Local anesthesia at the dentist
introduction
The local anesthesia creates a local anesthetic in the area of the nerve endings in the mouth. This results in a local elimination of pain and elimination of sensitivity without impairing the patient's consciousness.
After a while, the body breaks down the local anesthetic and the effects begin to wear off. In addition to a local anesthetic, a so-called vasoconstrictor such as adrenaline is often given. adrenaline makes the vessels narrowso that it takes longer for the local anesthetic to be removed in the blood. This will prolong the effect of the local anesthetic.

History of local anesthesia
The ophthalmologist Carl Koller accidentally discovered its narcotic effects through the use of cocaine in 1884 after discovering that it was cocaine numbed his tongue. After realizing this, the surgeon took advantage of William Stewart Halstet In 1885 cocaine for the first time for local anesthesia in dentistry. This is how surface, conduction and infiltration anesthesia ultimately developed.
1905 was the first time Adrenaline to prolong anesthesia from Heinrich Braun used. In the years that followed, local anesthetics, such as the widely used lidocaine and procaine, became increasingly successful.
indication
The indication depends on the one hand on the type of intervention and on the other hand on the patient's wishes. Different forms of anesthesia are selected depending on the procedure.
General anesthesia is often necessary for major operations in the oral cavity.
Find out more about the topic here: General anesthesia at the dentist
Often anesthesia is also caused by an anxiety disorder of the patient before dental interventions (Dentophobia).
You might also be interested in: Fear of the dentist
Classification of local anesthesia in dentistry
Surface anesthesia
Surface anesthesia is used to eliminate pain in the oral mucosa, e.g. as part of pain reduction when injecting the subsequent local anesthetic or during superficial interventions in the area of the gums. The sensitive nerve endings are supplied by diffusion and thus anesthetized. For surface anesthesia are mainly Atricain, Lidocaine and Tetracaine utilized. It is used as a gel, ointment or spray. The anesthetic is often applied to a cotton swab and placed on the future injection point for about a minute. Similar successes as with surface anesthesia can be achieved with pressure anesthesia. A finger pressure is exerted on the area to be injected for about 15 seconds, making the subsequent injection more painless.
Infiltration anesthesia
Infiltration anesthesia is only used for interventions in the upper jaw, as the bone tissue is less dense and therefore permeable to the anesthetic. In contrast to the lower jaw, the bone of which is more pronounced. Therefore, a central anesthesia is usually performed here. The local anesthetic is used in infiltration anesthesia under the mucous membrane (submucosal) and over the periosteum (supraperiostal) so that it can spread over the periosteum in the bone. The local anesthesia begins to show its first effects after just one to three minutes, with the maximum effect only occurring after about 20 minutes. In the time window of maximum strength, the anesthesia is sufficient to e.g. to pull a tooth.
Conduction anesthesia
In conduction anesthesia, the blockade of a nerve pathway is used, which numbs all areas that are supplied by this nerve pathway. This form of anesthesia is mainly used for major operations in the area of the lower jaw. The bones in the lower jaw are stronger, so that conduction anesthesia works better than infiltration anesthesia. The anesthetic is near the Inferior alveolar nerve in the area of Mandible foramen (Entry point into the jaw). Unlike infiltration anesthesia, not only the corresponding tooth is anesthetized, but also the entire subsequent supply area of the nerve. This leads to a long-lasting numbness of the lower jaw, the involved mucous membranes and the lower lip.
Intraligamentary anesthesia
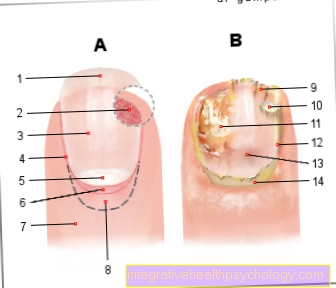
In the course of intraligamenous anesthesia, only the affected tooth is anesthetized. The injection takes place in the so-called Gingival sulcus. The sulcus gingivae is a recess running circularly around the tooth between the neck of the tooth and the gums. It is suitable for the upper and lower jaw, but with restrictions for the lower and posterior region, as the teeth are more powerful there. This form of anesthesia is called "intraligamentary"Because a mini-cannula is inserted into the periodontal gap, into the ligaments (lat. “ligamentum) of the teeth holding apparatus is introduced and the local anesthetic is injected there. The anesthetic penetrates the tooth supporting apparatus including the bony structures up to the tip of the tooth root and unfolds its effect within a few seconds. The duration of action corresponds to about 20 to 30 minutes, anesthetic can be injected to prolong the effect. For intraligamentary anesthesia, only a small amount of the anesthetic is required per lane, so this form of anesthesia is particularly suitable for patients with cardiovascular problems.
Aftermath of anesthesia
After the anesthesia, the sensation in the treated area only returns after a while.After that, you should initially refrain from eating and drinking. The duration of the waiver depends on the type of procedure and the anesthesia. This serves as a prophylactic protection against swallowing food residues and liquids.
How long does the local anesthesia last?
How long a local anesthetic lasts after a dental procedure is always very different and depends on the individual metabolism of the patient and on the type of local anesthetic used, its dosage and possible additives.
On average, it is pain-free between 30 minutes and an hour on. However, the subjective deafness persists much longer. A duration of action of up to 5 hours can be assumed here, although this again varies greatly from person to person.
The location of the anesthetic also influences the duration of the effect. For example, an anesthetic is involved Bupivacaine (Trade name Carbostesin®) in the upper jaw up to five hours and in the lower jaw up to eight hours. This is partly due to the bone structure: the upper jaw has a lower bone density, which is why the anesthetic can be removed more quickly than in the more compact lower jaw.
Additions like Phentolamine mesilate can shorten the duration of action of local anesthetics and the associated numbness. Like local anesthesia, they are injected into the same spot and take effect there.
When can I smoke again after having a local anesthetic?
Basically, it is advisable not to smoke for as long as possible after a dental procedure, as smoking severely affects wound healing and promotes wound healing disorders and severe infections.
Otherwise, a similar rule applies to smoking as to eating and drinking after a local anesthetic. As soon as the anesthesia has completely subsided, you can smoke againwithout the risk of swallowing or injury from the anesthetic. However, since the duration of the local anesthetic effect is very individual, it is not possible to give an exact guideline time for smoking.
Side effects of local anesthesia
In most cases, local anesthetics are well tolerated so that no side effects occur. If side effects occur, they are mostly caused by the addition of adrenaline.
Absolute contraindications for the administration of adrenaline are:
- an untreated glaucoma (Angle-closure glaucoma)
- a high frequency absolute arrhythmia
- nd taking tricyclic antidepressants
If too much of the anesthetic is used, it can cause too much Malaise, restlessness, dizziness, palpitations one metallic taste and deafness in the mouth up to Seizures come.
Furthermore, the patient can be allergic to the local anesthetic.
As a complication, it can get through the syringe Nerve damage come mainly of Lingual nerve and Inferior alveolar nervesome of which are permanent. Vascular and mucosal damage can occur. Rarely does an infection occur.
Read more on the topic: Side effects of local anesthesia
Which active ingredients are used?
Various active ingredients are approved for local anesthesia during dental treatments. Their exact composition can vary depending on the provider. For more detailed information, you should always talk to the attending physician. The most common active ingredients include:
- Lidocaine
- Prilocaine
- Articain
- Mepivacaine
- Procaine
In order to extend the duration of action, additions such as Epinephrine or Norepinehprin (also adrenaline) used. These cause the vessels to contract so that the active ingredient is not transported away as quickly, but acts longer at its desired location. It also reduces the tendency to bleed.
Read also: Local anesthetics - the local anesthetic
Duration of effect
The duration of local anesthesia can vary widely. It depends on the type of active ingredient, the amount administered and the concentration of the adrenaline additive. The higher the adrenaline concentration and the more anesthetic is administered, the longer the anesthesia will last.
The type of application also has an effect on the duration. Circuit anesthesia, in which the right or left half of the lower jaw is completely anesthetized, lasts longer than infiltration anesthesia or intraligamentary anesthesia, in which only individual teeth are anesthetized. The anesthesia usually subsides completely after 3-5 hours. As long as the oral cavity is still numb, you should avoid eating and hot drinks to avoid injury.
Is local anesthesia at the dentist possible during pregnancy / breastfeeding?
In principle, treatment with local anesthesia at the dentist is possible both during pregnancy and while breastfeeding. However, the indication for the need for treatment should be made strictly, since despite the good tolerability of local anesthetics, every intervention is associated with risks.
If there is an urgent need for treatment, the pregnancy or breastfeeding period should be discussed in advance with the attending physician so that the appropriate local anesthetic can be chosen and, if necessary, a dose reduction can be made. The possible waiver of certain additives such as adrenaline in the local anesthetic mixtures should also be discussed in advance in the event of an existing pregnancy. Become common Articain and Bupivacaine used.
The TENS
In the transcutaneous electrical nerve stimulation (TENS) one uses Stimulation current, which can relieve pain after treatment / illness and analgesia (Elimination of pain) is reached during interventions. The stimulation current releases pain-suppressing messenger substances (Neurotransmitters and Endorphins) increased distributed. In addition, vasodilator substances are increasingly produced so that the transmission of pain is inhibited.
A TENS machine is used for this method. It consists of a generator and two electrodes. For treatment, the electrodes are positioned in the mouth and outside the mouth. Before the treatment, the dentist adjusts the pulse strength and frequency as well as the current strength. However, should the pain change, the patient can change the parameters independently.