Lacrimal drainage disorders

1. Inflammation of the lacrimal gland
Inflammation of the lacrimal gland as a variant of a disease of the lacrimal ducts (Dacryoadenitis) can be divided into the acute and the chronic form.
Symptoms:
On the affected side, swelling, redness and pain in the side of the eyebrow area are noticeable.
Causes:
A local infection that also affects the lacrimal gland is just as likely a cause of inflammation of the lacrimal gland as a systematic disease.
Therapy:
Therapy is often enough systemic antibiotics off, but sometimes a surgical opening the inflamed area may be necessary.
Complications:
A spread of the Inflammation in the eye socket area its possible, but rarely occurs.
2. Lacrimal gland tumors
Symptoms:
Lacrimal gland tumors as a disease of the lacrimal ducts are rare and often noticeable for the first time as a non-painful swelling in the lacrimal gland area (lateral eyebrow area).
Forecast:
The tumors in the area of the lacrimal gland can be benign or malignant. As they grow, they can displace the eyeball, disrupting eye mobility or causing damage to the optic nerve. Changes to the fundus can also occur (e.g. retinal folds, retinal haemorrhage, choroidal swelling).
Therapy:
Lacrimal gland tumors are surgically removed and then examined histologically. Depending on the histological findings, the next steps should then be planned.
Lacrimal drainage ducts
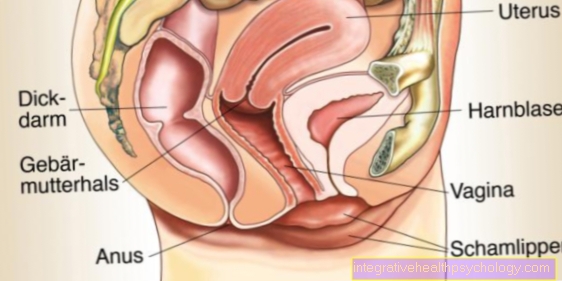
Tears flow in the area of the inner corner of the eyelid via the upper and lower teardrop point into the lacrimal tubules. These two small tear ducts of the upper and lower eyelids finally end in the lacrimal sac via a common tear duct. The lacrimal duct connects the tear sac and nose. The so-called Hasner valve is located in the area of the turbinate in front of the mouth of the lacrimal duct into the nose.
3. Inflammation of the lacrimal sac
synonym
Dacryocystitis [see extra article "Inflammation of the bags under the eyes]
4. Constrictions (stenoses) in the area of the draining tear ducts
root cause
Inflammation, scarring or, albeit rarely, a systemic disease can lead to a narrowing of the lacrimal points (puncta lacrimalia).
Therapy:
Dilation (widening) of the teardrop can often restore the drainage of tears.
More on this: Tear duct stenosis
Different surgical techniques for tear drainage disorders

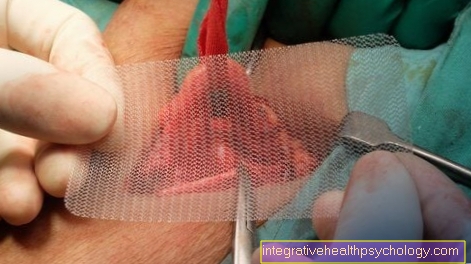
If there are drainage disorders as a disease of the lacrimal ducts in the area of the lacrimal tubules, the lacrimal sac or the lacrimal duct, a lacrimal duct surgery may be necessary.
There are various surgical techniques that can be used to restore the drainage of tears.
1. Dacryocystorhinostomy (according to Toti):
Especially with constrictions (Stenoses) in the area of the nasal passage, the dacryorhinostomy according to Toti shows very good results.
Procedure of the operation:
Blood thinning / anticoagulant drugs must be discontinued prior to surgery. The dacryocystorhinostomy is then performed under general anesthesia. It creates a new drainage path for tears into the nose. A silicone tube is inserted so that this path is kept open immediately after the operation. This can be removed after about 3 months, as the healing process is then completed to such an extent that there is little risk of adhesion.
If the hose slips prematurely or is lost, there is usually no acute risk to the result of the operation. Nevertheless, the patient should present himself to an ophthalmologist quickly. After the operation, there is a strict ban on blowing your nose to prevent loss or premature displacement of the tube.
2. Lester-Jones operation:
If the stenosis in the area of the lacrimal tubules (Canaliculus communis), a small tube is also required, which is implanted.
3. Probing the tear ducts:
The so-called Hasner valve sits at the end of the tear ducts in front of the mouth in the nasal cavity and closes it off. Usually it opens Hasner flap just before the child is born. If a newborn is opened too late, this can lead to tears in the child or recurrent inflammation.
In over 90% of these cases, the Hasner flap in the course of spontaneous up to the 1st year of life. By massages in the area of the tear sac, the drainage can be promoted and the opening of the Hasner flap get supported.
If there is no spontaneous opening of the Hasner flap shows, a probing of the tear duct is necessary.
The Hasner valve is opened mechanically by inserting a tear duct. After this minimally invasive operation, the local administration of decongestant and anti-inflammatory eye drops is necessary.