Lower leg
introduction
The lower leg is part of the leg and lies between the foot and the thigh. These parts are connected to one another via corresponding joints.
The lower leg itself is made up of
- two bony structures, as well
- numerous muscles,
- Nerves and
- Vessels, which are shown below.
It is primarily used for locomotion and statics, so that people can stand and walk safely. In addition, the muscles of the lower leg are largely responsible for the movement of the feet and toes, which ensures safe walking.

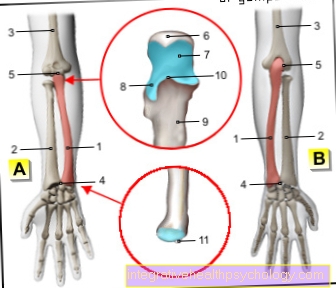
bone
Of the Lower leg consists of two bony parts, the
- Fibula (Fibula) and the
- Shin (Tibia).
Either Seemed- as well as Fibula are long Long boneswhose shaft the Diaphysis represents. The head of both bones is that Epiphysis. In articulated connection with the Thigh however, only the shin stands. This is clear stronger and functional more important than the fibula. The shin carries that static Weight and represents the articulated connection to the adjacent structures.
The body-hugging (proximal) End of Shin is widened and, like the thigh, has a
- lateral (lateral) and one
- middle (medial) Joint knorren (Condyle).
In between there is one cartilage-free Surface (Eminentia intercondylaris). At the front of the shin lies a bony protrusion, the Tibial tuberosity. This is where it starts Kneecap ligament (Ligamentum patellae) on. In addition, the lateral condyle has an oval joint surface with which the fibula articulates. The shaft of the tibia is elongated and is called the Corpus tibiae designated.
Remote from the body the shin forms a thickening again, the Inner ankle (Medial malleolus). This forms with the Outer ankle of the fibula the Malleole forkwhich is part of the Ankle is.
The Fibula (Fibula) lies to the side of the shin. It mainly serves as the starting point and source of various muscles, as well as for training the malleolar fork. The Fibula head (Head fibulae) is in contact with the shin through an articulated connection. To that Thigh bone the fibula has no direct contact.
Also the main part of the fibula is called Corpus fibulae and is mainly used as a Origin- and Starting point of the individual muscles. At the distant (distal) At the end of the fibula, this also goes into an ankle, the Outer ankle (Lateral malleolus), over. Since the outer ankle is much more delicate than the inner ankle, fractures occur more often here
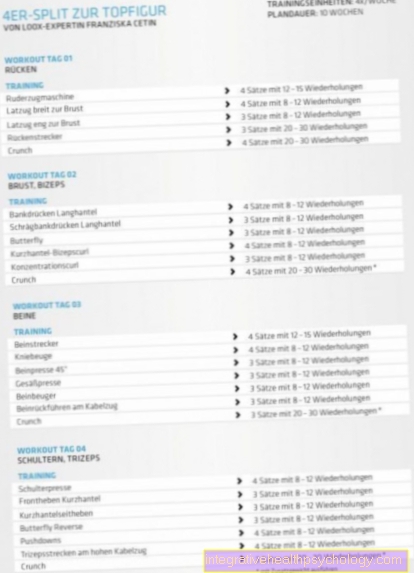
Musculature
Three muscle groups can be distinguished on the lower leg, each of which is located in its own muscle box and can therefore be easily separated from one another.
One distinguishes the
- anterior extensor muscles (Extensors), the
- posterior flexor muscles (Flexors) and the
- Laterally lying peroneal group.
All extensor muscles of the lower leg are innervated by the fibular nerve (= peroneus) profundus.
Extensor muscles include the
- Tibialis anterior muscle,
- Extensor hallucis longus muscle and the
- Extensor digitorum longus muscle.
The tibialis anterior muscle originates from the lateral condyle of the tibia and attaches to the first tarsal bone. As a rule, this muscle is relatively strong.
It causes the foot to lift in the ankle joint (Dorsiflexion).
The extensor hallucis longus muscle arises on the lateral edge of the fibula and attaches to the bony terminal of the big toe. As a result, he stretches the big toe in the base and end joints. It also lifts the foot (Dorsiflexion) in the upper ankle.
The extensor digitorum longus muscle has its origin at the front edge of the fibula and attaches to the aponeurosis of the back of the foot of toes 2 to 5. This also lifts the foot in the upper ankle and extends toes 2 to 5.
The peroneal group is made up of the peroneaus longus and brevis muscles. Both muscles are innervated by the superficial superficial fibular nerve. The long peroneal muscle has its origin on the lateral front surface of the fibula and on the head of the fibula. Its tendon has a very long course and ultimately reaches the side of the sole of the foot. From there it runs transversely under the foot and is therefore responsible for tensioning the transverse arch of the foot. He also lowers his foot (Plantar flexion) and lifts the foot outwards (Pronation).
The peroneus brevis muscle arises somewhat lower than the long part on the front of the fibula. The further course and the function correspond to that of the long part.
The flexor muscles of the lower leg are again divided into two groups. The superficial flexors are the
- Triceps surae muscle and the
- Plantaris muscle.
The deep flexor muscles include the
- Flexor digitorum longus muscle, the
- Flexor hallucis longus muscle, the
- Tibialis posterior muscle and the
- Popliteus muscle.
All flexor muscles are innervated by the tibial nerve.
The triceps surae muscle is composed of three heads.
- The two-headed gastrocnemius muscle and the
- Soleus muscle.
These three heads are popularly known as "calves" because they are responsible for the silhouette of the rear lower leg.
The gastrocnemius muscle finds its origin on the lateral (lateral) and middle (medial) Condyle of the femur. These two muscle parts unite in the course and put on the "heel" (Calcaneal tuberosity) on.
In the knee joint this muscle flexes, in the upper ankle joint it leads to the lowering of the foot (Plantar flexion) and in the lower ankle he lifts the foot inwards (Supination).
The soleus muscle is largely covered by the gastrocnemius muscle. It arises on the back of the tibia and on the head of the fibula and also attaches to the calcaneal tuberosity. This also leads to plantar flexion in the upper and supination in the lower ankle.
The plantaris muscle is a relatively small muscle whose function is largely negligible. It has its origin in the lateral condyle of the thigh, its insertion is the calcaneal tuberosity. It thus has the same function as the aforementioned triceps surae muscle.
The flexor digitorum longus muscle has its origin on the posterior surface of the tibia. It attaches to the end links of the 2nd to 5th toes and bends them.
The tibialis posterior muscle arises on the membrane between the fibula and shin bone (Membrana interossea). It attaches to different tarsal bones and leads to the lifting of the inner edge of the foot upwards (Supination). It is also part of the longitudinal arch of the foot.
The flexor hallucis longus muscle arises from the fibula and attaches to the distal phalanx of the big toe. As a result, he bends his big toe.
The popliteus muscle is the only muscle in the flexor group that does not pull over one of the ankle joints. Its origin is the lateral condyle of the thigh, its insertion the back surface of the fibula. As a result, it only exercises its function on the knee joint and bends it. He also tensions the joint capsule of the knee joint.
Figure lower leg muscles

Lower leg muscles
- Iliac-tibial tendon -
Iliotibial band - Kneecap - patella
- Tibia anterior muscle -
Tibialis anterior muscle - Internal calf muscle -
Gastrocnemius muscle,
Caput mediale - Long fibula muscle -
Musculus fibularis longus - Clod muscle -
Soleus muscle - Long toe extender -
M. extensor digitorum longus - Long big toe extender -
M. extensor hallucis longus - Lower strap of the
Extensor tendons -
Retinaculum musculorum
extensorum inferius - Short big toe extensor -
Extensor hallucis brevis muscle - Short toe extender -
Extensor digitorum brevis muscle - Fibula head -
Head fibulae - External calf muscle -
Gastrocnemius muscle,
Caput laterale - Achilles tendon -
Tendo calcaneus - Long big toe flexor -
Flexor hallucis longus muscle - Sole muscle -
Plantaris muscle
You can find an overview of all Dr-Gumpert images at: medical illustrations
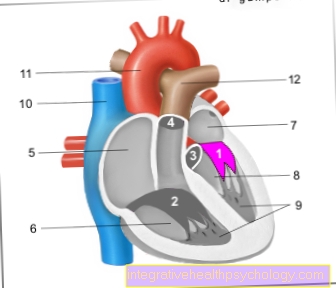
Joints
The Knee joint as a connection between Upper- and Lower leg is a Hinge joint.
In this are
- diffraction (Flexion) and
- Elongation (Extension), such as
- Turning movements possible inside and outside.
The Knee joint is passed through the two condyles of Thigh and Shin educated.
The fibula has no part in it Knee joint. Between the Lower leg and the foot is the upper one Ankle joint. This is supported by the Malleole fork between
- Seemed- and
- Fibula and the
- Ankle bone (Talus) educated.
In this are the movements of the Foot downward (Plantar flexion), up (Dorsiflexion), as well as the lifting of the inner edge of the foot inwards (Supination) and the Elevation the outer edge of the foot outwards (Pronation) possible.
Appointment with ?

I would be happy to advise you!
Who am I?
My name is I am a specialist in orthopedics and the founder of .
Various television programs and print media report regularly about my work. On HR television you can see me every 6 weeks live on "Hallo Hessen".
But now enough is indicated ;-)
In order to be able to treat successfully in orthopedics, a thorough examination, diagnosis and a medical history are required.
In our very economic world in particular, there is too little time to thoroughly grasp the complex diseases of orthopedics and thus initiate targeted treatment.
I don't want to join the ranks of "quick knife pullers".
The aim of any treatment is treatment without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You will find me:
- - orthopedic surgeons
14
You can make an appointment here.
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
For more information about myself, see - Orthopedists.
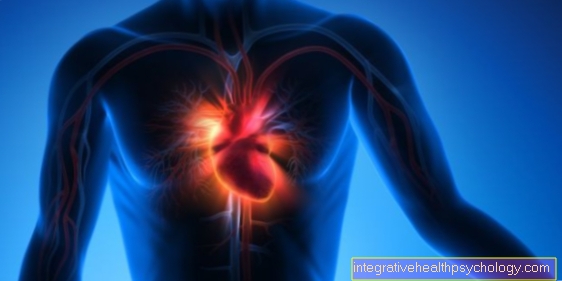
Vessels
In the squat it splits Tibial artery in its two main branches,
- the Anterior tibial artery (anterior tibial artery) and
- posterior (posterior tibial artery).
From the front Tibial artery numerous branches emerge, which the knee, the front of the Lower leg to supply blood to the back of the foot. The fibrous artery arises from the posterior tibial artery (Fibular artery). From this branches branch off again, which supply the inner and outer soles of the feet with blood.
The Veins are divided into the deep and superficial veins. The largest superficial vein is the Great saphenous vein, which is relatively centered on Lower leg up to the hip runs and there in the great depth Femoral vein flows out.
The smaller one hidden Vena saphena parva also runs in the middle of the calf in the subcutaneous fatty tissue and finally flows into the hollow of the knee Popliteal vein.
The deeps Veins usually run with the arteries and are much more important than the superficial veins.
They are divided into three groups:
- The tibialis anterior- Group,
- tibialis-posterior- group and the
- fibularis- Group.
These vessels take the blood accordingly superficial veins over Bridging veins on and transport this direction heart.
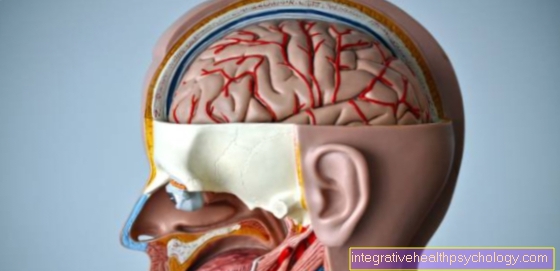
annoy
Femoral nerve from the lumbar Nerve plexus (Lumbar plexus) sensitively innervates the medial side of the Knee joint and the medial side of the lower leg to the Ankle.
Of the Sciatic nerveicus from the sacral plexus divides into its two main branches at the level of the hollow of the knee:
- Common fibular nerve and
- Tibial nerve.
Of the Common fibular nerve sensitively innervates the lateral skin of the lower leg, which divides again into two branches.
Of the Superficial fibular nerve innervates the motor Peroneus longus muscle and brevis. In addition, it sensitively cares for the skin of the whole Back of the foot. Of the Deep fibular nerve motorized everyone Extensor muscles of the lower leg. It also sensitively innervates a small area of skin between the first and second toe.
Of the Tibial nerve supplies the motor Gastrocnemius muscle. In its course, the tibial nerve gives off a few small branches that form numerous muscles of the Lower leg innervate. In addition, some branches sensitively supply the area of the heel. Another branch supplies the
- Abductor hallucis muscle, the
- Flexor digitorum brevis muscle and the
- Flexor hallucis longus muscle.
In addition, this branch sensitively supplies the Spaces between the toes.
Diseases of the lower leg
Lower leg thrombosis
Lower leg thromboses are caused by a blood clot in the arteries or veins that severely restrict blood flow. The following symptoms are:
- pulling or pulsing pain
- severe swelling of the leg including the foot
- Feeling of heaviness and tension
- Redness
- excessive heating
- sometimes fever and a rapid pulse.
Often the superficial veins also protrude more and are now clearly visible. The symptoms mentioned are neither proof of a thrombosis, nor does the absence of a symptom rule out a thrombosis.
The danger of thrombosis in the lower leg is the blockage of a pulmonary artery (pulmonary embolism) if the thrombus loosens. This is potentially life threatening. In addition, the affected vessel and the surrounding tissue can be damaged.
An important immediate measure in acute treatment is elevating the affected leg and applying a compression bandage. This prevents further swelling and further backlogging of the blood.
In any case, a doctor should be consulted. Here you can get drugs to dissolve the thrombus, which are supplemented by anticoagulant drugs. The dosage of these drugs must be controlled frequently.
In severe thromboses and young patients, the blood clot is often removed by surgery.
Risk factors for a thrombosis are flow obstacles in the blood, a slow flow rate and an increased tendency to clot. This is often caused by frequent alcohol consumption, frequent smoking, sedentary lifestyle, obesity but also a lack of fluids.
You can find detailed information on this topic at: Thrombosis in the leg
Pain in the lower leg
Pain in the lower leg is a common complaint. The causes of this pain can be very diverse. Vascular or interstitial, bony, muscular or sinewy or even combined causes come into consideration, whereby the development can also be very different.
As in other parts of the body, different types of pain can be differentiated on the lower leg. A dull pulsation usually indicates a vascular cause (affects vessels), while a sharp pain usually causes muscular problems. Meanwhile, pain due to bone causes is mostly based on a fracture following trauma, whereby pain of a vascular nature can occur due to thrombosis.
The vessels are also the origin of edema, which causes problems in the lower leg in particular, as they can develop particularly high pressure here due to the rigid connective tissue muscle fascia. If left untreated, this usually leads to irreversible damage to the nerves and muscles.
Furthermore, less serious causes can already be the origin of pain. If you already strain your legs too much while exercising, some people will experience cramps immediately, others later, which are not dangerous but can be very painful.
You can read more detailed information on this topic here: Pain in the lower leg
Lower leg fracture
A lower leg fracture is the breakage of one or both bones in the lower leg. Since these bones are very solid, they only break after a massive force, such as a traffic accident, a fall from great heights or a skiing accident.
Signs of a fracture are severe pain and the affected person is unable to withstand stress. Immediate treatment measures include splinting, cooling and elevating the leg. Then you should definitely go to a hospital or a doctor.
The prognosis for complete healing of a lower leg fracture is relatively high. Should there be an open break, i.e. the bone is exposed to the air and must be operated on immediately. For closed fractures, the type of therapy can vary.
The bones can be stabilized with an intramedullary nail, plate and screw or an external fixator. After about 18 months, these objects are surgically removed. In some cases, however, it is sufficient to keep the leg still and let the bone heal on its own. For this purpose, a plaster of paris is applied for a few weeks.
As a rule, all lower leg fractures are resilient after twelve weeks at the latest. Complications that can occur after a fracture are thromboses, nerve and vascular damage and also wound healing disorders. The coordination of running is also usually limited, which is why walking training is advisable.
Are you interested in this topic? Read more about this under: Fracture of the lower leg
Lower leg edema
Lower leg edema is often perceived simply as fat legs. This leads to water retention in the tissue. They can be recognized by pressing a finger on the skin. If a dent remains after the end of the pressure, there is edema. As a rule, they start at the ankles and from there rise further and further towards the trunk of the body.
The causes of lower leg edema can be very diverse and range from heart failure and kidney failure to thrombosis and local inflammation. This is also the reason why the underlying diseases can often only be recognized and treated late.
With unilateral leg edema, there is usually a local outflow disorder. This is typically due to deep vein thrombosis, lymphedema, or edematous inflammation.
If both sides are affected to the same extent, it is usually an organ that is further away. The most common cause of this is heart failure. In addition, kidney failure can be the cause, as the amount of fluid in the body is too high.
Therapy is cause-related, i.e. the disease that is the cause of the edema is treated. This can vary greatly depending on the cause or organ and thus includes different chances of recovery.
Our next article could also be of interest to you: Edema in the leg
Lower leg ulcer
A lower leg ulcer is a common disease in diabetes mellitus, peripheral arterial occlusive disease (PAVK) and chronic venous insufficiency after thrombosis. Infections, superficial skin lesions and tumors can also be the cause.
An insufficient supply of oxygen leads to the skin dying off and defective, resulting in a deep, weeping wound. This can be accompanied by typical signs of inflammation such as redness, swelling or pain. The danger with such an ulcer is the colonization with bacteria.
All of this means that the healing process is slowed down and it can take several months for it to heal completely. In severe cases, the healing process can take years or the ulcer persists.
Treatment can be both surgical and conservative. Surgical measures aim to improve the underlying cause, i.e. The aim is to increase blood flow. Conservative measures may vary depending on the cause. However, they all include cleaning the wound, removing any deposits that have formed and preventing it from drying out.
In the case of arterial causes, an attempt is made to increase blood flow, while in the case of venous causes, an attempt is made to prevent blood congestion by compression.
Compartment syndrome on the lower leg
The muscles of the lower leg are divided into several so-called boxes by connective tissue. There are several muscles in each box. A high degree of rigidity is an important characteristic of the muscular membranes, as it is the cause of what is known as a compartment syndrome.
Compartment syndrome is characterized by severe pain, numbness in the lower leg and foot and a feeling of tension. In addition, mobility is greatly reduced and the pulse on the foot can no longer be felt.
The cause of this is a dream such as a blow to the muscle or a fracture of the bones, as a result of which there is a hemorrhage in one or more muscle boxes. This leads to an increase in pressure in the box, as a result of which blood flow is reduced, tissue dies and irreparable nerve damage occurs.
Compartment syndrome is initially treated with cooling and immobilization. The muscle skin should then be surgically split as soon as possible. This usually relieves the affected compartment. After a while, the seam can be closed.
You can read detailed information on this topic in the next article: Compartment syndrome on the lower leg
Therapy options on the lower leg
What is a lower leg orthosis?
A lower leg orthosis extends from the sole of the foot to the knee, with the knee joint being spared. This is made to measure and is used for aftercare of the affected region after an injury.
The lower leg orthosis takes over the functions of the leg, which can no longer be performed, and also fulfills a protective function, because gentle mobilization is particularly important for the symptom-free use of the leg afterwards. In addition, a certain restriction of movement should prevent further injuries to the possibly unstable leg.
The ankle of the orthosis usually has a supportive effect on lifting the foot, but can also have a massive influence on the extension. A lower leg orthosis is often used after sports injuries when ligaments in the ankle or within the lower leg are torn. Often this concerns football.
They are also often used in chronic, progressive diseases when they can prevent pain and rapid deterioration.
Are you interested in this topic? Read our next article below: Lower leg orthosis
What is a lower leg brace?
Lower leg bandages are often made of neoprene reinforced with nylon. These have a hose-like shape and are slipped over the foot like stockings and then worn around the lower leg muscles. Velcro fasteners often allow the size to be adjusted continuously, so that they can be worn over the entire length of the lower leg without any problems.
The principle of action of the bandages is based on compression of the muscles, which increases the natural effect of the muscles. Thus, the leg is stabilized by a bandage. In addition, existing pain can be reduced.
Another positive effect of the bandages is a higher blood flow and the resulting higher body temperature below the bandage, which reduces the susceptibility to injury and thus takes on a protective function.
Wearing a bandage is recommended if the leg muscles are stressed, cramps, small muscle fiber tears and strains, bruises and injuries to the shin.
Lower leg amputation
A lower leg amputation is the (surgical) removal of the lower leg. This involves removing the leg below the knee joint. This enables the joint to continue to function, medium-heavy activities still have to be carried out and walking longer distances and walking on uneven ground are still possible.
Nonetheless, this procedure represents a great challenge for the person concerned and the medical staff. It is absolutely essential that comprehensive physical and psychological follow-up care is offered afterwards. As soon as the lower leg has been amputated, this begins.
Follow-up care ranges from a stay in a rehabilitation clinic to medical care for the remaining leg stump to advice and familiarization with a prosthesis. Afterwards, physiotherapeutic follow-up treatment is also offered.
The leg stump is mechanically resilient after about four to six weeks.This is where walking training usually begins on a parallel bars or with the help of crutches. Local surgical corrections have to be carried out on the scar tissue in about a fifth of the amputations.
The reason for an amputation is usually arterial occlusive disease, but often rapidly progressing diseases such as gas fires can also be the cause. Risk factors that can lead to an amputation are severe diabetes mellitus, smoking and very high-fat food that is consumed over a long period of time.
Many causes of an amputation have in common that there is an insufficient supply of oxygen to the lower leg. This manifests itself in pain, dead tissue, and skin lesions.
Would you like to learn more about this topic? Read our next article below: Lower leg amputation
What is a lower leg prosthesis?
A lower leg prosthesis is a replacement of the lower leg that is located outside the body and is used after amputations to compensate for the loss of your own lower leg to some extent. It is fixed below the knee and enables the affected person to walk. Experienced people usually hardly notice a prosthesis in everyday life. Doing sports is also possible.
A prosthesis is fixed at relatively pressure-insensitive areas of the residual limb. This includes the remaining sections of the tibia, the ligament structure between the two bones of the tibia, the patellar tendon, and the rest of the calf muscles. This does not include the bone ends of the calf and shin bones.
These structures are more sensitive to pressure, which is why particularly severe pain can occur here and the skin can often have sore spots. In the first few months after an amputation, the pain in the lower leg stump is more severe, but it decreases with time. You also sweat more than usual.
This also gets better with increasing. Depending on your needs, you can choose between various types of prostheses. There are prostheses for everyday life, sports and other activities.
You can find detailed information on this topic at: Lower leg prosthesis
Summary
Of the Lower leg consists of two bony structures, the
Shin (Tibia) and the Fibula (Fibula).
These are about that Knee joint with the Thigh and about that upper ankle with the Ankle bone (Talus) connected.
The muscles of the lower leg are divided into three groups:
- the Flexor (Flexors),
- the Straightener (Extensors) and
- the Peroneus group.
Since these individual muscle groups are each in a Muscle box they are easy to separate from each other.
The arterial supply takes place mainly through the Popliteal arterywhich from the great Femoral artery of the thigh. It divides into its main branches in the hollow of the knee and thus supplies the Lower leg.
The Veins will be in a superficial and a depth Group divided which by small Bridging veins are connected and thereby transport the blood to the heart.
The neural innervation occurs mainly through branches of the Sciatic nerve, which also divides in the hollow of the knee and then innervates the muscles and the skin.