Gallbladder Cancer Diagnosis
Diagnosis
Due to the unspecific symptoms, gallbladder carcinoma is sometimes diagnosed by chance during a routine examination (e.g. sonography of the abdomen) of the abdomen. If a carcinoma of the biliary tract is suspected, the patient must first be questioned in detail (anamnesis). One has to look especially for the symptoms that speak for a biliary congestion. The patient should then be given a thorough physical examination. The first thing that often occurs is a yellowing of the skin (Jaundice) and in some cases a painless, bulging gallbladder in the right upper abdomen can be felt (Courvoisier's symbol).
In advanced cases, the actual tumor can even be felt.
When analyzing the blood (laboratory) certain blood values can indicate a disease of the biliary tract. For example, the Gamma glutamyl transferase (Gamma-GT), the Alkaline phosphatase (AP) and the Billiruby increased, suggesting bile build-up but not specific to gallbladder cancer. These blood parameters can also be increased in the case of other biliary tract obstacles, such as a gallstone (cholecystolithiasis).
So-called Tumor markers are substances in the blood that are often found in some types of cancer and can thus indicate a cancer. They do not play an essential role in the initial diagnosis of gallbladder carcinoma, as it is not uncommon for false-positive results to be obtained. However, if you find a certain tumor marker value increased before the operation, which disappears after the operation, then this marker can be used particularly well to prevent a new outbreak of the tumor (Tumor recurrence) diagnose with a quick blood test. Tumor markers that can be increased in gallbladder cancer are: CA 72-4, CA 19-9, CEA.
Staging and grading
Staging describes the diagnostic procedure following the diagnosis of a malignant tumor. In addition to the tissue examination (histology), staging plays a decisive role in the choice of therapy and statements on the prognosis.
Staging assesses the spread of the tumor in the organism.
As part of staging, the so-called Grading. The tumor cells are classified according to their differentiation. Differentiation in this case means to what extent the cells from the biopsy obtained match the original cells from which they originated.
Sonography
With sonography (Ultrasonic) one cannot assess abdominal organs invasively and without radiation exposure. With ultrasound of the abdomen (abdomen) one can assess the extent of the tumor in the gallbladder bed, the extent of the bile duct narrowing and discover the affected lymph nodes in the abdomen. Since the method is easy to use and does not burden the patient, the sonography can be repeated as often as required and used especially for follow-up and follow-up care.
Computed tomography (CT) creates slice images using X-rays and can provide information about the extent of the tumor, the spatial relationship to neighboring organs (infiltration), the lymph node involvement and, in addition, about distant metastases. It is not uncommon to need a CT scan of both the chest (thorax) and the abdomen (abdomen) in order to be able to assess all metastatic routes (liver and lungs). Magnetic resonance imaging (MRI) and a provide similar results MRI of the liver.
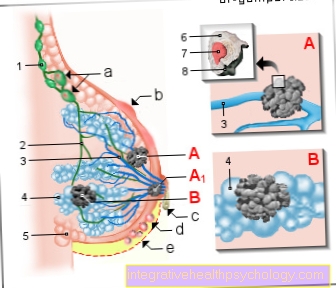
Endoscopic retrograde colangiopancreatography (ERCP) In this examination method, an endoscope with side-vision optics (duodenoscope) is advanced to the duodenum and the major duodenal papilla (Vater's papilla) is probed. This is the mouth of the common duct of the liver, gallbladder (ductus coledochus) and pancreas (ductus pancreaticus). If it is unsuccessful to push the instruments into the bile duct, it is necessary to carefully cut open the papillary opening in order to widen the opening. This measure is called a papillotomy or sphincterotomy.
In the second step of the examination, contrast agent is injected into these passages against the direction of flow of the digestive juices (retrograde). During the injection of the contrast agent, an X-ray image is taken of the upper abdomen. The contrast agent makes constrictions in the ducts (stenoses), caused by gallstones or tumors, for example, visible and therefore assessable. In addition, it is possible to take a tissue sample from the tumor (biopsy) via the endoscope and have it examined by the pathologist under the microscope (histologically).
Therapy can be carried out in the same session during the ERCP.
For example, an inserted instrument can be used to remove a stone or, in the case of constrictions caused by tumors or inflammation, by inserting a plastic or metal tube (stent), the bile and / or pancreas can drain again.
Percutaneous transhepatic cholangiography (PTC) If the display of the biliary tract using ERCP is unsuccessful, a percutaneous transhepatic cholangiography can be performed. In this method, the liver is pierced (punctured) through the skin with a hollow needle and a bile duct is found. As with ERCP, a contrast agent is injected here too in order to visualize the bile ducts by means of an X-ray. It is also possible in this way to drain the bile to the outside via a so-called percutaneous transhepatic drainage (PTD) in order to remove a backlog in the bile ducts. Particularly in the case of inoperable tumors, this can be used to provide relief from severe jaundice.
Chest X-ray:
An overview x-ray of the chest (chest x-ray) is made to provide information about metastasis of the lungs.
Read more on the topic: Chest x-ray (chest x-ray)
Endosonography (endoluminal ultrasound)
In an endoscopic ultrasound scan, as with a gastroscopy (esophago-gastro-duodenal endoscopy), a tube is first pushed into the duodenum (doudenum) in the immediate vicinity of the tumor. However, in this examination there is an ultrasound head at the end of the hose instead of a camera. With this method, the spread of the tumor in depth (infiltration) can be made visible by placing the transducer on the tumor and (regional) lymph nodes in the vicinity of the gallbladder can also be assessed.
Laparoscopy: In advanced tumor stages, it is sometimes necessary to perform a laparoscopy in order to correctly assess the regional extent, abdominal cavity involvement (peritoneal carcinosis) and liver metastases. During this procedure, which is carried out under general anesthesia, various instruments and a camera can be introduced through incisions in the skin of the abdomen and thus the spread of the tumor can be observed.

- Gallbladder Body -
Corpus vesicae biliaris - Right liver bile duct -
Ductus hepaticus dexter - Left liver bile duct -
Left hepatic duct - Gallbladder duct -
Cystic duct - Gallbladder Neck -
Collum vesicae biliaris - Mucous membrane -Tunica musoca
- Common
Liver bile duct -
Common hepatic duct - bile duct -
Common bile duct - Pancreatic duct -
Pancreatic duct - Extension of the united
Execution corridor -
Ampula hepatopancreatica - Large duodenal papilla -
Major duodenal papilla - Duodenum Descending Part -
Duodenum, descending part - Liver, diaphragmatic side -
Hepar, Facies diaphragmatica - Pancreas -
Pancreas
You can find an overview of all Dr-Gumpert images at: medical illustrations