Burning in the genital area
introduction
Burning in the genital area is by no means uncommon and occurs in many women and men at least once in a lifetime. Burning sensation can mean a tingling sensation with a slight, permanent burning sensation and itching on the outside of the genitals or the vaginal entrance. Another form of burning is the sharp burning sensation when urinating in the urethra. In most cases, both forms indicate an inflammation, which can have various causes, shapes and courses.

causes
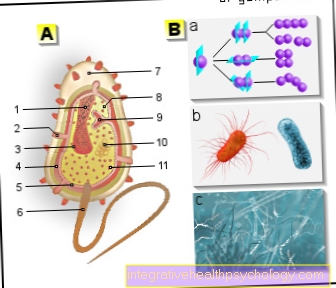
A burning sensation in the intimate area can be the result of dermatological diseases (skin diseases), mechanical irritation, injuries and chronic diseases. However, the most common cause of the uncomfortable burning sensation is inflammation caused by the pathogen.
Inflammation in the genital area can have very different causes and be localized in different ways.
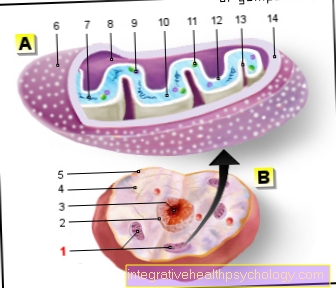
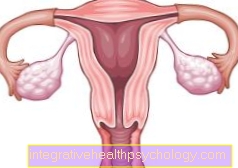
The vulva with its pubic mounds and labia but also the vaginal entrance are usually summarized under the genital area. This area is characterized by the fact that it consists largely of sensitive mucous membrane and is coated with acidic vaginal mucus with pH values of around 5.
At the same time, the intimate area is increasingly exposed to germs, for example faecal germs and mechanical stimuli, for example during sexual intercourse. If you experience frequent pain, itching or burning sensation during or after intercourse, you must urgently seek clarification from your gynecologist.
Pathogens that cause so-called "vulvitis", inflammation of the vulva, penetrate the mucous membrane through the anus, during sexual intercourse, by scratching, increased sweating or due to excessive intimate hygiene and trigger the inflammation there.
The low ph value of the vagina prevents the majority of infections, but through small damage to the mucous membrane or washing the genital area with conventional soaps, the pathogens can still lodge in the mucous membrane.
Even non-infectious causes can lead to itching and burning in the genital area. Chronic skin diseases are less common. Neurodermatitis or lichen sclerosus cause, among other things, these complaints of the vulva and vagina. These diseases appear to arise without a cause and can often only be suppressed but not cured.
In the case of burning pain, mechanical irritation must also be considered. Sexual intercourse, the use of sex toys, the wearing of certain textiles, the use of creams that are not suitable for the genital area, and careless genital shaving can all irritate the intimate area and cause a burning sensation.
You might also be interested in this topic: Sexually Transmitted Diseases
Burning sensation from stress
Stress can affect health in several ways and trigger a wide variety of symptoms. Severe stress can be physical or psychological and can influence night sleep, the cardiovascular system and the immune system via various mechanisms. Stress also affects vaginal health. In addition to a generally slightly reduced immune defense, stress can also reduce the formation of lactic acid bacteria to protect the vagina. This reduced pathogen defense makes it harder to fight bacteria, viruses and fungi and lodge in the vaginal mucosa. This can lead to vulvitis but also to “colpitis”, vaginal inflammation or inflammation of the urinary tract. Urinary tract and bladder infections can also make themselves felt as a burning sensation in the genital area.
Concomitant symptoms
Inflammation is usually characterized by redness, swelling, pain, overheating and impaired function. These typical signs of infection also appear on the vagina and vulva. The pain can be permanent or it can be caused by urination, sexual intercourse, or other touch. In many cases, pain and burning are accompanied by itching. Depending on the type of inflammation, moist, milky, but also purulent discharges from the vagina can also occur. Changes in the mucous membrane with cracked skin, rashes, blistering and crumbly secretion are often not visible externally. Depending on the type of pathogen, an unpleasant odor can also occur. Especially with vaginal thrush or certain sex diseases, this occurs more frequently.
Illnesses that affect the entire body can be accompanied by other symptoms. For example, neurodermatitis typically manifests itself in many other skin and body areas in addition to the vulva. Gonorrhea caused by bacteria can be accompanied by conjunctivitis in the eye, among other things.
itching
Itching is a very uncomfortable symptom that can appear in the genital area. It is created by certain messenger substances such as histamine, which are released in the skin. In addition to certain inflammations, the causes are also poisons, for example insect venom, or poisons produced by pathogens. In most cases, itching in the genital area is harmless, but sometimes it can be due to a disease such as atopic dermatitis or infections such as genital herpes or vaginal thrush.
Even if it becomes very uncomfortable, it is important not to scratch despite the itching. Otherwise, small skin defects can worsen the itching and damage the mucous membrane, which in turn promotes further infections.
Read more about this under: Itching in the vagina
Burning sensation during pregnancy
Apparently harmless infections in the genital area can pose a high risk during pregnancy and pose a danger to the child. However, due to prenatal care and a high level of hygiene awareness, life-threatening diseases have become very rare.
However, bacterial and viral infections in the mother's genital area are particularly dangerous for the child. In addition to the sexually transmitted diseases syphilis, gonorrhea and chlamydia, viral diseases such as rubella, chickenpox, herpes, HPV, mumps and measles are particularly dangerous. The pathogens can reach the child via the bloodstream or via the vagina and disrupt its development or endanger the pregnancy. Each pathogen poses different dangers at the time of pregnancy. While some pathogens lead to developmental disorders in the child, especially in the first few months, some acute bacterial pathogens can cause premature births and other complications in the later months. If there is a burning sensation in the genital area during pregnancy, a clarification by the gynecologist must urgently take place.
therapy
Which remedies help against burning sensations in the genital area?
The means used must be adapted to the underlying cause of the burning sensation in the genital area. Proper intimate hygiene must be learned to prevent future complaints. Under no circumstances should this be carried out permanently with non-acidic soaps, otherwise pathogens can colonize. Furthermore, targeted drugs must be taken to combat the pathogens. Typical antibiotics that help against the most common responsible bacteria are so-called "cephalosporins". So-called anti-viral drugs are used to combat genital herpes and other viral diseases. If the cause is an estrogen deficiency, this can also be treated with medication with replacement hormones. Chronic, autoimmunological skin diseases of the vulva must be controlled symptomatically with immunosuppressive drugs, depending on their severity.
Antibiotics to treat genital burning sensations
Antibiotics are drugs that are specifically directed against bacteria and destroy them or stop them from growing. Antibiotic therapy may therefore only be used in the case of bacterial inflammation, but not against viruses, fungi, parasites and other causes of illness. Intestinal bacteria are increasingly found in the intimate area of women due to the close proximity to the anus. Inadequate or incorrect intimate hygiene, the bacteria normally found in the intestine can trigger inflammation of the vaginal mucosa. In addition to the typical intestinal bacteria, streptococci and staphylococci are the most common causes.
Bacterial inflammation can also be found among the typical sexually transmitted diseases. Gonorrhea and syphilis are bacterial diseases that are transmitted through sexual intercourse. A so-called "antibiogram" can be drawn up with the help of a swab of the inflammation to precisely identify the germ, which determines the resistance and effectiveness of individual antibiotics. A targeted therapy can then be started with a specific antibiotic. In the case of unclear infections, antibiotics should be handled with care, as the use of unnecessary and incorrect antibiotics in recent years has resulted in more resistant bacteria.
Which ointments can help?
In the case of localized inflammation, irritation and discomfort, in addition to medication in tablet form, ointments can also be used. They have the advantage that they do not work in the entire body and the active ingredients can be dosed higher in the genital area. An infection with a vaginal yeast infection can typically be treated with an ointment. So-called "antifungal" ointments are also used. Viral diseases such as herpes are also increasingly being treated with ointments. In the case of local rashes and chronic skin diseases, the immunosuppressive active ingredients in the form of the ointment can act locally in high doses. This has the great advantage that the sometimes severe side effects of therapy for the entire body do not occur.
You may also be interested in this topic: Vaginal fungus
Home remedies
Valuable resources can be used in the household to combat symptoms in the genital area to reduce symptoms or to prevent infections and other diseases. However, self-treatment with home remedies must not be used for highly acute inflammations. Bacterial infections often cannot be adequately treated with home remedies.Yogurt, coconut oil, olive oil, sage and chamomile can be used to relieve symptoms of burning and itchy genital areas. These are either applied directly to the genital area or dissolved in a bath. Diluted soda baths and vinegar rinses can be used to support the vaginal flora in fighting germs. They lower the pH value of the vaginal mucous membrane and thus support the body in its natural fight against germs.
However, the most important measures must be applied over the long term to avoid any inflammation in the genital area. For this purpose, regular but not daily cleaning should be carried out without alkaline soaps. Furthermore, hygiene should be a priority when changing underwear and when using the toilet. Scratching and other causes of mucosal damage to the vagina should be avoided whenever possible. If these measures are followed, the body's own defense system is usually strong enough to fight off pathogens itself.
diagnosis
The most important steps in the diagnosis are the exact inquiry of the complaints and the physical examination. On the basis of the symptoms, chronic skin diseases, external irritations and pathogen-related inflammations can often be differentiated. Individual infections can also be differentiated based on the exact symptoms. While bacterial infections from streptococci and staphylococci are often rapid, fungal infections often occur more slowly and cause more itching. When diagnosing a burning sensation in the genital area, questions about the sexual past, intimate hygiene and other factors that can promote inflammation are always part of the diagnosis.
A diagnosis of vaginal inflammation can also be made with a so-called "colposcopy". This is a microscope that the doctor can use to examine the inside of the vagina more closely. If an infection is suspected, the exact pathogen can be determined with a smear. An antibiogram can be performed to determine the appropriate antibiotic in the case of bacterial infections.
Read more about this here: Vaginal infection
Burning time
The duration of the burning sensation in the genital area depends on the underlying disease and is therefore very variable. A slight burning sensation with itching is often due to minimal mucosal lesions in the genital area and subsides after hours to a few days. If there is a minor infection behind it, this can also be cured in a few days. Bacterial infections can be persistent, especially the typical sexually transmitted diseases. If they are recognized and treated with antibiotics, healing is possible within a few days. Even fungal infections can clear up within a week with the right treatment. Longer-term courses, however, take on skin diseases such as neurodermatitis or other eczema. Even with the right treatment, they can often only be controlled symptomatically but not cured, which is why relapses and new rashes can occur again and again.
You may also be interested in this topic: Eczema in the genital area- causes and treatment