Herpes simplex encephalitis
Synonyms in a broader sense
Encephalitis, brain inflammation, herpes
English: encephalitis, brain inflammation, brain-fever

definition
The through the Herpes simplex virus Type 1 (HSV1) triggered encephalitis is the most common form of one with around one new case per 100,000 inhabitants per year (5 per 100,000 in Western Europe) acute viral encephalitis (Encephalitis). If it is recognized and treated early, the prognosis is good. If left untreated, however, 70% of patients die, which is the reason that just because of suspicion, i. H. treated without identifying the pathogen GOT TO.
The herpes simplex virus is also the causative agent of the harmless Cold sore.
Read also on this topic Meningoencephalitis
Disease and symptoms
The herpes virus enters the central nervous system via the olfactory nerves and from there reaches the side lobes (temporal lobes) and the front lobes (frontal lobes) of the brain, initially only on one side (usually the left), later usually on both sides.
This is where the areas of the brain that are important for our language, memory and psyche are located, especially the limbic system.
This leads to bleeding and tissue destruction (necrotizing hemorrhagic encephalitis) and subsequently to extensive swelling around this area of the brain (cerebral edema), which can be seen well on MRI (magnetic resonance imaging) and which leads to the characteristic neurological and neuropsychological focus symptoms leads: Many patients can no longer speak, they have what is known as aphasia. Mild paralysis (hemiplegia) can also develop. In 60% of the cases, an epileptic seizure occurs (focal seizures, focus = focus). Neck stiffness and clouding of consciousness also occur. If left untreated, this can develop into a coma. Cranial pressure develops from which the patient can ultimately die.
Read more on the topic: Cerebral hemorrhage coma
How high is the risk of infection?
Herpes simplex viruses (type 1) are transmitted via secretion droplets that come from the human respiratory tract (droplet infection). One can become infected through direct contact with the mucous membranes in the mouth and throat area or through the absorption of secretion droplets into the air.
In adulthood, however, around 95% of people are infected with the herpes simplex virus (type 1). A renewed infection does not represent an increased risk of herpes encephalitis. The viruses persist in the nerve cells for life and are reactivated, especially when the immune system is weakened. There is a risk that the viruses migrate along the nerve fibers into the brain and trigger encephalitis (inflammation of the brain) there.
What is the route of infection?
Herpes simplex viruses (type 1) are transmitted by droplet infection. After the secretion droplets have been absorbed via the mucous membranes in the nasopharynx, the pathogens settle there. An inflammation in the surrounding area leads to a primary infection, which manifests itself in the form of fever and painful blistering in the oropharynx, especially in childhood. Then the virus is absorbed into the nerve endings running in the mucous membrane. Along these lines, the viruses can spread to nerve ganglia (a collection of nerve cell bodies) and persist there for a lifetime.
Due to a weakened immune system, the viruses can migrate again along the nerves and form the typical cold sores in the area where the nerves are supplied (often in the area of the lips). There is also the risk of the virus spreading along the nerves into the brain, which can lead to inflammation of the brain (encephalitis).
diagnosis
The quick detection of the genetic material of the herpes virus in the nerve water (Liqour) (DNA detection by means of PCR) is the most important form of diagnosis.
A small amount of nerve water must be obtained for this.
To remove it, a hollow needle is used between the 3rd and 4th or the 4th and 5th lumbar vertebrae into the subarachnoid space (space of the nerve water) below the spinal cord (lumbar puncture). It then drips through this needle into sterile tubes. Its appearance alone can provide clues as to the type of disease and possible pathogens. This procedure is medically known as CSF diagnostics.
Antibodies against HSV 1 are only produced from the 7th day and can be detected in the blood and nerve water. However, therapy must be started much earlier.
In the nerve water there is also an increase in cells to a few 100 per microliter (predominantly lymphocytes (white blood cells)) and an increase in protein content to 1.0 to 1.5 g / l.
You can find more information about the diagnosis of nerve water in our topic:
- CSF diagnostics
Magnetic resonance imaging (MRI) and the EEG give earlier indications of herpes simplex encephalitis. In the MRI, the tissue destruction can be seen one day after the onset of the symptoms, whereas the CT (computed tomography) shows no change in the first three days.
What can you see of the brain in the MRI?
With the help of magnetic resonance imaging (MRI), the early diagnosis of herpes encephalitis is possible. It is therefore the method of choice in early diagnosis, which means that therapy can be started at an early stage.
The MRI image of herpes encephalitis usually shows a typical infestation pattern. The viruses mainly spread to the areas of the temporal lobe and the limbic system (processing of emotions). There, the brain tissue is swollen (edema). A differentiation between the cerebral cortex and the brain marrow is no longer possible. Due to the accumulation of water in the course of the brain swelling, the areas of inflammation appear hyperintense (white) in T2-weighted frequencies of the MRI.
Read more at: MRI of the brain
therapy
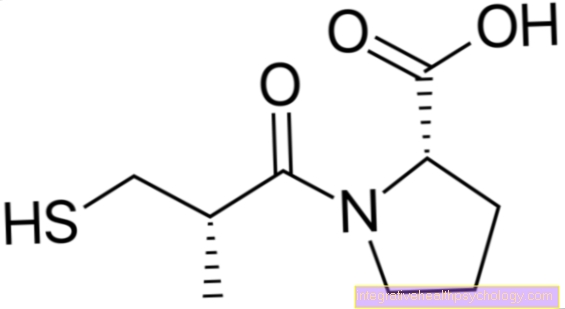
If there is justified suspicion, therapy must be started immediately Acyclovir be initiated. Acyclovir is a Nucleoside analogue, i.e. it is built into the DNA by the viruses instead of their own genetic material and thus leads to the breakdown of virus DNA synthesis (Replication).
Acyclovir is e.g. also in ointments for the therapy of Cold sore is used.
Herpes simplex encephalitis is treated intravenously (IV) and in high doses with 10 mg acyclovir per kg body weight, usually 750 mg, three times a day for at least 14 days.
Other drugs against the virus (Antivirals) are Famciclovir and Valaciclovir.
Against the cerebral edema, which always develops around inflammatory processes as swelling, glycerol 10% or mannitol 20% (Osmotherapy).
The treatment of epileptic seizures takes place with Phenytoin (Trade names in Germany: Epanutin ®, Phenhydan ® and Zentropil ®).
Phenytoin is a Anticonvulsant (anti-seizure drug) and works well against epilepsythat emanate from a specific focus (focal seizures, focus = focus), as is the case with the HSV encephalitis the case is.
forecast
If treatment is initiated quickly, around 80% of the patients survive, more than half of them without permanent sequelae. A memory disorder remains the most common neurological deficit. There is an increased risk after one Herpes encephalitis also for permanent seizure disorders (post-encephalitic epilepsy)that arise exactly in the brain region where the inflammation was previously: in the lateral (= temporal) lobe of the brain. You need an anticonvulsant (= epileptic cramps preventive) long-term therapy.
What are the long-term effects?
The various stages of herpes encephalitis occur very quickly. Serious complications with serious long-term consequences can therefore arise within a few days. For this reason, therapy must be started early. If antiviral treatment is started early, the probability of survival is around 80%.
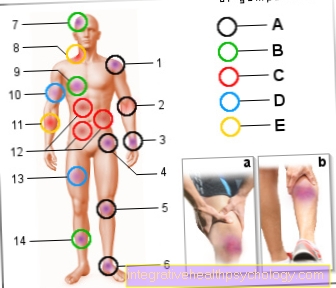
In the advanced stages of herpes encephalitis, the patient may experience dizziness, impaired perception (impaired vision, impaired sense of smell), paralysis and painful stiff neck. Due to the swelling of the brain tissue as part of the inflammation, there is a risk of the vital centers of the brain stem being trapped in the bony skull. An entrapment of the respiratory center means that death can occur more quickly.
In some cases, symptoms persist despite successful treatment of herpes encephalitis. In so-called postencephalitic epilepsy, the patient has frequent epileptic seizures. Drug therapy for epilepsy may be necessary. In addition, the patient may experience impaired memory or loss of memory. These depend on the affected brain region of the encephalitis (encephalitis).
Herpes simplex encephalitis in the baby
Herpes virus infection occurs in babies in two ways. One possibility is the infection already during the birth process if the mother is sick with genital herpes. Infection is also possible in the first few months of life from parents who have cold sores and other caregivers. As babies' immune systems are not yet fully developed, they are particularly at risk, as viruses can spread almost unhindered in the body.
With simple courses, only the skin, mucous membrane and conjunctivitis are involved.
In severe cases, the central nervous system is affected and thus herpes simplex encephalitis. This first shows up in flu-like symptoms with the baby being unable to drink. There is a high fever and seizures. The viruses lead to the destruction of important structures in the brain. It can lead to sequelae such as permanent neurological damage, developmental disorders and intellectual deficits. Despite treatment, fatal outcomes occur in 50-80% of cases.
The therapy of herpes simplex encephalitis consists, as in adults, of an antiviral therapy with acyclovir intravenously for 14 days. Furthermore, a lowering of the fever, an anti-spasmodic therapy for seizures and, if necessary, therapy for intracranial pressure should be carried out.
Read more on the subject at: Herpes in babies - how dangerous is it?