The nerve inflammation on the face
definition
Nerve inflammation in the face is defined as the inflammation of one or more nerves that supply certain areas of the face. In medical terminology, such an inflammation is called neuritis. If only a single nerve is affected, this is known as mononeuritis. If several nerves are inflamed, there is polyneuritis.
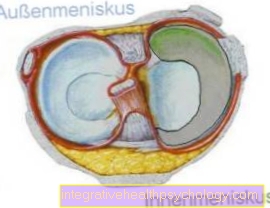
In the face, the trigeminal nerve, the trigeminal nerve, and the facial nerve, the facial nerve, are particularly affected by inflammatory processes.
The trigeminal nerve plays a major role in the sensory and motor supply of the head and face. It has three large main branches, of which one or two and rarely all three branches can be inflamed. A distinction is made between the branches of the eyes, the upper jaw and the lower jaw. In medical terminology, they are called the ophthalmic nerve, the maxillary nerve and the mandibular nerve.
The facial nerve has several secondary branches and its fibers have different qualities and functions. Depending on which nerve and nerve branch are affected, this can lead to various failure symptoms and complaints.

The reasons
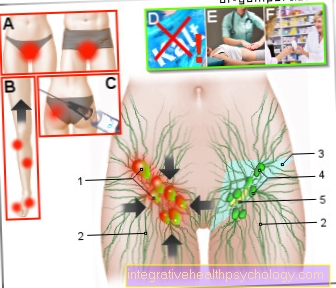
The causes of nerve inflammation in the face can be many. It is often triggered by an infection. Varicella zoster viruses are often responsible for nerve inflammation. This means that reactivation of the chickenpox virus in the form of shingles can provoke neuritis in the face. But other viruses or bacteria can also cause such nerve inflammation.
Inflammation can also be caused by surgery on the face. For example, surgery on the parotid gland can lead to nerve damage and inflammation. During the operation, the facial nerve can become irritated, inflamed, and damaged
In addition, inflammation of the nerves on the face can have a toxic cause. This means that neuritis can result from various chemicals or alcohol. In addition, long-term malnutrition can affect the facial nerves and cause inflammation. A deficiency in the B vitamins plays a particularly important role.
Furthermore, derailments and dysregulations of the metabolism can lead to nerve inflammation. For example, in the context of diabetes mellitus, kidney disorders or gout, inflammatory processes of nerves can occur. In addition, allergic reactions can lead to what is known as neuroallergic neuritis on the face.
The cause of classic trigeminal neuralgia is often unknown. The technical jargon speaks of idiopathic trigeminal neuralgia. The causal pathomechanism has been partially researched. It is postulated that classic trigeminal neuralgia is related to a "vascular-nerve conflict". The nerve branches are compressed by a degenerative change in the blood vessel. A permanent "vascular-nerve conflict" can isolate the N.trigeminal nerve. This can lead to direct contact between sensitive fibers and pain fibers. As a result, the typical pain attacks of trigeminal neuralgia can be triggered.
Find out more about the topic here: Shingles.
The trigeminal nerve as the cause
Classic trigeminal neuralgia is characterized by a lightning-like shooting, extremely burning and electrifying pain in the area that is supplied by one or more trigeminal nerve branches. The type of pain is described in medical terminology as neuropathic pain.
The pain attacks that occur in the context of trigeminal neuralgia can be triggered spontaneously or by certain triggers. These triggers can be, for example, chewing, speaking, swallowing, brushing your teeth, shaving, washing, facial movements, touching or a draft of cold air. Initially, the pain attacks set in spontaneously and later they are provoked by triggers.
Many of those affected suffer very badly and often the quality of life is limited. Understandably, this can lead to mood changes. Unfortunately, these depressive moods and the resulting reactive fears are misinterpreted as the “cause” for the disease.
Find out more about the topic here: Trigeminal neuralgia.
The draft as the cause
In the course of trigeminal neuralgia, external stimuli can trigger the pain attacks. One possible trigger is draft. This is emotionally very stressful for those affected, as it is difficult for them to predict the triggering of the attacks. Accordingly, this can be controlled or avoided to a lesser extent.
The consequence may be that those affected no longer leave their apartment or house. This can have further consequences for social and productive life.
The teeth as the cause
The upper and lower jaw branches of the triple nerve can also become inflamed. The nerve branch of the lower jaw is called the ramus mandibularis. The maxillary nerve branch, on the other hand, is referred to as the maxillary ramus. When this is inflamed, pain can spread to the teeth of the upper jaw, upper lip, roof of the mouth, nasal lining, and nostril.
If the nerve branch of the lower jaw is affected, the teeth in the lower jaw, tongue and lower lip are often painful.
An involuntary, reflexive clenching of the jaw can occur during an attack of pain. The complaints are often mistakenly interpreted as a dental problem. But the characteristic pain attacks of nerve inflammation facilitate differential diagnosis.
Less often, damage and / or inflammation of the lingual nerve (branch of the mandibular ramus) occurs when a wisdom tooth is removed. Immediately after the procedure, the affected person feels an immense blow in the tongue with immediate numbness. The complaints rarely remain permanent. Treatment is similar to that for trigeminal neuralgia.
Find out more about the topic here: Numbness.
Stress as a cause
As a rule, stress is not the only cause of nerve inflammation in the face. But psychological and physical stress can promote and intensify the triggering of symptoms.
This is due to the body's own processes that take place during stress reactions. As part of this, various substances and hormones are released. They serve as messenger substances. This means that they carry certain “messages” and thus enable the cells to communicate with one another. Among other things, this leads to changes in various vessels. This can ultimately increase the "vascular-nerve conflict" and affect the symptoms of nerve inflammation in the face
The consequences of stress? Find out more about this here.
The symptoms
Nerve inflammation in the face can be recognized by various symptoms. Both with classic trigeminal neuralgia and with other facial neuralgia, severe pain in certain areas of the face or in the entire face is in the foreground. The accompanying symptoms, the character and the localization of the pain can be differentiated in the various nerve inflammations in the face.
In classic trigeminal neuralgia, an extremely strong, electrifying pain in the face that shoots in like lightning occurs spontaneously or through irritation. The pain attack lasts only a few seconds. It is extremely rare for it to last beyond minutes.
In the midst of a pain attack, the facial muscles in the supply area of the affected nerve branch can involuntarily twitch. Experts describe this twitch as a clonic-tonic muscle movement. After the attack of pain, the area in question can no longer be excited for seconds or minutes. This means that immediately after a pain attack, no further attack can be triggered.
In symptomatic trigeminal neuralgia, the same attack-like attacks of pain occur as in classic trigeminal neuralgia. But in the symptomatic form, there is often no freedom from pain between attacks. In addition, the symptomatic form leads to a weakened reflex in the eyes (so-called corneal reflex), as well as paralysis and sensory disorders.
Atypical facial pain is characterized by its non-seizure, dull, boring pain in the supply area of the trigeminal nerve. The pain often lasts most of the day and is particularly severe in one eye, nose or cheek.
Later on, an atypical facial pain can spread to the entire face, hairy head and neck. It is also typical that with this form there are no trigger points and no loss of sensitivity.
Glossopharyngeal neuralgia can be recognized by a mostly attack-like pain in the base of the tongue, in the area of the tonsils or in the middle ear with radiating pain in the throat. In addition, uncontrolled watering of the eyes, coughing, taste disorders, hoarseness, swallowing and speaking difficulties, restricted tongue mobility, and dry mouth and throat area can occur. In addition, about 10% can lead to a drop in blood pressure, cardiovascular problems and temporary fainting and unconsciousness.
In addition, ophthalmic zoster can develop as part of a herpes infection. This means that nerve inflammation in the face occurs, which manifests itself in the eye area and is triggered by herpes viruses. This type of nerve inflammation is characterized by atypical facial pain, sensory disturbances and visible cold sores.
Find out all about the topic here: Symptoms of an inflammation of the nerves.
Facial paralysis as a symptom
With nerve inflammation in the face, temporary paralysis of the facial muscles can occur. The prerequisite is that motor facial nerve fibers are excessively irritated or damaged. Symptomatic trigeminal neuralgia can accordingly trigger temporary or long-term facial paralysis.
There are several diseases that can cause this. These include certain forms of migraines, certain types of cancer that are localized in the face, metastases from other primary tumors, a tumor of the cerebellopontine angle, circulatory disorders, multiple sclerosis and a few other diseases.
Any facial paralysis should always be clarified by a doctor. The best way for a neurologist to determine what the causes are and whether the facial paralysis is temporary or permanent. This or another doctor can also initiate appropriate drug and non-drug treatment in the form of occupational, physical and / or speech therapy.
The pain as a symptom
The pain of nerve inflammation in the face is often very pronounced. Some sufferers speak of a crushing pain.
Depending on the cause of the nerve inflammation and its form, the pain expresses itself in an attack-like or non-attack-like manner with corresponding accompanying symptoms.
Find out more about the topic here: Facial pain.
The diagnosis
The first priority in diagnosis is to ask about symptoms and to analyze pain attacks precisely. A neurological examination is also carried out. The functions, reactions and sensitivity of the facial nerves and facial muscles are tested. Touching certain trigger zones on the face or applying pressure to the exit points of the nerve branches of the trigeminal nerve can trigger a violent pain attack. Knowing about it must be handled carefully - also in diagnostics.
Magnetic resonance imaging (MRI) can also be used to detect compression of the nerve by a vessel. In some cases, performing a nerve ultrasound can be useful.
The treatment
Nerve inflammation in the face is treated differently depending on the cause, severity, individual factors and underlying disease.
The basis of the treatment is that possible causative substances, such as alcohol, are avoided. In addition, underlying diseases and disorders must be remedied. Accordingly, diabetes mellitus must be properly adjusted. If there is a vitamin or mineral deficiency, these must be substituted. If a virus is causally responsible, antivirals are used. Antibiotics can be effective for bacterial infection. In addition, pain relievers and anti-inflammatory drugs may be necessary.
As a rule, conservative treatment is attempted first. There are various drugs available that can be used for this.
First, monotherapy is attempted. This means that only one drug is used. If this procedure is not successful, different drugs are combined with one another. The dose is chosen and increased until it is as pain-free as possible - taking into account that the side effects remain tolerable. Often it takes a doctor's sensitivity to adjust the dose correctly. If no symptoms can be achieved over 4-6 weeks, the dose can be reduced gradually.
When conservative treatment options are exhausted, certain surgical interventions may be indicated. There are various surgical methods that can be effective. These methods are roughly divided into microvascular decompression (Jannetta operation), transcutaneous therapies and radiosurgical treatments. The choice of surgical method depends on the general surgical risk and the individual circumstances.
In addition to drug therapy and sometimes postoperatively, acupuncture, physiotherapy, occupational therapy and speech therapy can have a supportive effect. In some cases, those affected find the use of a TENS device helpful. With the help of electricity, specific nerve branches are stimulated and stimulated in a targeted manner.
These drugs can help
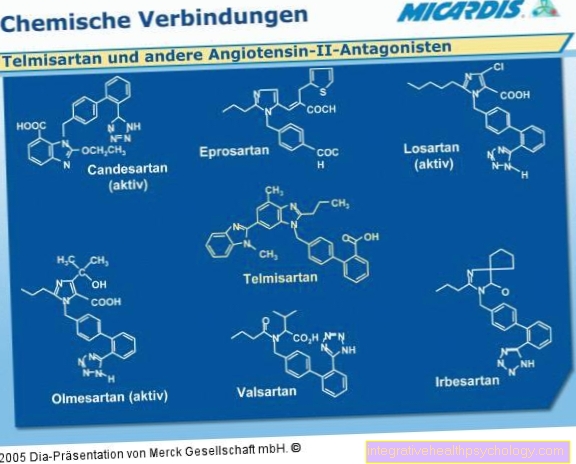
The drugs that can help with nerve inflammation in the face are constantly being developed. In trigeminal neuralgia, carbamazepine is often the drug of choice. Oxacarbazepine can also be used.
In acute therapy, phenytoin is often administered intravenously. Alternatively, pimozide is sometimes used. Furthermore, phenytoin, baclofen, lamotrigine and gabapentin can also be used for long-term therapy. If trigeminal neuralgia occurs as part of multiple sclerosis, misoprostol may be advisable for therapy.
Glossopharyngeal neuralgia is acutely treated with a drug that has an anesthetic effect, such as xylocaine spray or 1% novocaine. Long-term drug treatment is similar to that for trigeminal neuralgia.
Atypical facial pain is often treated with a tricyclic antidepressant, most often amitriptyline. In these cases, amitriptyline is used not because of depression, but because of its pain-relieving effect. Alternatively, drugs similar to those used to treat trigeminal neuralgia can be used.
These home remedies can help
In some cases, home remedies can be supportive. Some authors recommend camphor oil for this. One should leave 50 grams of camphor oil together with 15 peeled and crushed cloves of garlic at room temperature for 8 days. Then strain and squeeze out. The liquid can then be used to rub the painful areas on the face.
In addition, some affected people use St. John's wort oil - both for local application and in the form of tea for internal use. It is important to find out about possible side effects of St. John's wort oil beforehand.
An individual blend of clove, basil, eucalyptus and olive oils can also help. Another alternative is to fill a linen bag with hay flowers or a cherry stone pillow and heat it up. Then the linen bag can be placed on the painful area. The temperature should not be too hot and burns should be avoided. In addition, lavender sachets can also have a soothing effect.
Find out more about the topic here: Medicinal plants.
Homeopathy as a possible treatment
Homeopathic remedies can have a supportive effect in combination with other measures. The choice of remedies depends on the symptoms and individual factors. In addition, in the case of nerve inflammation in the face, it can be selected depending on the exact location, cause and characteristics of the pain.
For example, China rubra C15, Cinnabaris C15, Spigelia C4, Mezereum C7, Hypericum C9 or C15, Chamomilla C15, Magnesia phosphorica or Arsenicum album C4 are used. If possible, homeopathic treatment should be discussed with a doctor.
Warmth or cold - that helps better
In the case of highly acute inflammatory processes, heat treatment can be contraindicated, as this can worsen the symptoms. Otherwise, heat can often have a soothing effect.
There are various recommendations for certain home remedies for facial nerve inflammation. Cold can be a trigger and trigger pain attacks and should therefore be avoided. The cold causes the vessels to contract and can have a negative effect on the nerve branches. In addition, a kind of rebound phenomenon can occur after exposure to the cold. This means that the pain and discomfort can become even more pronounced. Therefore, strong cold influence on the facial skin and drafts should be avoided if possible. It is recommended to protect the skin of the face with creams and ointments that contain goat butter or high-dose vitamin E.
The duration of the illness
The duration of a nerve inflammation in the face depends on the cause, the immune system and individual conditions. If the cause can be adequately eliminated, the nerve inflammation can also be reduced under favorable circumstances.
If the cause cannot be treated or the conditions are unfavorable, facial nerve inflammation can persist in certain cases.
The length of the sick leave
Sick leave depends on many different factors. The cause, the extent of the inflammation and / or the underlying disease, as well as the workplace and the activities to be carried out are decisive. The extent to which the person concerned behaves in a restricted manner also plays an important role.
Prognosis
It is not possible to make a general prognosis for nerve inflammation. The prognosis depends on a variety of components, so it would be negligent to make general statements.
The only thing that is fundamentally given is that the prognosis is usually better if the cause is known and there are options for treatment. If the cause is unknown, the prognosis is often worse.