Trachoma
Synonyms
Greek: trachôma, trachus - "rough", English: trachoma
Trachomatous conjunctivitis, trachomatous inclusion conjunctivitis, Egyptian ocular inflammation, conjunctival granular disease
Definition of trachoma
Trachoma is a chronic conjunctivitis caused by the bacterium Chlamydia trachomatis (Conjunctivitis), which often leads to blindness.

How common is trachoma?
Trachoma is very rare in Europe and has to be reported here. In India, Africa and the developing countries of the southern Mediterranean, however, it is still one of the most common causes of blindness, affecting around 4% of the population there, and the most common infectious cause of blindness worldwide. In Egypt, China and India alone there are around 500 million sufferers.
What are the symptoms of trachoma?
After the initial infection with C. trachomatis, which particularly affects small children in endemic areas, an unspecific weeping (serousConjunctivitis with a foreign body sensation. Soon after, on the conjunctiva (Conjunctiva) of the upper eyelid large granular accumulations of inflammatory cells (follicle), which look gelatinous, enlarge massively and finally burst open. This will drain the infectious fluid trapped in the follicles (secretion) outward. After the follicles burst, scars appear, which leads to a shrinkage of the conjunctiva of the upper eyelid, which pulls the upper row of eyelashes inwards (Entropion). Because of these follicles, the surface of the conjunctiva of the upper eyelid appears rough, which is where the name trachoma comes from.
The inflammation affects the eyelid conjunctiva and the transitional fold, but not the conjunctiva over the eyeball. The knot-shaped elevation (Caruncle) and the conjunctival fold in the nasal corner of the eye are often clearly swollen. From the upper edge of the cornea, a gelatinous, follicular opacity grows over the cornea. This cloudiness is called "pannus from above" or pannus on the eye.
The entropion causes the eyelashes to rub the cornea and create a corneal ulcer (Corneal ulcer).
The end stage of a severe trachoma is a porcelain-like corneal scar, which consists of degenerate conjunctival and corneal cells with few blood vessels. It is caused by drying out of the surface of the eyeball and recurring erosions. The advanced and final stages of the disease develop over the course of several years.
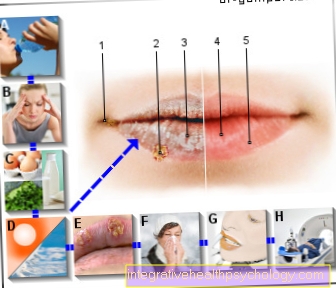
The World Health Organization (WHO) suggests dividing the trachoma into 5 clinical stages based on the severity of the symptoms:
- follicular trachomatous inflammation in 5 or more follicles of the conjunctiva of the upper eyelid,
- severe trachomatous inflammation with pronounced inflammatory thickening of the conjunctiva of the upper eyelid,
- trachomatous, conjunctival scarring with visible scars of the conjunctiva of the upper eyelid,
- trachomatous trichiasis when rubbing at least one eyelash on the eyeball,
- corneal opacity
In addition, it can always lead to a superinfection by bacteria such as Haemophilus, Moraxella, Pneumococci and Streptococci come, which can aggravate the clinical picture at any time in trachoma, both primary and in the chronic stage.
How is trachoma diagnosed?
The diagnosis of trachoma is based on the symptoms, i.e. the clinical picture.
In addition, microbiological diagnostics can be carried out: Direct microscopic detection is possible using immunofluorescence. The chlamydia are stained with fluorescence-marked antibodies and thus made visible. DNA detection by means of DNA replication using the polymerase chain reaction is more complex and expensive, but more reliable (PCR). The test material consists of conjunctival cells, the extraction of which is very painful for the patient.
Stages of a trachoma
According to McCallen, trachoma is divided into four different stages. In the first stage there is irritation of the conjunctiva, but this is still relatively unspecific. However, it occurs on both sides and there is often a secretion of pus or fluid. In the second stage, yellowish-white lymph follicles appear on the lateral conjunctiva of the upper eyelid. Stage three these follicles burst and fluid drains. The fourth stage is described by scarring and ulcerations on the cornea. The final stage is defined by the loss of opportunity to close the eyelid.
Causes of trachoma
The causative agent of the trachoma is the gram-negative bacterium Chlamydia trachomatis, which belongs to the chlamydia family. It comes in two different forms:
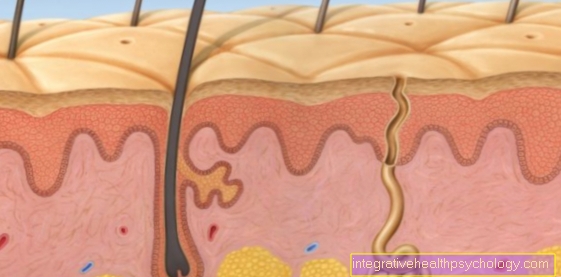
Outside a host cell it exists as a very resistant elementary body (EK) with a diameter of 0.25-0.3 µm. In this form, the bacterium infects the host cell. When taken up by the cell, the elementary bodies are enclosed in vacuoles, which protect them from the cell's own degradation. In these inclusions the elementary bodies change into reticular bodies (RK) that have their own metabolism and begin to multiply through division.After 2-3 days the host cell perishes, the chlamydia, which have meanwhile matured again into elementary bodies, are released and can then again attack other cells.
Chlamydia trachomatis is mainly transmitted through smear infection, a direct transmission of pathogens through contact, within close communities, for example when towels are used together. They can also be transmitted by flies and insects that settle in the inner corner of the eyelid and cause inflammation in malnourished, weakened children and adults. Poor hygiene plays a crucial role. Trachoma practically no longer occurs in the population groups of tropical countries who live under good hygienic conditions thanks to an adequate water supply. At the scarring stage, the disease is hardly contagious. There is no permanent immunity.
Chlamydia trachomatis (trachoma) causes two forms of conjunctivitis:
In countries with good hygienic conditions, e.g. Central Europe, serotypes D – K cause chlamydial conjunctivitis in adults ("inclusion body conjunctivitis"), in countries with poor hygienic conditions, serotypes A – C cause trachoma, which often begins in childhood.
Chlamydia pathogen
The causative agent of the trachoma is Chlamydia trachomatis. There are different groups of these bacteria. More precisely, the trachoma is caused by Chlamdia trachomatis Serovar A-C. It is transmitted directly from person to person via flies. Chlamydia are gram-negative bacteria that only live intracellularly. Chlamydia cause a variety of diseases. Other groups, for example, are the cause of urogenital infections and lung diseases.
Also read: Chlamydial infection and Chlamydial infection of the lungs
How is trachoma treated?
Systemic or local, intracellularly effective antibiotics are used to treat trachoma. The WHO recommends local therapy with tetracyclines. Therapy with azithromycin is also possible, but it is more expensive.
At the scar stage, surgery should be done to remove entropion and trichiasis. Surgical restoration of the cornea (keratoplasty) has little chance of success in the final stage of a severe trachoma.
In most cases, however, the treatment options for trachoma are very limited in the affected countries due to the socio-economic standards.
How can you prevent trachoma?
The transmission by smear infection can through appropriate hygiene measures, eg. B. hygienic hand disinfection with 70% alcohol are largely prevented. Contact lens wearers must be aware of the potential dangers of contact lenses (Corneal injuries with superinfection) and instructed in proper cleaning and storage.
A lack of hygiene options in underdeveloped countries favor the occurrence of trachoma. Only by improving the infrastructure, an adequate water supply and improved hygienic conditions (e.g. washing your face once a day) can the incidence of trachoma be reduced.
How contagious is that?
A trachoma, like many bacterial infections, is highly contagious. It has not yet been clarified whether patients are already infectious during the incubation period of 5-10 days or only when the first symptoms appear. However, it is transmitted from person to person via flies that carry the bacteria or via smear infection. For example, poor hygiene or sharing a towel can be a transmission route.
What is the prognosis with a trachoma?
The prognosis of trachoma depends on the stage of the disease. The prognosis is good if treatment is started at an early stage. Blindness only occurs if the disease has not been treated for years and re-infection occurs frequently.
What is the history of trachoma?
The term chlamydia is derived from chlamys (gr. the coat) from.
A description of a trachoma-like disease of the human eye can already be found in ancient traditions. In 1907, the first description of Chlamydia trachomatis was made by Ludwig Halberstadter (* 1876 in Beuthen, Upper Silesia, † 1949 in New York City) and Stanislaus von Prowazek (* 1875 Czech Republic, † 1915 in Cottbus). They were able to show that the clinical picture of trachoma can be experimentally transferred from humans to great apes: Using a specific staining technique, Giemsa staining, they identified cells from swabs of the conjunctiva (Conjunctiva) Vacuoles, which they interpreted as the cause of the trachoma. In the years that followed, similar inclusion bodies were found in conjunctival smears from newborns with conjunctivitis, in cervical swabs from their mothers, and in urethral swabs from men. Due to their inability to cultivate on artificial culture media, their small size and their purely intracellular reproduction, the pathogens were wrongly classified as viruses at the time. Thanks to cell culture techniques and electromicroscopy, it became clear in the mid-1960s that chlamydia is not a virus, but a bacteria. So they were recognized in 1966 as a separate order Chlamydiales of bacteria.




















.jpg)

.jpg)


