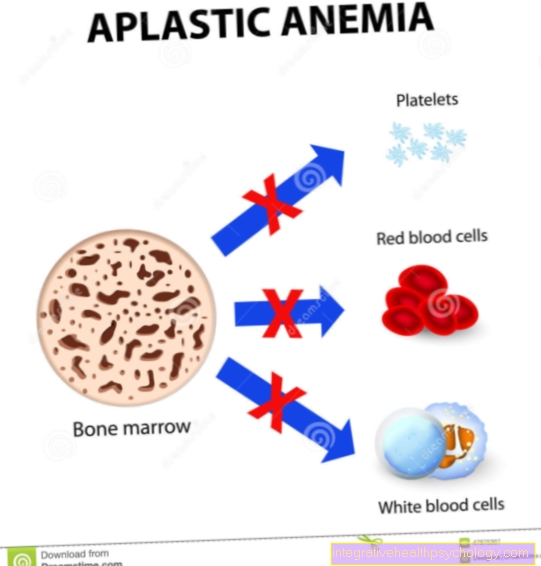
These symptoms occur, for example, with a wound infection, with a stye or an inflammation of the eye sac. Since the bacterium can cause pus to form due to various factors, the presence of pus is often a sign of infection. This pus can appear as part of an inflammation in one or more hair follicles. In addition, an abscess in general or, more specifically, a brain abscess and osteomyelitis, an inflammation of the bone marrow, can be caused by the bacterium.
Typical of an infection with Staphylococcus aureus is also the development of sepsis (blood poisoning) and endocarditis. Both of these disorders go with the symptoms
- Fever,
- Chills and
- Racing heart
hand in hand.
Sepsis can also lead to impaired consciousness, vomiting, chills and decreased blood pressure.
The following article may also be helpful to you: These are the symptoms of blood poisoning.
Endocarditis continues to show night sweats, weight loss, decreased performance and decreased appetite.
Further information on this topic can be found at: Correctly interpreting symptoms of endocarditis.
As part of a pneumonia, pneumonia, you may experience difficulty breathing and fever.
As part of the “Staphylococcal Scalded Skin Syndrome‘ ‘(SSSS), a fever, a rash, an otitis media and later blisters develop, all of which burst after a certain time.
That's how you get infected
The bacterium Staphylococcus aureus is largely transmitted through smear infections. For this it is necessary that infected persons or objects come into direct contact with another person. It can happen, for example, that a populated doorknob serves as a carrier for infection.
Staphylococci can also cause other infections through the air, but this is rare. For example, sick people can release the bacteria into the air by coughing and infect other people. Transmission is relatively common, especially when there is close contact with an infected person. However, if precautionary measures, such as maintaining a certain safety distance or wearing protective clothing, are taken, further infections are very rare.
Nevertheless, infection with staphylococci is fundamentally a danger, as these bacteria can develop resistances that make them very difficult to kill.
therapy
An infection with Staphylococcus aureus is not necessarily treated if it is detected on the skin. The reason for this is that some people have the bacterium as part of the natural bacterial skin flora. The bacterium cannot develop its pathogenic properties, which means that the person concerned does not experience any corresponding symptoms.
However, if it is detected in the context of a blood culture or if symptoms are found that are compatible with an infection by staphylococci, antibiotic therapy is used. Different active ingredients are used for this, depending on the species and the resistance of the bacteria to some antibiotics.
The following antibiotics are used
Due to the nature of their cell wall, staphylococci, like all other gram-positive bacteria, are initially sensitive to beta-lactam antibiotics. These antibiotics include, among others
- Methicillin,
- Penicillins,
- Carbapenems and
- Cephalosporins how Cefuroxime.
However, the majority of the staphylococcus strains now show one or more resistances to these antibiotics. For this reason, beta-lactam antibiotics are often given in combination with another active ingredient. This active ingredient is supposed to prevent the breakdown of the antibiotic in the bacterium. These include, for example
- Clavulanic acid,
- Tazobactam and
- Sulbactam.
In addition to the beta-lactam antibiotics, other active ingredients can also be used that have different mechanisms of action. These antibiotics include
- Clindamycin,
- Rifampicin,
- Clarithromycin,
- Azithromycin,
- Erythromycin or
- Gentamycin.
If there is an infection with MRSA, it is usually a special one Reserve antibiotics resorted to as normal antibiotics are usually ineffective. This often takes place
- Vancomycin,
- Linezolid,
- Teicoplanin or
- Doxycycline
Use.
What is MRSA?
MRSA originally stands for Methicillin-resistant Staphylococcus aureus and means bacteria of the species Staphylococcus aureus, which have developed a variety of resistances to methicillin and later other antibiotics. In the meantime, the term MRSA is commonly used as a Multi-resistant Staphylococcus aureus translates what is not entirely correct. The term is used, however, because these bacterial strains have a large number of resistances to antibiotics.
MRSA is a typical multi-resistant hospital germ. The bacterium is very common here and is responsible for a large number of hospital infections, including fatal ones.
On the one hand, the germ occurs on many surfaces that are not properly cleaned, on the other hand, the germ also colonizes many patients and hospital employees, who can also be a source of infection.
Infections with MRSA pose a high health risk, which is why people belonging to a risk group are screened before they are admitted to hospital. Infected patients are isolated in the hospital.
When rehabilitating MRSA carriers who are not sick, full-body disinfecting baths are recommended.
Also read our article: The transmission of MRSA.
Sepsis due to Staphylococcus aureus
Staphylococcal sepsis occurs when there is a massive increase in the number of bacteria in the blood, which causes a strong immune response. However, this reaction and the bacteria also harbor the risk of fatal multiple organ failure.
The entry portal of the bacterium can have different locations. After the formation of an abscess and subsequent infiltration of the surrounding, intact tissue, Staphylococcus aureus can attack the supplying blood vessels. In addition, the bacterium can settle relatively well on superficial skin wounds and subsequently also infiltrate the vessels. Indwelling venous cannulas and central venous catheters (CVC) also pose a particular risk for the development of staphylococcal sepsis, as this also allows bacteria to reach the blood vessels.
Staphylococcus aureus can be a special feature Superantigen, a product of the bacteria, which causes a massive reaction of the immune system. This usually results in the typical symptoms of sepsis
- Fever,
- Palpitations,
- Shock,
- decreased blood pressure,
- Impaired consciousness,
- Vomiting and
- increased breathing.
This usually leads to multiple organ failure with potentially fatal consequences. The diagnosis is made on the basis of the clinical symptoms and the detection of bacteria in the blood through a blood culture.
Staphylococcal sepsis occurs more frequently in women who use tampons during menstruation, as these create good conditions for the bacteria to multiply. From here, it is not the bacterium but the superantigen that enters the bloodstream and unfolds its effect. This so-called toxic shock syndrome is nevertheless very rare overall - only about a third of all women even carry the responsible bacterium in extremely small quantities in their vaginal flora, and the development of the syndrome can be counteracted by changing the tampon frequently and using tampons with low absorbency .
Infection after surgery
After an operation, various factors can trigger an infection with Staphylococcus aureus. On the one hand, the immune system is particularly weakened after surgery, which promotes infection. On the other hand, hospital germs such as MRSA occur more frequently in hospitals and can infect the patient. Infection through the surgical wound is also promoted, which offers the bacterium good conditions for colonization. More older patients are operated on than young patients. These people generally have a weaker immune system than younger people.
All of these factors lead to more frequent infections with Staphylococcus aureus postoperatively. As a result, the typical diseases that are triggered by Staphylococcus aureus can occur.However, sepsis, endocarditis or wound infection are particularly common. It is imperative to treat these diseases with antibiotics, otherwise they can be fatal.
Occurrence
Here Staphylococcus aureus also occurs naturally in the body:
skin
Staphylococcus aureus occurs permanently on the skin of up to 20% of the population. Staphylococcus aureus is temporarily detectable in up to 80% of the population. Hospital employees or people who are often hospitalized patients have a higher percentage. The bacterium does not develop any pathogenic properties, but forms part of the normal skin flora. However, these people can also act as vectors and infect other people with Staphylococcus aureus. This is particularly problematic with MRSA.
nose
In addition to the skin, Staphylococcus aureus can also be found in the mucous membranes. The mucous membrane of the nose, sinuses and throat is particularly affected. This is a higher percentage for hospital employees or people who are often patients in hospitals than for the general population. The bacteria in the mucous membranes can also be a cause of infection in other people.
ear
Staphylococcus aureus can also cause an infection of the middle ear with a subsequent otitis media. The bacterium gets there via the ear trumpet, which also Tuba auditiva or Eustachian tube is called. This represents a connection between the middle ear and the nose or throat. Typically, only one middle ear is infected.
The following occurrences of Staphylococcus aureus are pathological:
blood
The detection of Staphylococcus aureus in the blood always has disease value. The bacterium can multiply well in the blood and cause endocarditis as well as sepsis. The bacterium's access routes to the blood can be varied. After the formation of an abscess, Staphylococcus aureus can subsequently infiltrate the surrounding, intact tissue and attack the blood vessels supplying it. Furthermore, the bacterium can settle relatively well on superficial skin wounds and also infiltrate the vessels over time. Indwelling venous cannulas and central venous catheters (CVC) also pose a particular risk for the development of staphylococcal sepsis, as this allows the bacteria to also reach the blood vessels by migrating down the plastic structures.
abscess
Staphylococcus aureus can infiltrate and destroy healthy human tissue due to the various enzymes it releases. This can lead to the development of an abscess. The formation of an abscess always poses a risk for the infiltration of surrounding blood vessels, which can lead to sepsis. The bacterium can sometimes be detected within this abscess by microbiological cultivation.
Pimples
A pimple is caused by the clogging of a pore in the skin. As a rule, there are no complications when a pimple appears. Constipation can be caused by various substances. Among other things, sweat or sebum can cause a blockage. This creates good conditions for colonization by pathogenic bacteria such as Staphylococcus aureus. Here the bacterium can multiply and trigger further symptoms. In extreme cases, the pimple can spread to a boil, carbuncle, or abscess. There is a risk of developing sepsis.






-braun.jpg)