The chronic pain syndrome
definition
The chronic pain syndrome is generally understood to be a pain condition that lasts longer than six months.
It is important to differentiate between acute pain and chronic pain.
The acute pain lasts only for a short time and is coupled with a pain event. For example, acute pain occurs when you are injured, but then ends when the wound heals.
The chronic pain is not directly attributable to a direct pain event. Thus, chronic pain has no warning or protective function like acute pain.

Often the chronic pain arises from an acute pain, for example when pain has not been adequately treated. Since the pain has no direct function in this case, the chronic pain syndrome is viewed as an independent clinical picture. In addition, a psychological component often plays a decisive role.
Chronic pain can be the result of a psychological ailment; at the same time, acute psychological pain can also develop into chronic pain through an additional physical component.
The chronic pain syndrome is not a rare disease. Over eight million people in Germany suffer from chronic pain. Therapy is not easy as the pain cannot be caused by a specific event. In acute pain, such an event is often easy to treat. Patients suffering from chronic pain must therefore be treated with many different methods at the same time.
Also read more on the topic: Chronically ill and chronic disease
to form

Basically, you can four different types of pain differentiate each to one chronic pain syndrome being able to lead.
One cause of pain is the so-called psychogenic pain. This pain is not caused by physical injury, but by damage to the psyche. So can mental illness like depression or Delusional and Imagination of fear also lead to pain that needs to be treated.
Neuropathic pain arises from an injury or damage to the nerve itself. In the human body, nerves have the task Sensory and pain perception from the periphery to our brain. If nerves are damaged, one will develop permanent, intense pain experience. Common causes of neuropathic pain are Viral infectionssuch as the Herpes zoster, or diabetes ( diabetes).
Nociceptive pain is the pain we feel when we hurt ourselves. For example it happens with one Cut in the skin for the distribution of substances that the annoy irritate and lead to pain. If such pain occurs over a long period of time, the nerves are overstimulated and a so-called develop Pain memory. This is the basis for the creation of a chronic pain syndrome. People take nociceptive pain equally when there is damage to the body internal organs true.
The last form of pain is that myofascial pain. This goes from the Musculature and can for example at rheumatic diseases occur.
Emergence

Regardless of the origin of acute pain, it can always become chronic if it is not treated or handled incorrectly. Often a psychological component also plays a decisive role in chronic pain syndrome. The development can best be explained with an example.
An imaginary 50-year-old patient suffers from a herniated disc, which causes pain in the buttocks that radiates into the legs. In the initial stage, this is called an acute pain event. Out of stubbornness, he ignores the pain and refuses to go to the doctor in the hope that the pain will go away on its own in a few days. Only after months does the patient go to the doctor who will write him down and refer him to the orthopedic surgeon. It takes a total of six months for the final diagnosis and therapy to be achieved.
This example shows three different ways of developing chronic pain syndrome.
For one, there is a crucial psychological component. By taking a sick leave, the patient is indirectly rewarded for his pain, since he does not only have to go to work. This increases his acceptance of the disease. In addition, the patient notices that he cannot do anything about the pain on his own and develops a feeling of powerlessness along the way. This psychological attitude ultimately favors the development of a chronic pain syndrome.
Men in particular live with the attitude that many clinical pictures subside just by persevering. When they are in pain, they take pain medication much less often than women. But this chronic, untreated pain condition leads to my body getting used to the pain and believing it to be normal. It is said that the body develops a so-called pain memory. This is responsible for the chronification of pain.
A final cause is the physical and mental fixation on acute to chronic pain. Just the idea of being in pain with a certain movement can lead to a perception of pain in the brain. Constantly taking a relieving posture can also lead to the development of a chronic pain syndrome.
In summary, every patient who has been in pain for more than a month should consult a doctor in order to treat the pain and possibly the cause as early as possible. The treatment of acute pain is much easier and more efficient than that of a chronic pain syndrome. Therefore, one should avoid letting it develop into chronic pain.
Accompanying factors
In addition to the main symptom of pain, other accompanying symptoms may occur. Exhaustion and tiredness are not untypical for this disease. Furthermore, the persistent pain can in some cases cause nausea and even vomiting.
Psychological accompanying symptoms play a role that should not be neglected in chronic pain syndrome. Anxiety disorders, depression or somatoform disorders are often an accompanying symptom. The somatoform disorder describes a clinical picture in which physical disorders exist without an actual organic disease being present.
If a stressful situation occurred before the chronic pain developed or if the pain is perceived as particularly stressful, a post-traumatic stress disorder can develop.
In some cases it can be difficult to determine whether the psychological symptoms are an accompanying reaction to the pain or whether they are the triggering factors.
Psychosomatic factors
The guiding principle of psychosomatic medicine is to link physical damage or symptoms with one's own psyche. It is believed that physical symptoms are triggered or influenced by psychological factors.
The human psyche also plays an important role in the development of chronic pain. This will be explained further under the aspect of causes.
Your own perception of pain can be influenced by past events as well as current events and changes the perception of a normally short-term pain so that it becomes chronic.
Psychological risk factors that can support this chronification are, for example, persistent stress or other pain experiences in the past.
Interestingly, initially ignoring the pain or inconsistent treatment of pain can also play a key role in making it chronic as it progresses.
You might also be interested in this topic: Psychosomatic pain- can you imagine pain?
Protective psychological factors that have a positive effect on pain are social support, especially from a partner. In addition, a positive attitude and acceptance of pain can have a healing effect on it.
causes
Chronic pain syndrome is a very complex clinical picture and the causal factors are not yet fully understood. Often the exact cause of the chronic pain cannot be found either.
However, we know some factors that can lead to the development of a chronic pain syndrome.
For example, long-term pain caused by accidents, tumor diseases or amputations can lead to certain changes in the body. As a result, pain is no longer a symptom of a superordinate disease, but is now a disease in itself.
The pain persists even if the original underlying disease is considered to be cured or adequately treated.
Neuropathic pain, also known colloquially as nerve pain, can, if the initial treatment is inadequate, affect pain memory. This creates chronic pain that is difficult to treat.
Finally, incorrect handling of pain, for example in the case of extreme fixation or depressive disorders, can lead to a chronic pain syndrome. Psychological factors can also trigger chronic pain on their own without a disorder in the body being able to be found here.
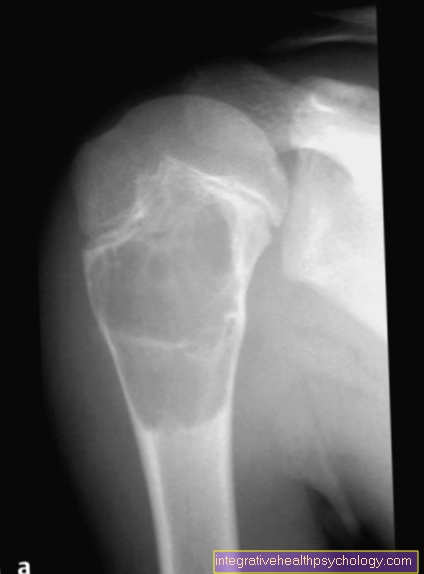
Spinal stenosis

In medicine, a stenosis is generally understood to be a narrowing.
In spinal canal stenosis, the spinal canal is narrowed, i.e. the space in the spine in which the spinal cord runs. The spinal cord is a bundle of nerves that can react with pain through compression.
A common cause of spinal stenosis is a herniated disc. The core of the disc presses on the spinal cord and causes pain.
As long as there are no neurological symptoms such as paralysis or sensory disturbances in the back, buttocks or legs, stenosis is usually treated conservatively. This includes physical therapy and pain medication.
Only one operation is available as the last step in therapy.
Read more under our topic: Surgery of a spinal stenosis
If the pain is not adequately treated, there is a possibility that it will become chronic. This means that the patient still has pain even after the spinal stenosis has been successfully resolved. These can last a lifetime and must be treated, as chronic pain can often lead to mental exhaustion and depression and even the risk of suicide.
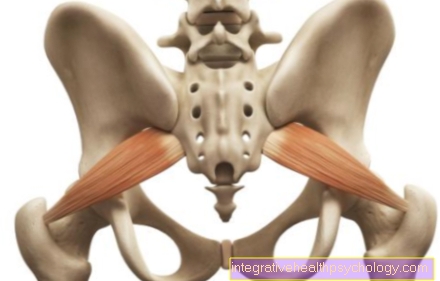
Chronic pelvic pain syndrome
Chronic pelvic pain syndrome describes a condition that is characterized by prolonged pain in the pelvic area and lower back.
The disease occurs more frequently in men after the age of 50 and is formally part of the clinical picture of bacterial prostate inflammation (prostatitis), even if the cause of the chronic pelvic pain syndrome is not a bacterial infection.
Chronic pelvic pain syndrome is defined as pain in the pelvic area that has lasted for more than three months and is accompanied by complaints of the prostate. Furthermore, a distinction is made between an inflammatory and a non-inflammatory form of chronic pelvic pain syndrome.
The exact cause is unclear and often cannot be fully explored in the patient. Symptoms are the eponymous pelvic pain, problems urinating and erectile function disorders.
The diagnosis is made based on a medical history along with a physical examination of the pelvis and urine examination. In addition, the ejaculate can be examined and a transrectal ultrasound of the prostate can be performed. During this examination, a probe-shaped ultrasound head is inserted into the rectum, which improves the resolution of the prostate.
Therapy is limited to symptom relief. For example, medication for urination discomfort and painkillers can be given.
Classification according to ICD
The ICD (International Statistical Classification of Diseases and Related Health Problems) is an internationally used classification system for diseases. This standardization is important in order to be able to make uniform diagnoses. It also plays a crucial role in billing with health insurers.
Chronic pain syndrome and its sub-forms are also listed in the ICD. A distinction is made precisely according to the background and the severity of the clinical picture. The problem is that mental illnesses are not listed in the ICD. However, chronic pain syndrome often has a psychological component.
It has also been proven that psychological involvement in the chronification of pain has a decisive role in the intensity and course of the disease. The ICD has therefore been amended accordingly so that both somatic (physical) and psychological forms of chronic pain syndrome are listed. In the various sub-items it is even specified in more detail whether the mental illness came first and then the physical illness or vice versa.
Only through these exact distinctions is it possible to standardize medical diagnostics and therapy on an international level.
Classification according to Gerbershagen
With the Gerbershagen classification, the chronification of pain can be categorized more precisely. The division includes five different axes, each of which is divided into three stages. Stage 1 shows the best prognosis, while stage 3 is given to the most severe pain disorders.
The first axis describes the temporal course of the pain conditions.In doing so, attention is paid to whether pain always occurs or only temporarily and whether the intensity of the pain changes or whether the pain is continuously the same. If the pain is particularly severe, it is referred to as stage 3. If the pain occurs only intermittently and is weak in intensity, this is referred to as stage 1.
The second axis deals with the localization of the pain. If the patient can clearly assign the pain to a body region, then he is in stage 1. In the case of diffuse, non-localizable pain all over the body, the patient is designated stage 3.
Thirdly, the consumption behavior of pain medication is dealt with. Above all, attention is paid to whether there is an overdose or medication abuse. If this is the case over a longer period of time, it is referred to as stage 3. With proper and pain-related self-medication, the patient is classified in stage 1.
The fourth axis describes the extent to which a patient needs medical help. Particular attention is paid to whether he regularly visits a doctor (often the family doctor) as needed, or, mostly out of desperation, visits many different medical facilities at short intervals. In the first case this corresponds to stage 1 according to Gerbershagen, in the second to stage 3.
The fifth and last axis deals with the patient's social environment. If this is stable or only marginally burdened by problems, this is stage 1. If the family structure has broken up and the patient is not integrated into professional life and society, this speaks for stage 3.
In summary, the classification of the chronification of pain according to Gebershagen offers a multidimensional classification system from which both the symptoms and the patient's handling of the disease can be read. However, it should be ensured that the boundaries between the stages are often fluid and that a division is therefore not always precise.
Pension for chronic pain syndrome
If the patient is no longer able to work due to the chronic pain, even with extensive therapy, the following types of pension can be applied for. On the one hand, a disability pension can be a possibility. This is called “full” if the patient can only work three hours or less per day and classified as “partial” if a working time of three to six hours is possible.
The disability pension is limited to a certain period and must be extended again after it has expired.
If an application for a disability pension is submitted, some medical examinations must be carried out and it must be certified that the pain could not be improved by rehabilitation measures.
On the other hand, if you have severe disabilities due to chronic pain, you can apply for an old-age pension for severely disabled people. This means that the normal old-age pension can be applied for earlier. To do this, however, a severe disability must first be certified.
Degree of disability (GdB) in chronic pain syndrome
The GdB (degree of disability) is a standardized measured variable for quantifying the degree of disability in physically or mentally ill people.
In most cases, the GdB is determined by the pension office. The GdB is measured on a scale from 0 to 100, with 0 or hardly any restrictions and 100 a severe disability.
Generally speaking, from a value of 50, one speaks of a severely disabled person. The GdB is usually based on the underlying disease and the resulting functional restrictions.
There are many different types of disabilities in relation to chronic pain syndrome. If the symptoms of the underlying disease are not particularly severe and the resulting pain hardly leads to restrictions in daily life, the patient does not achieve a value higher than 20. If, on the other hand, the underlying disease is severe, for example cancer, and the patient is no longer able to do so to provide for independently, he is often classified as severely disabled.
The GdB therefore plays an important role in awarding social benefits and is a non-binding measure of the severity of an illness.
therapy
The goal of therapy should be to combat the root cause of chronic pain. Since this is often difficult, the therapy should lead to an increase in the quality of life of the patient and not only focus on reducing the pain intensity.
It is also the task of the attending physician to recognize psychological changes such as depressive moods or sleep disorders early on and to treat them.
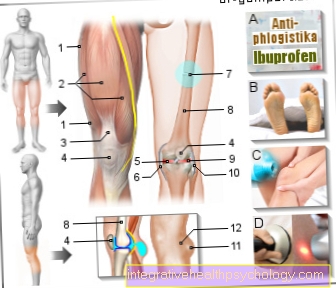
The choice of pain medication depends on whether the pain is nociceptive, i.e. originating from the tissue, or neuropathic, originating from the nerves. If you have nociceptive pain, you can give pain relievers such as ibuprofen and, if necessary, opioids.
Neuropathic pain can be treated with anticonvulsants such as gabapentin or pregabalin (Lyrica).
If psychosomatic factors play a role in chronic pain syndrome, drug therapy alone is not enough to optimally treat the pain.
Psychosocial therapy in the form of behavioral therapy or attention-guiding therapy to support medication is recommended here.
In general, the treatment of chronic pain syndrome should always consist of a combination of medicinal and non-medicinal measures, if possible.
You might also be interested in this topic: Conduction anesthesia
Therapy after an accident
Accidents are an important triggering factor in chronic pain syndrome. Protracted pain from injuries or incorrect processing of the pain can lead to changes in the body that are not fully understood and with the consequences of chronic pain syndrome.
It is therefore important not only to treat the physical damage after a traumatic accident, but also to give the patient the opportunity to process what they have experienced. If this does not happen, accidents are also associated with post-traumatic stress disorders.
This can lead to impaired processing of the pain and trauma and the pain persists even after all physical injuries have healed. Typical of post-traumatic stress disorder are deep feelings of loss of control, despair, and helplessness.
forecast
In the case of chronic pain syndrome, the protective function that pain has in healthy people takes a back seat and chronic pain becomes its own clinical picture.
The definition of chronic pain syndrome is pain that lasts for three to twelve months and shows no signs of a time limit. Therefore, the prognosis for a complete cure of this disease is poor, especially since there is no therapy that can specifically treat the cause of the pain.










.jpg)