Pudendal neuralgia
What is pudendal neuralgia?
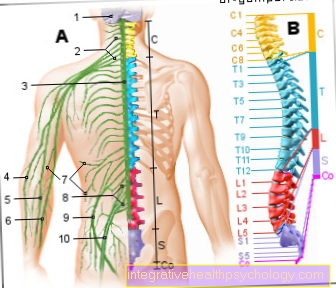
Pudendal neuralgia is a painful irritation of the pudendal nerve, which presents itself as pain in the area between the genital and anus (perineal region). Pain can radiate to the front and back and be accompanied by other symptoms such as urinary or stool continence or disorders of sexual function. It is also typical that the pain becomes stronger when sitting and decreases significantly when lying down. The condition is relatively rare and affects women twice as often as men.

causes
The causes of pudendal neuralgia are manifold. In most cases, it is mechanical compression of the nerve that causes irritation and thus pain. This is the case, for example, with cyclists who experience a permanent constriction of the pudendal nerve over longer distances.
But even with a change in the surrounding tissue, such as vascular diseases and damage to the connective tissue, pinching can occur.
It is not uncommon for pudendal neuralgia to occur as a result of operations in the pelvic area. On the one hand, there is the risk of direct damage to the nerve by the surgeon and, on the other hand, the risk of mechanical irritation due to excessive pulling on the leg, as is often carried out in fracture operations.
In addition to these mechanical causes, there are a number of other diseases that can lead to the clinical picture of neuralgia of the pudendal nerve.
These include above all diabetes mellitus and so-called shingles.
Read more on the subject below: Diabetes Mellitus and Shingles
diagnosis
The diagnosis of pudendal neuralgia is secured through the use of several imaging and electrophysiological procedures in addition to a detailed survey of the medical history.
In electrophysiology, where, among other things, the nerve conduction velocity can be measured, this is usually shown to be longer. Imaging procedures such as X-rays or an MRI are primarily used to search for possible causes and to rule out other differential diagnoses, since pudendal neuralgia itself is rarely associated with structural changes that can be detected in the imaging.
Thus, the diagnosis of pudendal neuralgia is largely guided by the clinical picture of the symptoms that are usually specific for this disease.
Which doctor treats pudendal neuralgia?
If you suspect pudendal neuralgia, you should always first see a family doctor, as this can rule out simpler differential diagnoses such as hemorrhoids.
In most cases, a referral is made to the proctologist, who can conduct a more detailed examination and basically carry out the treatment of this neuralgia. The diagnostics described above, such as imaging procedures and others, are usually initiated by the proctologist.
It is not uncommon for the opinion of a neurologist to be consulted in the treatment of the disease, as they specialize in the treatment of nerve pain (neuralgia). The diagnosis and treatment of pudendal neuralgia therefore requires the interdisciplinary participation of various disciplines.
Read more on the topic under: Hemorrhoids
What are the symptoms of pudendal neuralgia?
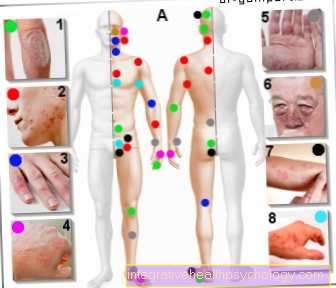
The leading symptom of pudendal neuralgia is severe nerve pain (neuralgia).
These are often described as stabbing, stinging, and inclusive. While the focus of the pain is in the area between the genitalia and anus, the pain often radiates further into the area of the external vagina or penis.
In most cases, the symptoms are unilateral. Involvement of both sides is usually only described after severe pelvic fractures or other major trauma. All patients describe that the pain increases significantly when sitting, while it almost completely disappears when lying down.
Sleep complaints are therefore usually not given. Often, patients also report an improvement after a bowel movement, which can be attributed to a pressure relief of the small pelvis. In addition to the pain, other symptoms can occur. These include urinary and fecal incontinence, which, however, rarely occurs.
Sensitivity disorders in the sense of paresthesia in the perineal area are described somewhat more frequently. In rare cases, sexual dysfunction can also occur.
Read more on the subject under: Incontinence
Treatment and therapy
Drug treatment of pudendal neuralgia, like most nerve pain, is complicated because it does not respond to conventional pain relievers such as ibuprofen or ASA. Therefore, drugs that are normally used as antidepressants or anti-epileptic drugs are mainly used. The antidepressant most commonly used in this context is amitryptyline.
Antiepileptic drugs or anticonvulsants that are used are:
- Carbamazepine,
- Gabapentin,
- Lamotrigine
- Pregabalin
A combination of active ingredients of these two substance classes is possible and often shows a good effect. However, complete freedom from symptoms can only rarely be achieved.
In addition to drug therapy, treatment through surgical interventions has established itself.
These always aim to decompress the nerve and show response rates of over 70%. In most cases, however, the effects of the interventions only become apparent within the following months. Another therapeutic option is canular infiltration. With this, a mixture of cortisone and long-term local anesthetics is injected onto the compression site of the pudendal nerve. While this therapy shows a good effect up to complete freedom from pain in almost all patients, this effect is only limited to a few weeks.
Thus, drug therapy or surgical decompression of the nerve continue to be the leading options in the long-term treatment of pudendal neuralgia.
Read more on the subject at: Amitriptyline
Can you operate on that too?
As described above, surgery is a possible treatment option in the presence of pudendal neuralgia.
The aim of the procedure is to decompress the nerve, i.e. to remove structures that pinch the nerve in its course.
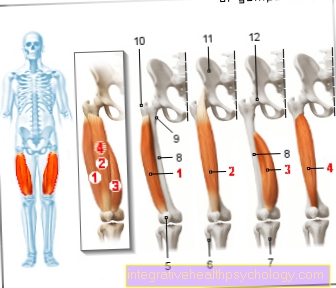
The surgical access is usually via the muscles of the buttocks (gluteal muscles).
The nerve is often relocated to the small pelvis and disorders of the ligament structures that can cause the nerve to become trapped are eliminated.
Since the pain often increases after the pudendal nerve has been freed, it is usually numbed with local anesthetics at the end of the operation.
In most cases, the pain-relieving effect of the procedure only shows up after a few weeks to months.
homeopathy
There are numerous homeopathic remedies that promise to relieve or cure the pain of pudendal neuralgia. Which remedy is used depends largely on the triggering cause of the nerve pain.
For example, if this is due to an injury or trauma, taking Arnica is recommended.
But the quality of the pain is also taken into account when deciding on the appropriate remedy. When the pain is described as pressing, throbbing, Belladona is often prescribed, while Bryonia is used for sharp pain.
Duration
The duration of pudendal neuralgia can vary significantly. While it is not uncommon for the symptoms to subside spontaneously, which is more common in patients without an identifiable cause, the symptoms can last for several years in other patients.
This is especially the case when the nerve is permanently compressed by surrounding structures. In these cases, a good drug setting is essential and a surgical procedure should be considered.
In the case of short-term irritation of the nerve during an operation or other mechanical loads, the symptoms usually subside within a few months.
Is there a cure?
The prognosis of pudendal neuralgia is generally considered to be good, provided that all available therapy options are included in the treatment regimen. If a pinching cause of the nerve can be identified, surgical treatment makes sense in many cases and can lead to complete healing in the long term.
Nevertheless, there are patients who do not benefit from surgery and who also have poor drug therapy. In this respect, the prognosis of pudendal neuralgia depends largely on the underlying cause and can usually only be assessed in the course of the disease.