We had Corona - it was so dangerous!
interviewed two medical students from am today who fell ill with the corona infection COVID 19 in March 2020. The two are twin sisters and are studying medicine at the Goethe University in in their 10th semester.

: How did you get infected?
Joanna: You can never be absolutely sure where you got infected. However, since I followed the isolation recommendations very strictly at the time of my infection, I can fairly safely say that I got infected while working for a doctor in the health department, where I and my sister worked on a medical advice hotline for questions about the coronavirus to have. At the time, besides work, I hardly had any external contacts and didn't even go shopping.
Deborah: Yes, it looks very similar for me. Besides my boyfriend and at work, I had no contact with other people either. I also think that I got infected while working in the health department, of course I can't prove that. I always kept my distance when shopping, but you can't be sure about that.
: What were your first symptoms?
Joanna: My first symptoms were a headache. At the time, I assumed that it could be due to lack of sleep, as I was quite overtired. You could describe it like the headache that you have when you are very tired or when you have a hangover.
Deborah: I can't really tell if I had any symptoms at all. At least I didn't consciously notice any symptoms. In retrospect, I noticed that I was a little dizzy for one day and my circulation was somehow unstable. It was a very strange feeling that I can't describe well. But I don't know for sure whether that actually came from Sars-CoV2 (Corona virus). In addition, something burned in the oven one evening while we were cooking and I smelled it very late at the time. But since my nose is sometimes closed due to an allergy, I did not associate that with the corona virus.
: What did you do then?
Joanna: The process for us was a little different than for most patients. Through our work in the health department, we were in contact with at least one doctor and 9 employees every day. Since one of the doctors fell ill with COVID 19, all employees who were working shifts with her were given a prophylactic test. When we received this message, neither of us had any symptoms.
Deborah: The contact with the positive doctor was actually not a direct contact with a high risk of infection. We all wore surgical face mask and always kept our distance. According to RKI guidelines, we shouldn't have all been tested out of caution, that was just the goodwill of the health department for their employees. However, when we received the message that we were in contact with the positive person, we did not leave the house at all until the test result, purely out of caution. As I said, we had no symptoms at the time.
: How was the test for you?
Deborah: We already knew the procedure for a deep nasopharynx smear from the hospital. Sometimes I had to make such compromises with patients myself, I always felt sorry for that. Such a smear is not really bad, but it is a bit uncomfortable. For the test you need material from your nose and throat. That's why you go deep into one nostril with a kind of long swab and right behind into the throat. If the test is done correctly, the gag reflex must be triggered. During my first smear test, I accidentally hit the examiner's arm away as a reflex. In the end, a tear even ran down me.
Joanna: I've struggled with gagging after some dental treatments. Accordingly, I found the smears uncomfortable. After my first smear test, I had nasal pain for half a day. But there are worse things!
: How long did it take to get your test result?
Deborah: Our test was around 10 a.m. on a Friday morning. We got our result on Tuesday evening around 8 p.m. So it took a little over 4 days. The results were actually already available to the health department at the weekend, but were sent to the wrong address and therefore only accessed on Tuesday evening.
Joanna: However, our tests were also marked “urgent” as a health department employee. Otherwise the results would not have been there so quickly.
: Were you afraid of COVID?
Joanna: I wouldn't say real fear, but respect would. In itself, you can never be completely sure how the infection will work out in you. However, I do not belong to the risk group myself, so a severe course was extremely unlikely. When I went to bed on the evening of the test result, I still had thoughts like “What do I do if I get a bad course? I don't even have a living will. " But I quickly pushed such thoughts aside. I was just really glad that I hadn't visited my grandparents or my parents recently! I would have completely reproached myself for that.
Deborah: I felt the same way. Sure, we neither had any previous illnesses, but due to our work in the health department and our studies, I have not seen the doctor as the “demigod in white” for a long time. I am aware that there is currently no drug available for COVID-19 and that the doctors try their best in an emergency, but also do not have very many options. So it was a bit depressing, but you could easily distract yourself. I also always hoped that I wouldn't get a toothache by chance or get injured in some other way and need a doctor. Of course that would have worked somehow, but as a COVID-19 sufferer, you don't like being treated so much.
: Who helped you?
Deborah: On the medical side, we were looked after by the infectiologists from the health department. Since we had also worked there and the test was taken there, they continued to look after us. It was good to know that we can contact them at any time if we had difficulty breathing or other symptoms. Since we could no longer leave our apartment, our neighbors and friends went shopping for us. Otherwise we weren't restricted and didn't really need help.
Joanna: Of course, contact with family and friends via telephone and video chat also helped a bit against loneliness. Although you have to say that you still felt very isolated and isolated.
: How was the quarantine for you?
Deborah: In our case, the quarantine was definitely the worst part of the whole illness. There were three of us in a 54sqm apartment and at the time the weather was absolutely fantastic. We couldn't even go down to the mailbox or the garbage cans without hesitation. In a big house with a garden, things would have been much easier. It was especially difficult for us to have to sit inside all day in this weather. When we were tested again after 14 days of quarantine, at least I was negative and was finally allowed out again! It was an incredibly liberating feeling.
Joanna: Yes, Deborah already suggests it. For me, the quarantine was a really grueling process. Sure, in retrospect it sounds really cool: sitting at home, no longer having to work and others also shop for you. But I was still positive after 14 days, even though I no longer had any strong specific symptoms. So I stayed home for the third week and then did another test. Until I finally got my negative test result after a lot of phone calls back and forth, I had been in quarantine for about 3½ weeks. Sometimes I felt like I was in a luxury prison. The last few days I was all alone because my sister was allowed out again. It helped me keep telling myself how grateful I should be not to be seriously ill.
: What was the worst in the quarantine?
Deborah: As I said, the worst part was the isolation from the outside world. That even in the best of weather you couldn't see a minute of sun, go running or see friends. We were also no longer able to work in the health department, so we didn't have a really regular daily routine. But I still forced myself to get up relatively early and use the time for meaningful things.
Joanna: It was similar with me too. Fortunately, I was able to work on my doctoral thesis from home and occupy myself so meaningfully. Actually, I sat at my desk for weeks from morning to evening, as I had no more appointments.
: How are you today?
Joanna: We're doing very well! So far, we have not noticed any long-term effects or the like and are now enjoying the status of having the infection behind us a little. You can't be absolutely certain about immunity and of course we still adhere to all hygiene rules and, for example, continue to wear a face mask at all times at work. However, we now trust ourselves to visit our parents, which we had not done before the infection.
Deborah: You definitely feel freer and also enjoy the freedom to go outside a lot more than before.
Addendum in July:
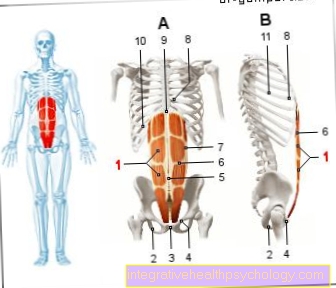
Joanna: In the past few weeks we both had a control MRI of the heart as part of a COVID-19 study at the university hospital. It turned out that we both have myocarditis, i.e. inflammation of the heart muscle and pericardial effusion. This means that fluid has collected in the pericardium. In addition, scars were found in at least my heart muscle.
Deborah: We didn't notice it and we don't have any symptoms now either. In 6 months we will have another check-up appointment, hopefully none of which will be seen on the heart. Until then, we make sure to only do moderate sport and not to overload ourselves.
: Have you suffered from COVID 19?
Deborah: As I said, we haven't noticed any late effects so far. We signed up as test subjects for a study on COVID-19 recovered patients. Next week we will have an MRI appointment in connection with the study to check for potential consequences on organs. But we have no restrictions!
Addendum in July:
Joanna: During the last interview, Deborah had already mentioned the upcoming MRI appointment. During this, each of us was diagnosed with myocarditis and pericardial effusion. Since neither of us have any symptoms, we are not particularly restricted in everyday life. In any case, it is unsettling.
Deborah: When it comes to sports, we try not to overload ourselves and take things a little easier. It's a shame, but as long as we can do sport as usual next year, everything will be fine. Hopefully the inflammation and effusion in the pericardium will subside within the next six months without any consequences!
: What would you do differently next time?
Joanna: Oh dear, that's a pretty tough question. As such, next time I would perhaps have less confidence in being reliably contacted when the test results were available. As a patient without connections, however, you don't have much leeway. Whether you get a call or not is not up to you.
Deborah: I also find the question difficult to answer. We couldn't really change all the things that didn't go optimally or that depressed us.
: What are your most important tips for other sick people?
Deborah: It depends a bit on the symptoms and circumstances, of course. You should probably not worry too much and start treating the condition the same as you would a common cold or flu. If you have a garden or a roof terrace, distraction while gardening or lying in the sun is definitely good. Of course only if you only have mild symptoms! For example, if you experience shortness of breath, you shouldn't be afraid to contact a doctor.
Joanna: In order to survive the quarantine well, I would recommend to come up with a daily schedule and to go through it roughly. Otherwise you will feel at some point as if you were just vegetating to yourself. If you can't work from home, you can do your own projects. Learning a new language or tackling the windows that you've always wanted to clean.
: Thank you for the interview, all the helpful information and tips for those who might be affected!










.jpg)