Influences on my individual breast cancer risk
Does breast cancer even affect me?
Breast cancer (breast cancer) is the most common female cancer, accounting for well over a quarter of all cases. According to the German Robert Koch Institute, 27.8% of all women will develop breast cancer in their lifetime. Every half hour in Germany a woman dies of this disease.
The peak age for women with breast cancer is between 60 and 65 years. In the age group of women between 35 and 60 years, breast cancer (breast cancer) is the main cause of death. This is why early and comprehensive preventive care is of great importance.

In general, the rate of new illnesses (cases of illness that are newly diagnosed within a certain period of time) in Germany has risen steadily since 1980 - by 15% in the last 10 years - while the death rate has fallen slightly since the mid-1990s. The increasing number of new cases is partly due to the improved possibilities for breast cancer detection. With better diagnostics, the disease can often be detected at an earlier stage. This, together with the great advances made in the therapeutic area, has a positive effect on the survival rate.
Please also visit our website Causes of Breast Cancer
It is important to know that a general distinction is made between the incidence of cancer, i.e. the number of new cases and the mortality rate, i.e. the number of people who actually die from their cancer and not from another disease. For comparison you can use the Prostate cancer draw the man. It is the most common cancer in men, i.e. it has a high incidence, but far fewer men die from this type of cancer; prostate cancer only ranks third in terms of mortality.
Breast cancer, on the other hand, is not only the most common cancer in women, it is also the disease with the highest mortality rate. The prognosis of the course of the disease depends largely on the stage at which the breast cancer is diagnosed. The earlier the disease is diagnosed, the better the chances of recovery.
Incidentally, men can get breast cancer too, albeit in a very small percentage. This cancer is so rare in men that international experts do not agree on the exact number: about half a percent and one percent of all breast cancer diagnoses are made in male patients, these are the approximate figures for industrialized countries. In the treatment approaches, no significant differences are made between male and female patients.
Why does breast cancer develop and when should you be extra careful?
Nobody can say exactly when and why the disease breaks out in some women. In contrast to other diseases, it is not yet sufficiently clear which factors ultimately lead to the development of breast cancer. However, there are certain risk factors that statistically increase the likelihood of getting sick. The problem with probabilities is that they don't provide solid information about which women will get sick and which will stay healthy. Many women who develop breast cancer do not belong to any of the different risk groups. Likewise, many women who have multiple risk factors never develop breast cancer. Nevertheless, one should be more careful when several risk factors coincide and regularly follow the recommended ones Checkups go.
Read more on the subject here Breast cancer screening and Breast cancer detect.
What role does age play in breast cancer risk?
Age is the most important risk factor! The risk of breast cancer in older women is increasing. In most cases, breast cancer is a postmenopausal woman's disease. This is attributed to errors in cell division, which become more likely with age. This creates errors in the genetic material (DNA) of the cells. They can lead to cells e.g. becoming immortal or growing uncontrollably. Cancer can develop from these cells if our immune system does not recognize them and fight them quickly enough.
How do hormones affect breast cancer risk?
The female sex hormones are called estrogen and progesterone (progestin). These hormones not only affect a woman's cycle, but also breast development and thus have an impact on the development of breast cancer. Like other healthy cells, tumor cells can have so-called receptors, which are proteins on the surface of the cell that act like receiving stations for hormones. By binding the hormones to the receptor, the cell receives e.g. the signal to grow and share.
Women who have had their first menstrual period before the age of 12 and / or who enter the menopause late have an increased risk of developing breast cancer. These women produce the female sex hormones over a longer period of time, because before the first menstrual period and after the onset of menopause, the estrogen levels in the body are very low. With the number of menstrual (regular) cycles from the first period (menarche) to the onset of menopause, the duration of the estrogen effect on the tissue increases and thus the risk of developing breast cancer.
Pregnancies also have an influence on the risk of breast cancer through the hormonal balance. Childless women have an increased risk of developing the disease, just like women who had their first child at an old age.
In contrast, breastfeeding seems to have a protective effect on the risk of breast cancer.
There are two possible explanations for this: Before the birth of the first child, the cells in the breast that are supposed to form the surface of the mammary glands are relatively indefinite. They only finally mature for their actual task when they receive a signal from the body. The signals are triggered by the birth of a child and amplified by breastfeeding, the body then recruits the mammary gland cells that it needs. Mature cells are less prone to damage to their genome and are therefore less likely to mutate into cancer cells. In addition, breastfeeding postpones the point at which the woman's cycle resumes after pregnancy.
However, estrogen and progesterone have no proven carcinogenic effect. Carcinogens are substances that are believed to cause cancer. A well-known example of a carcinogen that has been shown to cause cancer in humans is asbestos. For estrogen and progesterone, only a growth-promoting, not a triggering effect for tumor development has been assumed so far.
Breast cancer risk with estrogen ingestion
Estrogen is considered one of the most important risk factors for breast cancer. Many women naturally live with elevated estrogen levels, but artificial estrogen is also often used therapeutically for various diseases. Some contraceptive pills may also contain estrogen, increasing the risk of breast cancer. Therapeutic estrogen is often used, especially during menopause. It primarily counteracts the common osteoporosis in menopause. High estrogen levels can also occur as metabolic products in overweight patients. Regular smoking also influences the estrogen level and is therefore an important risk factor for breast cancer.
Breast cancer risk and the "birth control pill"
The “pill” is one of the most frequently prescribed drugs in Germany. Birth control drugs called contraceptives contain estrogen and / or progesterone, the female sex hormones. Therefore, the question arose early on whether taking the “pill” promotes the development of breast cancer. An army of scientific studies is concerned with this question, some of which come to contradicting results. The European Society for Reproductive Medicine (ESHRE Capri Workgroup) has drawn the following conclusions from the various data and research results:
The use of oral contraceptives leads to a small temporary increase in breast cancer risk by about a factor of 1.07-1.24. And that for about as long as the medication is being taken, after which the risk drops back to normal values, regardless of the total duration of use. Since contraceptives are typically used at an age when breast cancer is rare, such an increase in risk would have little effect on the overall incidence of the disease.
Does breastfeeding affect the risk of breast cancer?
Various studies have shown that breastfeeding children reduces the risk of breast cancer. Breast-feeding seems to have protective properties, especially in familial breast cancer accumulations. One reason for this may be that breastfeeding releases hormones in the body that reduce breast growth. When breastfeeding, among other things, the hormones "prolactin" and "oxytocin" are released. The exact mechanisms behind these two hormones in the development of breast tumors are not known. Nevertheless, they initially seem to have a positive influence on the breast tissue through the release during breastfeeding.
Info: pill
The risk of ovarian and uterusbodycancer (not uterusneckcancer) is even lower after taking the pill for many years.
Postmenopausal hormones
Another point is taking female hormones for relief from Menopausal symptoms. In order to clarify the question of the advantages and risks associated with the administration of estrogens and progesterone, one of the largest and most expensive studies on hormone replacement therapy was started in America in 2002. The results of this study of the "Women's Health Initiative" (WHI) made big waves and are still controversial today. Actually, the study was supposed to show whether estrogens were a preventative measure Heart attacks and osteoporosis act and protect against chronic diseases.
However, the doctors involved stopped the study prematurely. In the study of more than 16,000 women aged 50 and over who took hormone therapy, there was an increased incidence of breast cancer, heart attacks and Strokes compared with the placebo group. According to the evaluation of the study, hormone therapy after menopause increased the risk of breast cancer by about 1.5 times after about 10 years of hormone use. After the results were published, there was a drastic drop in prescriptions for estrogen preparations in Germany as well.
The WHI study is still hotly debated today. Critics cite methodological weaknesses of the study, they criticize e.g. that the examined women z. Some previous illnesses had not been considered during the treatment, the age range of 50-79 years was chosen too wide and the administration of the hormones was not adjusted to the body weight.
It should also be noted that the risk of breast cancer only increases after an intake of more than five years, a period that e.g. when taking hormone preparations for the relief of menopausal symptoms is / should not be exceeded.
Overall, today's recommendations point towards an individual risk-benefit assessment. If there is a medical reason for use, you can Estrogen preparations can be used sensibly. Nevertheless, a short and low dose prescription should be aimed for. There are also differences between estrogen-only supplements, which have a lower risk, and Mixed preparations out estrogen and progesterone.
What role do genes play?
While the majority of breast cancer cases occur without a recognizable family background, 5-10% of all breast cancer cases can be traced back to a genetic predisposition. You can have your own risk determined through a simple genetic test.
Many genes protect us from normal body cells turning into cancer cells. These genes control the growth of cells and ensure that a cell stops growing when it comes into contact with other cells on its surface. If one or more of these protective genes fail, the risk increases that this cell will develop into a viable “cancer cell”. The cells then grow, although they are completely surrounded by other cells, displace them and spread in healthy tissue; their growth is then called invasive.
BRCA-1 and -2 are such protective genes, they play an important role in repairing damage in the genetic material. BRCA stands for Breast Cancer Gene. If BRCA-1 and -2 fail, cancer does not result directly, but because the damage that occurs in the genome of breast cells can no longer be repaired, the likelihood that this damage will turn a cell into a cancer cell increases. In the case of the BRCA gene, it is a two-step process: First, the supervisory authority fails and then external factors lead to damage in the genome that can no longer be absorbed. Women with a defective BRCA-1 or 2 gene are at high risk of developing breast cancer during their lifetime.
Read more about the topic here: Is Breast Cancer Hereditary?
Breast cancer cases with a genetic cause are characterized by the fact that the disease usually occurs at an early age (called: early onset), affects several family members and often both breasts are affected. The lower the age of onset of those affected or the greater the number of sick people in a family, the more likely there is a genetic cause and the higher the risk of breast cancer for close relatives. In addition, male members of these families have a significantly higher risk of developing prostate cancer.
The likelihood of developing breast cancer is increased compared to a man without damage to one of the breast cancer genes. Compared to the risk of the female family members, however, very low, since only very small amounts of female hormones are produced in the male body and have an effect on the breast tissue. The disease follows an autosomal dominant inheritance. Autosomal means that the damaged BRCA-1 or 2 variant is not on the two sex chromosomes X or Y, but on another of our 46 chromosomes.
Chromosomes consist of DNA and thus contain the genetic material of the cell. If a disease is inherited in an autosomal manner, this means above all that both sexes can get the disease. Dominant means that a defective gene is sufficient to increase the risk of the disease.
This is best understood by looking at the opposite, recessive inheritance. All genes in a cell exist in duplicate, with recessive inheritance the second gene can catch the defect in the other gene, so both genes must be broken for the disease to break out fully. With the dominant inheritance, it is sufficient if one of the two genes is broken. At least that is the general theory. However, as is often the case, real life is a bit more complicated and there are exceptions to this rule. Carriers of a mutated BRCA-1 gene have an approx. 87% chance of developing breast cancer in their lifetime and an approx. 45% chance of ovarian cancer. A mutation in the BRCA 2 gene is rarer overall and less likely to lead to the development of ovarian cancer. In addition to BRCA-1 and -2, there are mutations in other genes that increase the risk of developing breast cancer. But they are each very rare in and of themselves.
If a genetic burden is diagnosed, it is possible to perform prophylactic (i.e. preventive) surgery on the breasts, namely a mastectomy. At the same time, a prophylactic removal of the ovaries can be useful, but the problem here is that with the removal, the estrogen production drops rapidly and the women enter the menopause virtually surgically.
Are you more interested in this topic? Then read our next article on this at: BRCA Mutation - Symptoms, Causes & Therapy
Info: genes
If you suspect that there is a genetic strain in the family, see your gynecologist. If necessary, he can refer you for genetic counseling.
What does lifestyle have to do with breast cancer risk?
In the past, a relationship between diet and disease risk has been established for many different types of cancer. A high-fat diet is e.g. a relevant factor in cancers such as esophageal cancer, gastric cancer and colon cancer.
For breast cancer, too, it has been shown that diet has an influence on the risk of disease. It plays an important role here because it influences the body's own hormone production. Obesity in childhood and adolescence presumably favors the development of breast cancer, but the study situation is not yet sufficient and there are contradicting results.
In addition to body weight, measured as BMI (= body mass index), it is crucial how the fat is distributed in the body. The BMI is calculated from the body weight [kg] divided by the square of the body height [m2]. The formula is:
BMI = body weight: (height in m) 2.
The unit of the BMI is therefore kg / m2. In women, depending on age, there is an increased risk with a BMI of approx. 28 kg / m2. A more masculine fat distribution, in which the waist circumference is increased (also called apple shape), is unfavorable. On the other hand, a more feminine fat distribution, in which the hip circumference is increased (also called pear shape), is more favorable. This is measured in what is known as the hip-waist ratio, i.e. the ratio of the hip circumference divided by the waist circumference; a low hip-waist ratio is therefore less favorable.
You can find more under our topic Body Mass Index.
Excessive consumption of high-calorie foods with little physical activity can lead to high body weight and high body fat percentage. This in turn causes the body to start producing estrogen too early and the first menstrual period starts early. The earlier the first period starts, the more years a woman has with cyclical hormone production and the higher the number of menstrual cycles, the higher the risk of breast cancer, but only for breast cancer that occurs after menopause has occurred.
Other underlying mechanisms are also being discussed: Scientists suspect that the fatty tissue itself also releases hormones that promote the growth of cancer cells. In the adipose tissue itself, estrogen is produced, albeit to a lesser extent than in the ovaries.
Exercise and exercise are likely to lower the risk of breast cancer. Physical activity improves the energy balance - calorie consumption in relation to calorie intake - and thus reduces the risk of various diseases.
Can soy reduce the risk of breast cancer?
The effects of soy on breast cancer risk and breast cancer treatment are controversial. While naturopathic practices often emphasize the beneficial effects of soy on health and the immune system, caution should be exercised when dealing with breast cancer. Many doctors even consider soy to be harmful, as it releases so-called "phytoestrogens" which, in theory, can even promote breast cancer or counteract the treatment of breast cancer. Both theories cannot be proven. Overall, there is only a very small, insignificant difference due to the consumption of soy. Nevertheless, caution should apply at least during hormonal treatment of an existing breast cancer.
Breast cancer risk and alcohol
Excessive alcohol consumption increases the risk of breast cancer to some extent, which is likely due to an increase in the level of estrogen in the blood. If folic acid deficiency occurs at the same time (vegetable malnutrition such as too few types of cabbage, soy, tomatoes, green vegetables, etc.), this increases the negative influence of alcohol, because folic acid is important for the stability of the DNA.
Breast Cancer Risk and Radiation
Ionizing radiation (e.g. radioactive radiation or X-rays) can generally lead to cancer of radiation-sensitive tissue. In Germany, ionizing radiation usually only occurs in connection with medical examinations. Since the mammary gland tissue is one of the most radiation-sensitive tissues in the body, radiation (x-ray examinations of the cervical and thoracic spine, the esophagus, the gastrointestinal tract (see stomach, small intestine, large intestine), the kidneys, computed tomography and nuclear medicine examinations) should be carried out as far as how possible to avoid. An increase in the risk of breast cancer due to ionizing radiation was observed in particular before and during puberty and before a first pregnancy to term. With increasing age, the sensitivity of the breast (female breast) to radiation decreases.
Do other diseases affect breast cancer risk?
Other breast diseases can in principle also increase the risk of breast cancer, e.g. Mastopathies. However, these diseases can also make diagnosis more difficult and thus increase the risk of "not discovering" the disease.
What role does the immune system play?
The body's own immune defense is a much discussed topic and the subject of intensive research in connection with all types of cancer. The complex interplay of different cells and messenger substances is still a mystery today and will probably do so for a long time to come. Cells in our immune system are actually able to recognize and eliminate cancer cells under certain circumstances. However, cancer is not a failure of the immune system.
The basic task of the body's immune system is to protect us from cells and organisms that are foreign to the body. Bacteria, viruses and fungi that make us sick are repelled to ensure survival. That sounds easier than it is at first. The individual parts of our body's own defenses must not only recognize what is foreign, but also be able to distinguish what is our own. And tumor cells are never as foreign as bacteria, viruses or fungi: they usually only differ from healthy cells in the slight changes in the genetic make-up; the devil is in the details here. In addition, cancer cells can camouflage themselves from the immune system.
For a better understanding one can imagine a pair of scales: on the one hand there are diseases against which our immune system can no longer defend itself: an example of this is an HIV disease (AIDS). If left untreated, a person dies from it in a short time and not from the virus itself, but from many different infections with bacteria, fungi and viruses that our body fends off with ease.
On the other hand, there are diseases in which our immune system can defend itself too well, in which it even begins to defend itself against its own body: Examples are autoimmune diseases such as multiple sclerosis, in which nerve cells are attacked by the immune system. That is the range on which the responsiveness of our body's own defenses moves, both sides of the scale must be precisely balanced, the scale must not deflect too much either to one side or the other.
Of course, this picture is very simplistic and incomplete, but it helps to understand why a simple increase in immune response does not necessarily lead to increased health. Cancer researchers now know that the processes in the body's defenses are far too complex for a simple "immune boost" to have a demonstrable influence on an illness.
What are important risk factors?
Factor by which the relative risk increases
- Familial burden due to genetic factors (e.g. BRCA-1 or -2) (up to 20-fold)
- Age at the time of the first pregnancy over 30 years (approx. 3 times)
- Childlessness (approx. 1.5 to 2.5 times)
- Obesity (obesity) (approx. 2-fold)
- Excessive alcohol consumption (approx. 2 times)
- Mastopathies (approx. 2-fold)
- Early first menstrual period and later onset of menopause (approx. 1 to 2 times)
- Oral contraceptives (while taking) (approx. 1 to 1.5 times (but not yet fully understood))
- Hormone replacement therapy (approx. 1 to 1.5 times)
How does the risk of breast cancer relate to breast size?
According to the current status of the studies, the pure breast size has no influence on the risk of breast cancer. It is important, however, whether the breast contains pure fat tissue or whether it consists to a large extent of glandular tissue. Glandular tissue increases the risk of developing breast cancer. The amount of glandular tissue can also have an impact on the size of the breast. A large breast that is high in fat is in no way at risk. A breast that is large because of the amount of glandular tissue is more likely to be affected. The risk is not influenced by the size alone, but breast cancer detection is. Large breasts can be more difficult to examine in mammography, which is why the risk of overlook is minimally increased if the tumor is already present.
Can you calculate the risk of breast cancer?
The risk of breast cancer can be calculated. As a result of various long-term studies, it is now known which risk factors have a significant influence on the development of breast cancer. For example, studies have tested the occurrence of breast cancer in women with previous pregnancies, with high levels of estrogen, with previous family illnesses and many other factors, which revealed the likelihood of occurrence. It is important to note, however, that breast cancer risk is a probability that is statistically correct, but can never be transferred to the individual case. Even with an extremely high calculated risk, there is no need for illness. A gynecologist can use certain calculation options to determine your own risk. Factors that receive the most attention in the calculation are age, previous breast findings, familial breast cancer cases, hormone levels, the number of pregnancies and the presence of certain genes.
Is there a test to assess breast cancer risk?
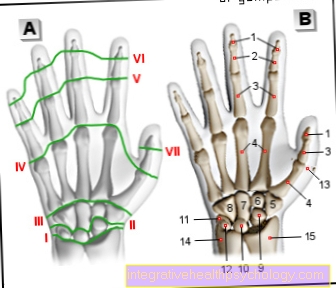
A woman can have all kinds of tests carried out by a gynecologist in order to better assess her own risk of breast cancer. The risk can be calculated in the best possible way with many known factors. However, in order to identify most of these factors, it is often necessary to perform gynecological diagnostics. An important test for the early detection of breast cancer is a mammogram, a chest x-ray. This makes it possible to identify the nature of the tissue, the size of the breast, changes that have already been made in the tissue and other preliminary stages or risk factors of breast cancer. Genetic tests can also be done. It is known that the "BRCA1" and "BRCA2" genes are associated with an increased risk of breast cancer. As an invasive measure, a breast biopsy can be carried out, in which the tissue can be precisely analyzed under the microscope, whereby any changes and preliminary stages can be identified.
Can I reduce the risk of breast cancer?
Some factors that influence the risk of breast cancer are linked to behavior and external influences. Important risk factors are related to hormone levels in the body. The pill as a contraceptive can adversely affect hormone levels. Although it is only a small factor, it increases the risk of breast cancer minimally. The hormone levels are also influenced by obesity, a high-fat and unhealthy diet, smoking and alcohol. All these factors together increase the risk of breast cancer by a certain percentage, which is why it is advisable to avoid them. However, a diet rich in fish and iodine has a positive influence.
How can you recognize breast cancer?
Signs of a tumor in the breast are often very early palpable lumps in the breast tissue that are not sensitive to pressure, are indistinct and hard.
Especially in older women, there is a high probability that lumps are a sign of breast cancer. In younger women, cysts - benign, fluid-filled growths - are often the cause of lumps.
Unusual discharge from the nipple, such as bloody and / or watery secretions, also speak for breast cancer.
Retraction in the skin, the inability to move the breast on the chest muscles or a retracted nipple can also indicate breast cancer.
Skin abnormalities such as "peau d'orange", an orange peel-like change in the skin or eczema on the chest are indications of advanced cancer.
In the so-called inflammatory carcinoma, the inflammatory breast cancer, the tumor is usually not sharply delineated, but is noticeable through reddening of the skin.
If breast cancer is suspected, you should see your doctor as soon as possible. They can make a diagnosis by palpating the breast and performing other diagnostic measures.
Read more on the topic: Detecting Breast Cancer




.jpg)