The aorta
Synonyms in a broader sense
artery, main artery, artery, body artery
Medical: Thoracic aorta, abdominal aorta
English: aorta
definition
The aorta is the largest blood vessel in the body and is also called the main artery.
It is divided into four sections. With a total length of around 35 - 40 cm, it has a diameter of 3 - 3.5 cm. It arises from the left heart.

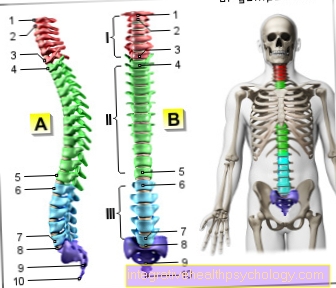
Classification and sections
The aorta above the diaphragm supplies the organs in the chest and is divided into three sections:
- ascending section (ascending aorta or pars ascendens aortae)
- Aortic arch (Arcus aortae)
- descending section = Pars thoracica descendens aortae
Below the diaphragm, the section is called the abdominal aorta or, more precisely, the descending part of the aorta. It gives off numerous branches to supply the abdominal organs.
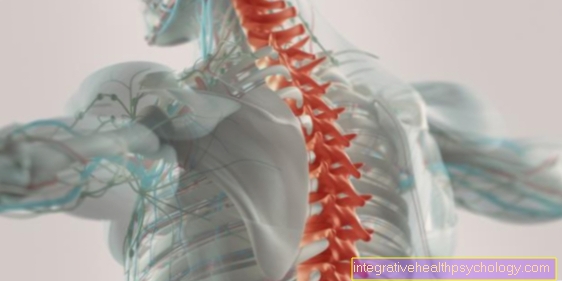
Illustration of the aorta

- Ascending aorta -
Pars ascendens aortae - Aortic arch - Arcus aortae
- Thoracic aorta
(descending aorta) -
Thoracic aorta - Aortic slit of the diaphragm -
Aortic hiatus - Abdominal aorta
(descending aorta) -
Abdominal aorta - Aortic fork - Aortic bifurcation
- Trunk of the liver, spleen and ma
gene arteries - Celiac trunk - Upper arm artery -
Brachial artery - Common pelvic artery -
Common iliac artery - External head artery -
External carotid artery - Cervical artery (common head artery) -
Common carotid artery - Clavicle artery -
Subclavian artery - Axillary artery - Axillary artery
- Diaphragm - Diaphragm
- Renal artery - Renal artery
- Radial artery - Radial artery
- Ulnar artery - Ulnar artery
You can find an overview of all Dr-Gumpert images at: medical illustrations
Anatomy (macroscopy) and departures
Ascending aorta
The aorta arises from the left heart just behind the aortic valve. Most of it runs upwards in the pericardium. This ascending section is called the ascending aorta.
It is about 5 - 6 cm long. The aorta also gives off its first two branches directly behind the heart valve (aortic valve). These are the left and right coronary arteries (also called coronary arteries) for supplying the heart muscle (arteria coronaria sinistra and arteria coronaria dextra).
These two branches lead to a swelling of the aortic origin (bulb aortae). The ascending section extends to the first large vascular outlet, the Truncus brachiocephalicus.
At the point where the ascending aorta begins, there is another small section - the aortic root. It is only a few centimeters long and plays an important role in maintaining a continuous blood flow.
If you'd like to learn more about it, check out our next topic below: Aortic Root - Anatomy, Function & Diseases
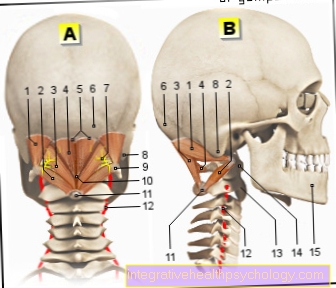
Aortic arch
Then it curves backwards, left and down.
This aortic arch is also known as the aortic arc. It extends over the left main bronchus at the level of the 4th thoracic vertebra. Large vessels arise from the aortic arch to supply the head, neck and arms.
The brachiocephalic trunk arises first and supplies the right side. The arteria thyroidea ima contributes to the blood supply to the thyroid gland.
The next two branches are the left common carotid artery, which supplies blood to the head and neck on the left side (= left carotid artery), and the left subclavian artery, which continues as the left subclavian artery to the left arm.
You may also be interested in this topic: Arteries of the Neck
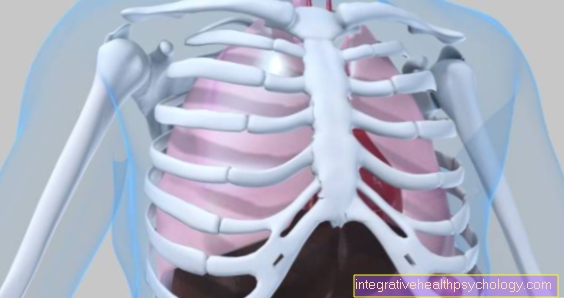
Descending aorta into the rib cage

After the aortic arch, the main artery is called the descending aorta above the diaphragm and the abdominalis below the diaphragm.
The numerous branches supply the space between the ribs as intercostal arteries (11 arteriae intercostales posteriores and one arteria subcostalis); Mediastinum (a space that is behind the breastbone and contains the chest organs without the lungs).
Before the aorta passes through the diaphragm at the level of the 12th thoracic vertebra, it gives off two upper branches on the right and left side to supply the diaphragm (arteria phrenica superior, left and dexter)
Descending aorta into the abdomen
after the aorta by the diaphragm has entered, it immediately gives off two branches to the side to supply the lower diaphragm (arteria phrenica inferior sinister and dexter).
Now follows as a large branch from the front Celiac trunk. This large-caliber vessel soon divides into three sections for supplying blood to the spleen (Splenic artery), the liver (Arteria hepatica communis) and des Stomach (Left gastric artery).
The next organs will be the Adrenal glands supplied with blood (arteria suprarenalis medialis sinistra and dextra).
The superior mesenteric artery, which arises forward, divides into several branches and supplies the Small intestine and large proportions of the Colon.
The paired renal vessels (arteria renalis sinster and dexter) go off above the unpaired arteria mesenterica inferior, which supplies the rest of the large intestine. Before the aorta joins the iliac arteries (arteria iliaca communis dexter and sinister) at the level of the 4. Lumbar vertebra divided, a total of four paired, laterally emerging vessels carry blood to the lumbar region.
Function of the aorta
The heart pumps blood intermittently into the main artery. This pulsatile blood flow has to be converted into a continuous flow to supply the body.
While the aorta v. a. close to the heart due to the high proportion of elastic fibers in the fine tissue when the blood is expelled from the heart (systole), it temporarily saves half of the ejection volume through the stretching.
Subsequently (in the diastole, i.e. the relaxation of the heart muscle), the vessel expands and the other half of the ejection fraction is replenished. In this way, the blood flow is even and the organs are protected from damage by the continuous supply. This function is also called the wind chamber function. Certain diseases of the blood vessels can cause the elasticity to decrease and organs to be damaged by high blood pressure or insufficient blood flow.
Diagnostics for diseases of the aorta
The aorta can be examined in the following ways:
- Ultrasound / sonography
- TEA (Transesophageal ultrasound = ultrasound over the esophagus)
- X-rays
- Computed Tomography
- Angiography / cardiac catheter
- MRI
Ultrasound of the aorta
A transducer emits waves that are reflected in different ways.
The return of the waves is registered. Depending on the strength of the reflection, this can be shown on a screen in a darkened room and the images can be printed out.
The aorta can be easily visualized on ultrasound.
TEA
TEE is a special type of ultrasound. A tube with a transducer is inserted through the mouth and into the esophagus of the fasted patient.
Since the heart and parts of the main artery are in close anatomical relation to the esophagus, these organs can be viewed using this transesophageal echocardiography.
Diseases like:
- Thrombosis
- Aneurysms (vascular wall sacs)
- Initial detachments (dissection)
or - Rupture of the aorta (ruptures)
can thus be diagnosed.
X-ray of the aorta
An X-ray of the entire chest can give an overview of the size, location and course of the aorta.
Computed Tomography
An expanded form of the X-ray is the Computed tomography (CT). A large number of X-ray images are created in a tube, which are then added to a three-dimensional image under computer control.
Aortic angiography
With X-rays and the use of a contrast agent, blood vessels can be visualized and assessed in an angiography.
With a cardiac catheter, a probe is pushed through an artery, usually the inguinal artery (arteria femoralis), back to the heart against the direction of flow, and blood flow to the heart, cardiac function and aorta are tested with contrast medium.
Magnetic resonance imaging (MRI)
Depending on the question, the Magnetic resonance imaging (MRI) can be used. Here you can too without using a contrast agent the vessels are depicted. This is helpful if you have a known allergy to contrast media. Turn into a tube Sectional images, but made without the use of X-rays.
Histology and Tissue (microscopy)
There are three histological layers:
1. Intima: The intima forms the innermost layer of the aorta and consists of the endothelium and a subendothelial layer.
On a basal lamina there are so-called endothelial cells in a unicellular layer, which have a negative charge at the tip (apical) due to a glycocalyx (sugar connected to the cell membrane).
These cells are flat and their long axis is parallel to the blood stream. The individual cells are connected by dense membrane protein connections (e.g. tight junctions, gap junctions, desmosomes). This seals the space between the cells, regulates paracellular transport (cells can escape from the blood system without damaging the cell wall!) And ensures the polarity of the cells.
The endothelium forms a barrier in the aorta through which the exchange of substances with the tissue takes place. It also plays an important role in blood clotting and inflammatory reactions (adherence of blood platelets and white blood cells), as well as in the regulation of the vessel size.
The subendothelial layer of the aorta consists of the extracellular matrix. This includes e.g. collagen and elastic fibers, collagen (type IV), microfibrils, fibrillin, proteoglycans, etc. This layer is the scene of vascular calcifications (atherosclerosis).
Read more on the topic: Atherosclerosis
2. Media (tunica media): In addition to elastic and collagen fibers, this middle layer mainly consists of (smooth) muscle cells that are arranged in a spiral or ring shape and regulate the size of the vessels.
3. Adventitia (Tunica externa): This outermost layer of the aorta consists mainly of connective tissue and anchors the vessel in the environment. However, it also contains blood vessels (vasa vasorum) and nerve vessels.
Between the intima and the media as well as between the media and the adventitia there is another membrane elasticinternals and externa). It is an elastic lamella.
The aorta is one of the elastic-type arteries. In this type of vessel, the media is particularly thick and contains many elastic fibers, which is important for the function of the aorta.
Diseases of the aorta
Aortic stenosis
Aortic valve stenosis is the almost complete closure of the aortic valve.
The stenosis can be caused by a congenital malformation, arteriosclerosis, rheumatic inflammation or endocarditis (inflammation of the inner lining of the heart) caused by a bacterial infection. The stenosis puts pressure on the left ventricle. The blood in the chamber can only be ejected against a higher pressure, as the heart valve can no longer fully open.
To compensate for this, there is muscle hypertrophy (the heart muscle becomes larger) in the left ventricle, which has further consequences, such as a higher heart rate due to a higher oxygen requirement for the increased muscle mass.
Symptoms are absent for a long time, symptoms such as tiredness, dizziness or arrhythmia appear late. Aortic valve stenosis is treated with a pressure gradient of over 50mmHg between the left ventricle and the ascending aorta or in symptomatic patients.
Read more here: Diseases of the aorta
Aortic regurgitation
Aortic valve insufficiency is the inability of the aortic valve to close.
This can be caused by an increase in the connective tissue of the valve (fibrosis) and the associated shrinkage of the valve, as can often be the case with rheumatic inflammation. This dilatation (expansion) can be caused by an increased volume of blood in the left ventricle, whereby the heart initially reacts with an increase in stroke volume and a dilatation of the ventricle (chamber) and later also with an increase in muscle mass.
This increase in volume loading is defined and described by the Frank-Starling mechanism. The aortic valve insufficiency is treated by an operation if the patient shows impaired resilience with known insufficiency, the insufficiency is severe or the volume in the left ventricle is significantly increased.
You may also be interested in this topic: Valvular heart disease
Aortic tear
An aortic rupture is caused by increased mechanical stress from the blood flow and a previously damaged wall.
Depending on which wall layer tears, the lumen may be relocated, as in aortic dissection, or free bleeding. This can result in a covered rupture, whereby the escape of blood from the aorta is stopped by the peritoneum and blood can seep in for a few days.
Patients with a ruptured aorta experience sudden devastating pain in the back and / or abdomen, often accompanied by symptoms of shock with a drop in blood pressure or fear of death, as well as subjective shortness of breath or blood-depleted lower extremities. If a tear in the aorta remains undetected and it is not a covered tear, death occurs within a few minutes. A covered rupture is also an emergency indication and must be operated on immediately if it is discovered in good time.
You may also be interested in this topic: Calcifications in the abdominal artery
Aortic aneurysm
An aortic aneurysm is a localized widening of the aorta.
A real aneurysm (verum aneurysm), whereby all wall layers are affected, is differentiated from a false aneurysm. In the case of the false aneurysm, only the outermost layer of the wall, the adventitia, is affected. False aneurysms can take various forms, such as sac-shaped (sacciformis) or spindle-shaped (fusiformis).
An aneurysm results from the weakening of the elastic force of the media (middle wall layer of the vessel), which means that the vessel can no longer withstand the intravascular pressure and "bulges".
The causes for the development of a widening of the aorta are manifold. For example, arterial hypertension (high blood pressure), arteriosclerosis or a congenital weakness of the connective tissue (e.g. Marfan syndrome) can be responsible. Symptoms such as pain in the back, feeling of pressure or subjectively perceived shortness of breath can occur, but are not specific to an aortic aneurysm. An imaging procedure such as computed tomography (CT) or magnetic resonance imaging (MRI) can be considered for diagnostic clarification.
An indication for an operation is the critical diameter of 5 cm for the ascending aorta and the aortic arch or 6 cm for the descending aorta. However, an operation should also be considered if the aneurysm grows more than 1 cm in 3 months. A stent is often implanted in the descending aorta during the operation, provided that no further branching artery is obstructed during the operation.
Read more about this: Symptoms of an aortic aneurysm
Aortic dissection
Aortic dissection is the splitting of the wall layers of the main artery. The starting point for the division of the wall layers is the tunica intima, the innermost layer of the aorta, where the blood is in direct contact. There is bleeding between the tunica intima and the media, which is the subsequent wall layer.
The bleeding causes the lumen to shift, so that a “true lumen” and a “false lumen” are created. Lumen refers to the cavity in a vessel. The tearing of the intima and the creation of the “false lumen” can displace the true lumen. The entry is the tear point in the intima of the aorta, the reentry is the point at which the blood from the false lumen returns to the true lumen.
The aortic dissection can be divided according to the Stanford and DeBakey classification. Both classifications describe the location of the dissection.
Typical symptoms of an aortic dissection are stabbing pain radiating into the shoulder and / or so-called annihilation pain, in which one can also feel fear of death. The dissection is treated similarly to the aneurysm by means of an operation through a tube prosthesis or stent.
Read more on this topic: Aortic dissection
What is an aortic prosthesis?
Just as there are prostheses for joints or entire extremities, there are also prostheses for the aorta that allow normal blood circulation. The vascular or tube prosthesis is usually made of plastic, such as polyethylene terephthalate, and is inserted into the damaged part of the aorta during an operation. First of all, the damaged part of the artery is removed and then the prosthesis is implanted and sutured in place with an overlap.
A heart-lung machine is connected to maintain the blood circulation during the operation. Depending on which area of the aorta is damaged, the connection of the heart-lung machine and the actual insertion of the prosthesis can be problematic. One example is the prosthesis in the aortic arch, from which the vessels to the brain and the upper extremities, among other things, branch off.
Since the brain has to be continuously supplied with oxygen, we deal with the phenomenon of hypothermia, in which the body is cooled down to a cool number by means of the heart-lung machine in order to reduce the maximum oxygen requirement by more than three times.This gives the surgeons a certain amount of time to insert the prosthesis into the aortic arch without causing massive damage to the brain.
Read more on this topic: Aortic prosthesis
Lymph nodes on the aorta
There are numerous lymph nodes on the aorta and especially on the vascular branches of the aorta.
A filtration of the lymph from the abdominal organs takes place in the lymph nodes. In a certain way, the lymph nodes on the aorta represent a collection point for the lymph of the individual organs, because the lymph drains in a specific sequence for each individual organ.
How long is the aorta?
The length of the aorta is usually 35-40cm, with the actual total length varying from person to person.
In general, the ascending aorta has a length of 5-6 cm and the total descending aorta is about 25-30 cm.
What is the normal diameter of an aorta?
The normal diameter of the aorta in adults is between 2.5-3.5 cm.
In the course of life, however, the diameter can also increase. This is due to the loss of elasticity in the connective tissue, which is also noticeable as normal skin folds. However, the diameter can also decrease due to degenerative processes such as calcification of the vessels (arterosclerosis).















.jpg)







-mit-ten-(titanic-elastic-nail)-oder-sten.jpg)
