Heparin Induced Thrombocytopenia (HIT)
definition
A drop in the number of blood platelets caused by the administration of heparin is considered heparin-induced Thrombocytopenia (HIT). A distinction is made between two forms, the non-immunological (HIT type I) and the antibody-related form (HIT type II).
.jpg)
introduction
The word Thrombocytopenia denotes one Platelet deficiency, so Platelets. The word components "thrombos", "kytos" and "penia" come from the Greek and mean translated: lump, vessel / shell and lack.
Platelets play an important role in the Blood clotting, because they adhere to injured areas of the blood vessels and seal the injury by sticking them together. They also release substances that promote coagulation. Normally a person has between 150,000 and 450,000 platelets per microliter of blood. If there are fewer platelets, it is called thrombocytopenia.
A heparin-induced thrombocytopenia (abbreviated: HIT) is a rare but dreaded possible one side effect of the anticoagulant Heparin, in which the number of platelets decreases due to the heparin.
frequency
It is difficult to give precise information on the frequency. However, it can be assumed that everyone tenth patient, the one with Treated with heparin forms antibodies.
A Type II reaction joins about 3% on that with unfractionated heparin treated and only at 0,1% of patients with low molecular weight / fractionated heparin be treated.
Thus, heparin-induced thrombocytopenia of type II is 30 times less common in patients with fractionated heparin than in patients with unfractionated heparin. For this reason, patients should preferably be treated with fractionated heparin to avoid HIT II.
Forms of heparin-induced thrombocytopenia
Non-immunological HIT (Type I)
This form is the most common HIT with a early onset and one rather mild course. It affects about 1 -5% of the patients with unfractionated Heparin be treated.
In the nonimmunological early form of heparin-induced thrombocytopenia occurs no massive drop in platelets on, they decrease by a maximum of 30% of the initial value.
This is due to the effect of heparin on the blood platelets, because it activates the platelets directly. As a result, they release messenger substances that promote coagulation, which lead to the accumulation of further platelets. The platelet counts usually return to normal spontaneously after a few days, even if therapy with heparin is continued. Usually with this form of HIT no thrombosis and the number of platelets does not fall below 80,000 per microliter.
Patients with fractionated, low molecular weight instead of unfractionated Heparins treated show significantly less type I HIT.
Antibody-related HIT (Type II)
Of the second type the heparin-induced thrombocytopenia usually shows up a little later, but it can be life threatening run away. About 1% of patients who are infused with unfractionated heparins are affected.
If left untreated, 30% of patients die because of the consequences of heparin-induced thrombocytopenia of type II, with alternative anticoagulant drugs there are still a comparatively high number of patients with eight to twenty percent.
The type II is based on a Antibody formation against the complex formed in the body between heparin and the protein platelet factor 4. The symptoms appear in patients who are not yet sensitized between the fifth and twentieth Day after starting heparin. In the case of pre-existing sensitization, the antibodies from previous heparin therapy and the corresponding reaction are already present and type II heparin-induced thrombocytopenia manifests itself within a few hours.
Of the Low platelet count is much more serious than with heparin-induced thrombocytopenia of type I, because the drop is usually greater than 50% of the initial value and only less than 100,000 platelets per microliter remain.
When treated with fractionated heparins, HIT type II appears about 30 times less in contrast to unfractionated heparin.
causes
Heparin-induced thrombocytopenias arise either as non-immunological, harmless early form (type I) or based on the Formation of antibodies against the platelet factor 4 / heparin complex (type II). These lead to the clumping of the blood and the platelets are, so to speak, “trapped” or “caught”, they can no longer perform their natural function.
Unfractionated heparins have a higher risk triggering a HIT than, for example Clexane, a low molecular weight, fractionated heparin.
Symptoms
No symptoms usually occur in heparin-induced thrombocytopenia Type I. on, the drop in platelets spontaneously normalizes again. That is why this type usually happens in such a way that the person concerned does not even notice it.
Of the massive decrease in the number of platelets at a Type II heparin-induced thrombocytopenia often leads to pronounced symptoms the deficiency.
Skin necrosis may be noticed at the heparin injection site, the skin turns bluish-black. It is an expression of Cell death at this point.
Through the heparin-induced thrombocytopenia, the platelets are activated and clump together, it comes to Thrombosis (Clots) in the blood vessels. As a result, the tissue to be supplied can no longer be properly supplied with blood and nutrients from the blood and carries massive damage from that. If action is not taken in good time, it may be necessary to amputate the affected limb.
When the thrombosis can manifest itself in organs Strokes, Heart attacks or one Pulmonary embolism arise that are life-threatening.
The spectrum of symptoms shows how dangerous type II heparin-induced thrombocytopenia can be.
Diagnosis
A heparin-induced thrombocytopenia is proven especially in the Blood count. There you can Measure the platelet drop. A drop of more than 50 percent is alarming, the values usually drop below 100,000 platelets per microliter.
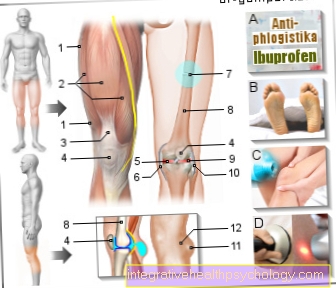
A more precise estimate of whether a type II HIT is present can be made with the help of the so-called 4 T scores to be hit.
Important parameters here are the vremaining number of platelets (Thrombocytopenia) the time elapsed between the start of heparin administration and the start of waste (Timing of the waste) how serious the Complications whether there is a thrombosis, necrosis of the injection site or other manifestations and whether there are any different reasons for thrombocytopenia.
Zero to two points are awarded. The higher the total number of points, the more likely the presence of heparin-induced type II thrombocytopenia.
New methods, the so-called ELISA or HIPA test, enable the Detection of antibodies. A positive test result with a simultaneous drop in platelets speaks for HIT, a negative test, however, rules it out. In Germany, the HIPA test (heparin-induced platelet activation assay) is mainly used.
therapy
The most important step in therapy is that immediate discontinuation of the heparin if a type II HIT is suspected.
Any other medication that contains heparin must also no longer be used to prevent possible complications. This also includes ointments containing heparin or catheter washes. The anticoagulant therapy must be on non-heparin based substances to treat the underlying disease and, above all, to avoid the circulatory disorders caused by HIT.
This is usually the means Argatroban (Argatra) used. The drug Danaparoid can also cause an allergic reaction due to its structural similarity to heparin. Before using it, it should therefore be clarified whether the antibodies that triggered the HIT also react with danaparoid.
If the HIT has already triggered serious thrombosis, fibrinolysis may be necessary. This means that the blood clots are dissolved using medication.
To prevent heparin-induced thrombocytopenia from occurring again, the heparin allergy should be avoided in the Patient ID card or Allergy pass and should not be left unmentioned in the case of new presentations at the hospital or the doctor.
Note
General information on drug thrombosis prophylaxis (heparins) can be found on the page on the topic: Drug thrombosis prophylaxis
Important!
If HIT type II is suspected, the heparin must be discontinued immediately.











.jpg)