Chemotherapy for breast cancer
introduction
There are various therapy options for patients with breast cancer.
Which type of therapy or which combination of several forms of therapy is best suited for the respective patient varies greatly and must be clarified individually for each individual case.

In principle:
- chemotherapy
- Irradiation
- Hormone therapy
and or - an operation available.
Which therapy the doctor will choose depends on various factors, including the age of the woman and whether or not she had her last menstrual period, the tumor size, certain tissue properties of the tumor, the extent of metastasis (spread) of the tumor and the hormone receptor status .
Read more about the here Therapy for breast cancer.
Types of chemotherapy
Chemotherapy is used in two different ways. Either as part of a so-called adjuvant or neoadjuvant therapy. Adjuvant means that primary therapy is given first, usually surgery, followed by chemotherapy to prevent recurrences.
In neoadjuvant therapy, the first thing that is performed is chemotherapy to shrink the tumor in order to have better chances with the actual therapy, i.e. the operation.
When do you have chemotherapy before the operation?
Chemotherapy before the operation is only carried out in certain cases. One speaks of a "neoadjuvant chemotherapy". The aim here is also to heal the body from cancer. In these cases, however, the tumor is of such a nature or size that an operation with complete removal is not immediately possible. The neoadjuvant chemotherapy should therefore attack and shrink the tumor so that the operation can be carried out more easily.
Neoadjuvant chemotherapy can also be useful for patients who wish to preserve their breasts. Here, the tumor can be shrunk before the operation so that the complete removal of the breast is no longer necessary.
At the same time, it has been shown that neoadjuvant chemotherapy reduces the risk of relapse after the operation. The chemo before the operation can eliminate small infected cells before it spreads further. The process is similar to post-op chemotherapy. Here, too, several chemotherapeutic agents are combined, which are administered in different cycles with breaks.
When do you have chemotherapy after the operation?
Chemotherapy after the operation is also called "adjuvant chemotherapy" designated. Adjuvant means "supporting". It is used after a successful operation to detect and combat residual cancer cells that have remained unnoticed in the body.
Even if the tumor has been completely removed for the human eye, individual affected cells remain locally in the tissue, in the lymphatic systems or in the body's circulation and can settle and Metastases (Daughter tumors).
Read more about this at: Metastasis in breast cancer
Chemotherapy fights these remaining cells in the entire body as best it can and thus noticeably increases the statistical probability of survival.
At the beginning of chemotherapy, the tumor cells must be carefully analyzed in order to find the most suitable remedy for them and to spare the remaining body cells. Since chemotherapeutic agents always act against healthy cells in the body, the typical side effects of chemotherapy occur.
Several studies have shown that adjuvant chemotherapy can significantly reduce the risk of relapse.
When can I avoid chemotherapy for breast cancer?
The use of chemotherapy is based on large scientific studies that have examined the probabilities of survival and recovery through various therapeutic measures. Chemotherapy therefore has a positive effect on the chance of recovery in very many cases.
Chemotherapy can only be omitted in patients who have a very early stage of breast cancer without any spread to organs or lymph nodes and who have had a successful operation.
There are also certain properties of the tumor. After removal, this can be examined for certain cell structures, which among other things have an influence on the so-called "recurrence rate", i.e. the probability of a relapse after removal of the tumor.
Please also read: Breast cancer recurrence
These cell structures also influence the therapy and the exact type of chemotherapeutic agent. The age of the person affected also influences the therapy decision. Young women can experience long-term fertility complications from chemotherapy.
You can read more about these cell structures and how they can be extracted in our article Tissue samples in breast cancer.
How long does chemotherapy last for breast cancer?
There are several forms of chemotherapy used to treat breast cancer. All have different goals and are deployed at different times.
The most common and typical chemotherapy begins right after the operation. Their duration can vary, but is usually carried out within a maximum of 15 weeks.
The duration varies with
- the condition of the patient,
- the dose of chemotherapy,
- the number of different gifts ("cycles")
- and the breaks in between.
The chemotherapy after the operation includes about 4-6 cycles. A cycle contains a certain dose of medication that is delivered to the patient within a day or a few days. This is followed by a break, during which the treatment takes effect and the body can recover from the side effects.
This can take days to weeks and helps the body recover from the rigors of the therapy.
Some cytostatics (drugs that inhibit cell growth) only work on cancer cells that are in a certain phase of their development. The cycle treatment is also an advantage here, as it increases the likelihood of "catching" the tumor in the right phase.
Chemotherapy is usually administered through the veins (intravenous, i.v.) administered, for which the creation of a port can be useful. Variants with chemotherapy as a tablet are also possible today.
Depending on the success of the therapy, the patient's state of health and the severity of the side effects, chemotherapy can also be carried out on an outpatient basis. This means that patients are allowed to go home during the break between cycles.
Also read our article on that Chances of recovery in breast cancer
What are the chances of success of chemotherapy?
The purpose of chemotherapy is to eliminate cells remaining in the tumor after the operation and thus to increase the chance of recovery. Statistically speaking, chemotherapy can increase the actual lifespan and likelihood of survival, which is why it is still recommended in treatment. The individual decision for or against chemotherapy must still be made dependent on personal factors.
Different types of breast cancer can respond very differently to chemotherapy. Some cell variants are almost resistant to the usual drugs. For this purpose, the cells are carefully analyzed before the start of therapy. Individual wishes must also be taken into account in the decision.
Even if chemotherapy increases the likelihood of a cure by a few percent, the side effects of chemotherapy are reason enough for some sufferers not to carry out the therapy.
You can also find more information about the chances of a cure for breast cancer in our article Prognosis in breast cancer
Administration of chemotherapy drugs
The cytotoxic drugs are usually administered into a vein, i.e. by infusion. This allows them to be distributed well in the blood and thus throughout the body and also to kill tumor cells where they have not yet been discovered.
Some preparations are also available in tablet form. This oral intake has the advantage that patients are spared the frequent trip to the hospital and invasive interventions on the veins, but current studies suggest that therapy with oral cytostatics alone is not as effective as infusion therapy.
Since the chemotherapy drugs are often drugs that strongly irritate the peripheral veins, the patient is often given a so-called PORT.
What is a port?
A port is a central venous access that can be surgically created, especially for cancer but also for other chronic diseases. The port has a small chamber that lies under the skin and can be used for quick infusions, medication or blood draws.
In the case of short hospital stays, a normal central venous catheter, a so-called "CVC", can be inserted. This increases the risk of infection after more than 10 days and the connections are outside the body, which is why it is impractical for long-term use.
Read more about this at: Central venous catheter
The creation of the port is more difficult, but the port can be used for several years. In exceptional cases, the port remains in the body for up to five years.
Each time a patient is hospitalized, the port can be pierced through the skin and henceforth used for blood withdrawals, infusions and chemotherapy. Because the port is under the skin, complications are reduced. However, in rare cases, infections or thromboses of the port and the chamber can occur. Injuries to the pleura or the lungs can also occur when the port is created or removed.
In general, however, the port system ensures that fast and good venous access is always possible, and that medication can be administered safely and easily in emergencies or during chemotherapy.
Read more on this topic at: port
Chemotherapy side effects
There are many side effects associated with chemotherapy, but can now be managed relatively well with various drugs.
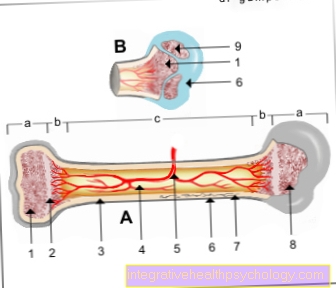
Since the cytostatics are not completely specific for tumor cells, they always damage the body's own tissue, particularly those cells that, like cancer cells, divide quickly. These include hair cells, which is why patients suffer from hair loss, cells of the gastrointestinal tract, which often leads to nausea, diarrhea and vomiting, and cells of the body's defense system, which makes those affected more susceptible to infections. As a preventive measure, a medication against vomiting and nausea is always given, such as Ondansetron.
In addition, there are unspecific complaints, such as poor concentration, tiredness and exhaustion or loss of appetite. These side effects can occur either directly after the therapy or even days or months later and are usually only temporary.
Whether side effects appear, and if so, which ones and to what extent, varies from patient to patient and is difficult to predict in advance.
Read more about this on our website Side effects of chemotherapy for breast cancer.
Hair loss
Hair loss is a side effect that can be expected with almost all chemotherapy treatments. The hair loss also shows that the chemotherapy is working. Most chemotherapy drugs target cells that are rapidly dividing and multiplying. In addition to cancer cells, which often grow particularly quickly due to defects in cell division, hair root cells are also affected.
The blood-forming cells and immune cells can also be affected, as these divide just as quickly. After the treatment, the hair root cells recover and normal hair growth returns.
Please also read: Hair growth after chemotherapy
What can be the long-term effects of chemotherapy?
In addition to the typical side effects such as hair loss, vomiting and increased susceptibility to infections, long-term complications can also occur.
Particularly with young women, certain long-term risks need to be weighed. If the woman wishes to have children, she must be informed about potential damage to the ovaries and limitations in fertility. After chemotherapy, the menstrual cycle may stop altogether and the menopause may occur earlier.
Further long-term effects also depend on the individual chemotherapeutic agent. Various substances can be very harmful during pregnancy or even attack the heart and damage the heart muscle. The medication can rarely cause blood cancer by changing the blood-forming cells.
Read more about this at: Side effects of chemotherapy for breast cancer
Polyneuropathy
A rare long-term complication of chemotherapy is the development of one Polyneuropathy, i.e. damage to several nerves. Typical chemotherapy drugs that can cause this are Capecitabine and Taxanes.
They can attack and damage the nerves outside the brain. The damage may initially lead to tingling, sensory disturbances and numbness in the arms and legs. Later even complete paralysis of the muscles in the extremities can occur.
Read our main article about this Polyneuropathy
Cytostatics
The aim of chemotherapy is to kill as many cancer cells as possible in the body and at the same time to protect the body's own tissue as best as possible. The drugs used in breast cancer chemotherapy are called cytostatics.
For more information on cytostatics, also read our article Cytostatics!
Groups of cytostatics
There are very many different groups of cytostatics, all of which have different starting points. What they all have in common, however, is that they prevent tumor cells from multiplying. Unfortunately, most of these drugs cannot differentiate sufficiently between cancer cells and body cells and therefore generally attack rapidly dividing cells, which is where most of the side effects of therapy with cytostatics result.
Two groups of cytostatics are particularly popular in breast cancer:
- Anthracyclines and
- Taxanes.
Anthracyclines disrupt the structure of the DNA of the tumor cells and thus damage their genetic information. As a result, the cell is no longer able to divide properly.
Examples of this are the drugs Doxorubicin and Epirubicin.
Taxanes are usually administered when metastases have been found in the armpit lymph nodes, often in addition to the anthracyclines.
They too intervene in the division process of cancer cells. This happens because the so-called cell spindles are disturbed in their task of dividing the genetic material fairly between the two daughter cells during cell division. In addition, they damage the genome and the cell wall of the tumor directly. Important representatives of this group are paclitaxel and docetaxel.
Please also read our page Substances used in chemotherapy.
Mono- or combination therapy
Often different cytostatics are combined in therapy to hit the breast cancer as hard as possible. However, this also means a higher burden on the rest of the patient's body.
For this reason, especially in the case of tumors in the advanced stage, monotherapy, i.e. therapy with only one active ingredient, is sometimes chosen in order to ensure that the rest of the body is spared.