Heart bypass
definition
A bypass at the heart is a diversion of the blood around narrowed and no longer continuous vascular sections of the heart (so-called coronary arteries).
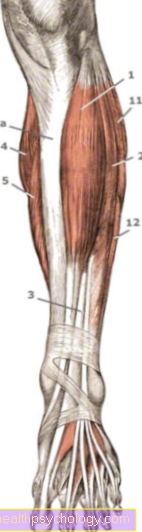
One can compare a bypass with a diversion in traffic at a construction site. In the case of a bypass, a blood vessel is removed, usually from the leg, the constriction of the cardiac artery is bridged and the ends of the inserted vessel are sewn to the heart vessel in front of and behind the constriction. The blood flow to the heart is guaranteed despite a blocked cardiac artery.

Indications
In the past, a bypass was the only way to ensure proper blood flow to the heart in the event of a constriction (stenosis) or a complete blockage (infarction) of a cardiac artery. Today there are other corresponding ways of doing this, so that today a bypass operation is only performed when a coronary artery is so narrow that no other measures can be carried out or when the vessel is completely closed. Even if there are contraindications to an alternative treatment measure, bypass is considered.
In order to decide whether to use a bypass or one of the alternative treatments, a number of criteria are considered. For example, whether it is a constriction of a main branch or a secondary branch of the coronary arteries or whether there are one or more constrictions.
How severe is the narrowing? Is it a complete occlusion or a slight constriction? What causes the narrowing? Is it a calcium deposit or is the narrowing caused by a blood clot?
One of the most important criteria is the length of the vessel section that is narrowed. A short constriction is usually supplied with a stent, while longer constrictions usually have to be bypassed in order to ensure the blood flow again. Another important criterion for whether a bypass operation should be performed is the patient's state of health. In older patients with many secondary diseases, one would rather refrain from a bypass operation, as this is very stressful for the body. The decision also takes into account how urgent the procedure is. Acute circulatory disorders are usually treated in an emergency with a stent placed in the cardiac catheter laboratory.
The most common cause of a narrowing of the coronary arteries is the so-called coronary heart disease (CHD).
Read our article on this: Coronary heart disease
Diagnostics before bypass surgery

The diagnosis of whether a bypass operation must and can be carried out is made on the basis of the patient's clinical complaints and confirmed with the help of a contrast agent display of the cardiac arteries.
The cardiovascular system is shown using a cardiac catheter examination (coronary angiography). Here, a wire is pushed over the vascular system to just before the heart via the inguinal artery (femoral artery) or an arm artery (radial artery). Once there, a contrast agent is injected into the patient's coronary artery system. This spreads in the vascular system within milliseconds.
With an X-ray device that is pushed over the patient, images are now made that represent the contrast medium. There is a narrow point where gaps and dark spots can be seen in the course of the vessel. With complete occlusions, the contrast agent cannot flow through the vessel at all. Here you can see a break in the white contrast medium course.
Nowadays, thanks to new treatment methods, such constrictions can be treated immediately with a stent. A bypass operation is therefore not necessary. In the case of complete occlusions, the catheter examination is ended after the diagnosis has been made and a bypass operation is usually planned.
Read more about this: Cardiac catheter
Symptoms
When bypass is necessary, deposits have narrowed or blocked arteries that supply the heart. The first symptoms of cardiovascular narrowing usually appear under pressure on and are Pressure on the chest, shortness of breath and shortness of breath, irregular pulse such as Reduction in performance. If the arterial system of the heart is severely narrowed, the symptoms appear even at rest.
Corresponding risk factors for vasoconstriction can often be identified in the patient. These include smoking, being overweight, high blood pressure and comorbidities like Diabetes mellitus. Most of the time, the patients state that they were able to climb stairs a few months ago and are now suffering from symptoms in peace.
If a vessel is completely closed, this corresponds to a Heart attack with severe pain in the chest, radiation in the jaw and / or left shoulder, shortness of breath and sweating. A heart attack is an absolute emergency that needs to be addressed as soon as possible.
The operation
Surgical techniques
In the past, bypass surgery was always performed on the open heart. Here was the heart stopped (Cardioplegia) and the body's blood supply from one Life-support-machine accepted. This technique is still widely used today.
A modification of this is the bypass OP on the open, but hitting Hearts. No heart-lung machine is required and the bypass is carried out on the beating heart. This measure is usually taken when the vessels and the aorta are so strongly calcified that the heart-lung machine cannot be clamped and thus put on.
Nowadays the minimally invasive Bypass surgery, i.e. the operation is no longer performed on the open heart and the chest remains closed. Instead, the operation is performed through a small incision between the ribs (Keyhole technology) carried out. When using artificial heart valves This gentle surgical technique has already established itself and is now performed regularly. The advantage of the minimally invasive surgical technique is that it is gentler and has complications such as wound healing disorders less common occur. In the course of the operation, however, it may be necessary to carry out the operation on an open heart due to the anatomical conditions (poor visibility, etc.). Then the keyhole method that was initially started is broken off and the chest is opened.
Bypasses through the traditional open method and the newer keyhole method differ in outcome not essential from each other. With the open surgical method, it can also lead to wound healing disorders Inflammation of the sternum come. In contrast, with the minimally invasive keyhole technique, because of the smaller access, the ribs have to be spread many times, which as side effects can lead to more pain in the follow-up treatment.
In 2002 just 1% of all bypass operations were performed with the keyhole technique. The proportion of minimally invasive operations has meanwhile increased, but has not yet replaced open heart surgery. In the opinion of the scientists, this is because the advantages of a minimally invasive technique over open surgery are currently not as convincing as hoped.
Due to the low rate of complications in standing heart operations, the minimally invasive surgical method can only score insignificantly in this aspect. Where it clearly leads, however, is the cosmetic result. While the open bypass operation leaves a wound with a subsequent scar of approx. 30 to 40 cm on the breastbone, with the minimally invasive technique only a scar of a few centimeters remains.
Procedure of the operation
Bypass surgery is necessary when one or more coronary arteries are blocked. During the operation, a replacement vessel produced by the body (a vein from the lower leg or an artery from the arm) is used as a diversion. Before the blockage, the vessel is connected to the main artery and behind the blocked area again connected to the affected coronary artery. This creates a diversion that ensures the supply of the heart muscle behind it. Every bypass operation takes place under general anesthesia.
In the standard operation, the chest is opened first, as this is the only way to ensure access to the heart. The patient is connected to a heart-lung machine that can replace the heart for a period of time. Since beating heart surgery is extremely difficult, the heart is immobilized with medication. Newer surgical procedures allow a bypass operation without opening the chest. It is also not always necessary to use the heart-lung machine. If this is not done, the bypass must first be attached to the blocked coronary artery. Then the main artery is partially clamped off and the bypass is sewn on. The clamp is then removed again.
Duration of the operation
When using the standard surgical procedure, the duration of the operation is usually around three hours. A similar duration of surgery can be assumed for minimally invasive surgical techniques. In general, the duration of the operation depends on how many bypasses are to be constructed. On the one hand, every bypass needs additional time when removing the vessel from the arm or leg. The operation time is longer, especially when several bypasses are used from different parts of the body.
In addition, depending on the location, “installing” the bypass on the heart is time-consuming. For example, it is more difficult to get to the back of the heart, which is why a bypass at that point takes longer than a bypass at the front wall.
The preparation and follow-up work can also be counted towards the duration of the operation. A medication is usually given about an hour before the operation, which makes you tired and has a calming effect. The operation itself then begins with the induction of general anesthesia, after which the operation on the heart can be performed. It usually takes another 10 to 30 minutes to wake up from the anesthetic after the operation.
OP costs
During the minimally invasive use of a Stents approx. 17,000 EUR costs is with one Bypass surgery at a cost of up to 30,000 EUR to be expected. The cost difference of the pure surgical method is small, but due to the somewhat longer follow-up treatment one open Surgery (wound care, drainage insert, etc.) the costs may be higher.
On the other hand, the more complicated training methods that surgeons use to specialize in the keyhole surgery technique are costly. Here is a Surgical robot necessary, the cost of which is approx. EUR 1 million and which not every center can afford. The training costs for the minimally invasive operation are currently much higher, which makes the costs for the open bypass operation lower in comparison.
Risks of the operation
Another disadvantage of the minimally invasive method is the more precise and demanding monitoring of the patient during the procedure. Since the operation is performed on the beating heart, special care must be taken for possible Irregularities in the circulatory system placed during the procedure. Also the risk of injury from Vessels and or Nerve cords during the procedure, the Keyhole technology described as elevated because the cardiac surgeon lacks the usual view of the open surgical field.
With the open surgical method, however, there are more frequent wound healing disorders and complications due to the massive opening and spreading of the chest.
Despite the almost identical results with open and minimally invasive bypass surgery, it should be noted that several bottlenecks can be bridged with the keyhole technique, but not 4-5 as with open surgery. Critics point out that this is where the minimally invasive bypass operation reaches its limits, as a large number of bottlenecks make a bypass operation necessary.
The standing heart procedure takes about 3-6 hours, depending on the vessels to be operated on and the general condition of the patient. The duration of the minimally invasive surgical technique is somewhat shorter because there is no need to open the chest and connect the heart-lung machine.
Advantages and disadvantages of the minimally invasive technique
With the minimally invasive technique, a distinction must first be made between two procedures: There is the Minimally Invasive Direct Coronary Artery Bypass (MIDCAB), in which the sternum does not have to be opened. With the Off Pump Coronar Artery Bypass (OPCAB), the breastbone is opened.
The advantage of both minimally invasive techniques is the significantly lower operative stress, which promises faster and better recovery after the operation.
The higher technical demands on the surgeon are seen as a disadvantage. Another great advantage of the MIDCAP technique is that the sternum does not have to be cut. This also reduces the stress caused by the operation. The major disadvantage is that with this surgical technique only the front of the heart can be reached, which is why only some of the affected people can be treated with this procedure. The OPCAB technology, on the other hand, allows access to both the front and the back of the heart, but is still not as stressful for the body as conventional surgery. However, the greatest danger with this technique is that it can impair the heart's pumping capacity during the operation. In principle, both minimally invasive surgical techniques can be performed without the heart-lung machine.
How long do you stay in the hospital after bypass surgery?
The hospital stay for a bypass operation is usually around three weeks. As a rule, you are admitted to the hospital one day before the operation. Immediately after the operation, affected persons are carefully monitored in the intensive care unit for two to three days. The monitoring of the heart rate and the heart rhythm is particularly important. If there are no problems in this early phase after the operation, further monitoring takes place on the normal cardiological ward. The stay there is usually around three weeks, but is extended if necessary, for example in the event of complications or complicated concomitant illnesses.
In most cases, rehabilitation immediately follows the hospital stay. This rehab takes place in a special clinic and usually lasts about 3 weeks, during which rehabilitation procedures take place five to six hours a day, five to six days a week. Due to the large amount of time required and the daily treatment, rehabilitation almost always takes place in an inpatient setting. In exceptional cases, affected people can stay at home again, but they have to come to the rehabilitation clinic every day for their therapies.
Rehabilitation after bypass surgery
Rehabilitation usually follows the hospital stay after a bypass operation in the form of follow-up treatment (AHB). Due to the long and open operation, affected patients are exposed to a great deal of stress, which must also be treated in detail in the subsequent period. As a rule, the heart disease and the operation not only represent a high physical strain. The psyche is also usually affected and is therefore also taken into account in rehab.
Rehabilitation usually takes place over 3 weeks in an inpatient setting. However, outpatient rehab is also possible in principle, provided that those affected are able to come to the rehab clinic independently on 5-6 days a week. The program consists of extensive physical training, which includes physiotherapy and occupational therapy, conditioning training and various gymnastics exercises. In addition, great importance is attached to the education of those affected.After a rehab, everyone should have detailed knowledge about healthy eating, obesity and its prevention as well as about the various medications used. Depending on requirements, independent care and, if necessary, a return to work should also take place after the rehabilitation, so that these socio-medical factors also play a major role.
The psychological component of rehabilitation is primarily concerned with relaxation procedures, but should also address the issues of coping with anxiety, depression and pain after the operation. The various rehabilitation programs usually take place in both group and individual training sessions.
How long are you on sick leave after bypass surgery?
The duration of the sick leave after a bypass operation is at least 6 weeks. This is the time that affected people spend in hospital and then in a rehabilitation facility. Ideally, the ability to work is restored, especially during the stay in the rehabilitation clinic. In particular, people with physically demanding jobs are usually on sick leave for a long time. After a bypass operation, the body must first be trained again until it can reliably carry out the corresponding stresses of everyday work. If heavy physical work is necessary in an occupational field, retraining in a less stressful occupation may be necessary.
Is bypass surgery possible without a heart-lung machine?
Bypass operations without a heart-lung machine are technically demanding heart operations. The heart-lung machine is supposed to take over the pumping function of the heart while the heart is immobilized with medication. In this way, a calm surgical field on the heart can be guaranteed. The heart-lung machine is often not used in minimally invasive procedures. In this case, the bypasses must be used on the beating heart. The bypass is first attached to the affected coronary artery. The main artery is then partially pinched off and the bypass is sewn into the pinched off area.
The alternative: stent
The alternative to bypass surgery is this Stent placement. Nowadays, this method of treatment has become established and is carried out several times a day in all cardiac catheter laboratories.
A stent is a thin wire frame in the form of a cylinder that is initially in a folded state. If there is a suspicion of a coronary artery narrowing, a cardiac catheter examination is carried out. This also as Coronary angiography known procedure is initiated through the patient's inguinal artery. A thin wire is pushed over the patient's arterial vascular system to just before the heart. Contrast medium is then injected into the vasculature of the heart. Vacant areas are colored light, constrictions are left out and dark.
If the vessel is only narrowed and not occluded, the folded stent can be advanced over the wire into the narrowed vessel of the heart. If it is positioned in the constriction, it is unfolded and thus expands the constricted vessel. Several stents can also be introduced into the vascular system in one session.
A distinction is made between stents that have a drug film and those that are uncoated. Coated stents usually carry anticoagulant drugs, so that a new clot formation in the vessel is counteracted.
The procedure takes about 30 to 60 minutes and is now the standard treatment for a heart attack.
Risk of stem implantation
Stenting is a relative low risk Procedure that is carried out several thousand times a day in Germany. However, like any intervention, it carries a statistical risk.
As the catheter is advanced in the arterial section of the body, it can happen that small blood clots form in the area of the entry point or in the area of the catheter. These blood clots can also be pushed forward towards the heart by the catheter and can thus lead to a complete blockage of a blood vessel, which triggers an acute heart attack.
The procedure can also cause blood clots to spread in the body and, for example, in the brain stroke to lead.
Furthermore, it can become too during the procedure Cardiac arrhythmias come, some of which can also assume life-threatening proportions. It may then be necessary to undertake appropriate resuscitation measures. The patient is monitored on a monitor during the procedure, so you can react very quickly. Lighter cardiac arrhythmias are and are relatively common easily controllable. More serious and / or life-threatening arrhythmias are less common. In the worst case, cardiac arrest can occur during the procedure.
Prognosis after stent placement
After a stent has been implanted, patients have a good prognosis.
The greatest danger is the stent becoming blocked by blood clots or renewed vascular deposits. The continuous improvement of the materials used has significantly reduced this risk. It must be from a danger of 1-2% it can be assumed that a part of the arterial vessel that has been dilated by a stent will narrow again within 4 years (so-called "restenosis"). This risk was higher with previously used stent materials and could amount to 5-7%.
Of course, it is important and decisive that a corresponding essential combination of medication is taken correctly, which usually consists of at least 2 Anticoagulants consists. In addition, a Cholesterol lowering drugs to be taken and on an accurate Lowering blood pressure be respected.
The laying of a stent leads to the same symptoms as a vasoconstriction, namely to a feeling of pressure on the chest at rest or during exercise, to pain, shortness of breath and an irregular pulse.
Patients who have been stented should pay close attention to symptoms such as those preventive Medication Consume continuously and reliably and regularly Check-ups with your cardiologist.
What is the life expectancy with a bypass?
Life expectancy with a bypass depends on many different factors, which is why it is not possible to make a general statement about life expectancy.
Of course, bypass surgery increases life expectancy when compared to people who do not have surgery. Survival of the bypass will vary depending on whether arteries or veins are used. In general, arteries last longer, with veins about 30% of the vessels are blocked again after about 10 years. However, there are many people who have successfully lived with venous bypasses for over 20 years.
There are some studies that have compared stent insertion to bypass surgery. However, this does not provide any reliable data that would suggest the superiority of either method. One can therefore assume that the life expectancy with a bypass is comparable to the life expectancy after insertion of the stent. Overall, life expectancy depends in particular on other diseases such as hypercholesterolemia (high blood lipid levels) or diabetes mellitus (diabetes). It also plays a major role whether affected people change their lifestyle through a healthy diet and physical activity.
You can find more about this on our website What is life expectancy with a bypass at heart?