Platelets
definition
Both Platelets it is about Plateletseach of which is human around 150,000 to 350,000 per µl blood carries in itself.
The platelets perform a important function in blood clotting. So platelets ensure that when a patient cuts, the Wound as quickly as possible and with as little blood loss as possible locked again will be without before lost too much blood goes.
A Platelet imbalance (too many or too few platelets) can lead to various diseases. Because the platelets from the so-called megakaryocytes arise which in Bone marrow can be formed, among other things, a Malfunction in the bone marrow be responsible for the decreased or increased platelet count. A normal platelet count is also important, as platelets can be a contributory factor Heart disease and Calcification of the blood vessels (arteriosclerosis).

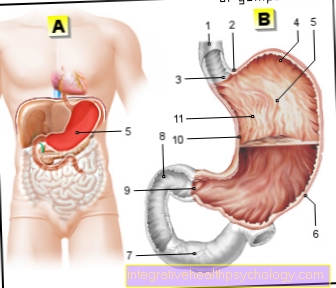
construction
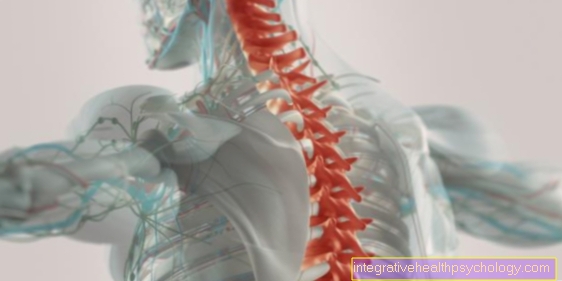
Thrombocytes, also called blood platelets, are constrictions from their precursor cells, the so-called megakaryocytes located in the bone marrow. In the non-activated state, they correspond to a biconvex disc, that is, it bulges in both directions. This particular form of platelets is stabilized by a kind of fibrous support structure, the microtubules. In addition, they have a fiber system which gives them the ability to change their shape when activated and to form a large number of runners, so-called pseudopodia, which then serve as contact points for attachment and mutual networking.
Due to the fact that the platelets are only constrictions, they are also not considered to be full-fledged cells and also do not have a cell nucleus, which means that further cell division is excluded. So-called mitochondria, the energy-generating organs of the cell, are still contained in the platelet, which provides the necessary energy for the activation process. The platelets also contain different types of beads, so-called granules. These can contain messenger substances or enzymes that promote coagulation and are released when activated.
function
The platelets perform a crucial function in blood clotting. If a patient cuts their finger, it starts to bleed briefly, but after a few seconds the bleeding stops and does not last for minutes. They have the function of doing a little locally Platelet clots (white platelet thrombus) in the event that a blood vessel is damaged, and to strengthen the clotting of the coagulation factors. Without the platelets, people would suffer minor injuries or spontaneous bleeding, e.g. from the nose, bleed to death. The platelets are coming as soon as there is damage from Blood vessels comes with the so-called von Willebrandt factor in contact, which is usually due to the intact tissue has no contact with the platelets. The von Willebrandt factor together with the platelets lead to a Platelet aggregation, that means that the platelets by the Willebrandt factor glue together. This becomes a Plug formed which closes the defective point in the blood vessel. So it comes hemostasis very quicklytriggered by the platelets.
This process is described as primary hemostasis or cellular hemostasis (synonym for hemostasis: Hemostasis). In addition, in the context of secondary hemostasis, the Activated clotting factors of the blood. The protein fibrinogen is activated, which, after its activation, accumulates as fibrin and also forms connections with the existing platelet network. This creates an even denser clot in which red blood cells can get caught, so that a piece of solid tissue is created that reliably closes the injury site of the vessel and thus stops the bleeding.
Hence it is also clear that the platelets are always sufficient quantity should be present in the blood, otherwise a adequate hemostasis not possible is. At the same time, too not too many platelets be present so that it does not become an increased one Blood clot formation (thrombus) is coming. These thrombi can become procrastinate and then to one Pulmonary embolism to lead. Besides, it can too deep vein thrombosis and other diseases, sometimes too Heart problems, come. This is especially the case when patients many risk factors wear. Women are more likely to be of Leg vein thrombosis affected than men. Other risk factors are as well Obesity, Smoketaking oral contraceptives, little movement and drink little as well as too greasy eat. All of these risk factors favor storage together of platelets.
Because in general: The slower the blood flows the more time there is for the platelets contained in it to assemble.
If a person does not drink much, the blood flow slows down because that Blood more viscous becomes. If a patient moves too little, the blood builds up in the legs and there is increased accumulation of platelets in the leg veins (deep vein thrombosis). These examples show that it not the platelets themselves that “fail” in a thrombosis because they cluster together and form a thrombus. Rather, it's them circumstancesin which they are located, i.e. the blood and the vessels through which they flow. Of course there is also one family history, which plays an important part in the formation of thrombi, i.e. the aggregation of platelets. In general, however, it is true that platelets fulfill their function very wellas long as they are not exposed to too many risk factors.
Platelet aggregation
When a vessel is injured, the platelets come into contact with the connective tissue, which normally has no contact with the blood. A coagulation factor, the so-called. von Willebrand factor (vWF), accumulate from the blood. The platelet has special receptors for this factor (vWR) and binds to it. This leads to the adherence of the platelets, also known as adhesion. This is also the stimulus for the platelets to activate them. They change their disc shape and form many runners (Pseudopodia) out. They also release the contents of their granules, which contain coagulation factors and other platelet-activating substances. The latter include, for example, adenosine diphosphate (ADP) or thromboxane. This solves a kind Chain reaction off so many more platelets activated can be.
The activation of the platelets leads to a change in the shape of the protein GPIIb / IIIa on their surface. This works as a receptor for a plasma protein called fibrinogen. It acts as a bridge bond between platelets and connects them to one another via the GPIIb / IIIa. A network of platelets linked via fibrinogen can therefore form at the injury site. This network is known as the "white platelet thrombus" and the process is known as platelet aggregation. In the further course, the coagulation factors of secondary hemostasis are activated and a very stable cross-linked thrombus is formed.
Antiplatelet drugs
For some diseases or conditions, platelet aggregation must be inhibited. On the one hand there is the tried and tested ASS (Acetylsalicylic acid) which inhibits an enzyme (COX-1) that produces the thromboxane necessary for aggregation. In addition, the receptor molecules of the platelets can also be inhibited. So-called ADP receptor blockers (Synonym: P2Y12 receptor blockers) can also prevent activation of the platelets by the adenosine diphosphate. These include, for example Clopidogrel or Ticagrelor.
Last but not least, the cross-linking of the platelets via the receptor called GPIIb / IIIa can be prevented. These drugs, which unfortunately cannot be taken orally, include, for example Abciximab.
- ASS
- Clopidogrel
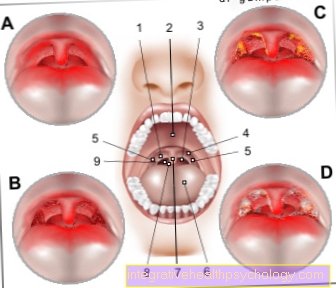
Blood count
in the small blood count will always be the Number of platelets determined as it has an important function in the Coagulation cascade fulfill. The platelets are here as small platelets without a nucleus recognizable. You see compared to the white blood cells (Leukocytes) and the red blood cells (Erythrocytes) are tiny and are therefore particularly noticeable. They are also in the blood count most frequently representedso that many small round "dots" appear between individual larger erythrocytes and leukocytes.
Generally, platelets are right round but not always circular, about 1-4 µm big and very flat. They survive in the blood about 5-12 days then they will be in the spleen, liver or in the lung reduced.
Since a blood sample has an enormous number of platelets, these must be counted with a fully automated measuring device as it would take a human too long. So that the platelets do not clump together in the blood sample, an additive is always added, which prevents the platelets from accumulating and then lying as a large lump at the bottom of the blood sample, because that way you could no longer count the individual platelets add ethylenediaminetetraacetate, or EDTA for short, to the blood sample. The blood along with the anti-coagulant is called EDTA blood. Usually the platelets in this EDTA blood do not clump together. However, it rarely happens that despite the EDTA, some platelets clump together and settle at the bottom of the blood sample. The automatic counting machine cannot record these clumped platelets because they are too large for a normal platelet when stacked together. As a result, the meter will indicate that the patient is low on platelets when it is not. The doctor speaks of pseudothrombocytopenia. To prevent this wrong diagnosis, citrate can therefore be added to the blood instead of EDTA. The platelets do not clump together in these citrate tubes and can then be correctly evaluated.
Numerical values / number
The number of platelets in the blood has a Standard range of 150,000-400,000 pieces / µl (one µl corresponds to 0.001 l). A value below this (> 150,000 / µl) is called defect and in technical terms as Thrombopenia (see below). Values above (450,000 - 1000,000 / µl) are called excess and Thrombocytosis (see below) designated. This is usually limited in time and can arise as a reaction to trauma, surgery, blood loss or chronic inflammation. If the number of platelets per µl exceeds one million, one speaks of one Thrombocythemiawhich can occur in certain diseases of the bone marrow.
Thrombocytosis
= too many platelets
A patient has too many platelets when the number of platelets in the blood rises to over 360 thousand / µl blood.
This can have different causes. For example, an increased number of platelets (thrombocytosis) occurs after removal of the spleen, since the spleen is an organ that breaks down platelets. If the spleen can no longer break down the platelets, more platelets automatically accumulate.
If there is a major loss of blood, for example during an operation or an accident, it is a reflex that the body produces more platelets in order to be able to close the wounds. Accordingly, there is often an increased number of platelets in the blood after major surgery. Since this poses a risk of thrombus formation, so-called anticoagulants are often given after major operations or injuries, i.e. drugs that prevent platelets from accumulating and thus make the blood more fluid. A blockage of the blood vessels by platelets is therefore very unlikely, but the risk of bleeding increases.
The number of platelets can also increase in inflammatory processes, as well as in diseases of the bone marrow. The thrombocytes arise from the so-called megakaryocytes, which in turn arise from stem cells via several intermediate stages in the spinal cord. If overstimulation occurs during this maturation process, an increased number of platelets are formed as a result.
Read more on the topic: Thrombocytosis
Thrombocytopenia

= too few platelets
One patient has too few plateletsas soon as the number of platelets in the blood increases below 140,000 per µl of blood falls. This can various causes to have.
After a more severe infection for example, it is normal for the The number of platelets decreases because many platelets were "used up" by the infection.
It can also be with one Vitamin B12 or folic acid deficiency to a so-called megaloblastic anemia come to the Number of all cellular components of the blood is decreased. The platelet count also drops in very low physiological ranges or is pathologically decreased, then it is a thrombocytopenia. These two causes are arguably the most common causes for platelet depletion, however, there is also far worse, but just rare causes.
On the one hand, this includes one pathologically low platelet count owing to blood cancer (leukemia). Here is the normal bone marrow displaced and thus the number of normally present in the blood decreases mature blood cells are partially replaced by immature cells. Thus one finds not just platelets in the blood but also partly Megakaryocytes.
But not just blood cancer may be responsible for one Thrombocytopeniabut also the Use of certain medications like for example Chemotherapy drugs after or during a Cancer treatment. Here it is especially important that Monitor blood counts regularly.
Additionally there is various autoimmune diseases in which autoantibodies against the platelets are formed. These autoantibodies ensure that the Platelets broken down will and will produced by the body itself (therefore "auto-"). To be mentioned are those idiopathic thrombocytopenic purpura (ITP) and the Lupus erythematosus disseminatus. In very rare cases, a increased intake of lead (Lead intoxication) ensure that the platelet count is reduced.
Especially in the elderly can a premature breakdown of platelets occur more often. This can be done for example by a artificial heart valve be the case or due to a dialysis with extracorporeal circulation.
A decreased number of platelets is mainly characterized by a increased tendency to bleed out. The patients bleed faster and the bleeding may be partial difficult to stop. Usually one recognizes a thrombocytopenia by the fact that the patient punctiform hemorrhages in the legs and the rest of the body (Petechiae).
Platelet donation
In injuries or surgery where there is significant blood loss, or in people who are unable to make enough platelets due to their illness (s), it may be necessary for platelets to be given to them by other people not artificially produced can be. This happens nowadays in the form of Platelet concentrates.
Donations can be in the form of a Whole blood donation happen in which half a liter of whole blood is drawn. This is followed by processing and separation into individual components. Alternatively, a pure platelet donation take place during which the donor is connected to a separating machine in which only the platelets are selectively filtered out. Meanwhile, the remaining blood components are returned to the donor. This method takes a little longer.
It is legally regulated that the donation should be made free of charge. However, the donor can be paid an expense allowance depending on the effort. This varies depending on the type of donation and the organization, although some do not spend any compensation in the form of money. For a whole blood donation, an amount of approx. € 20 can be expected, whereas a pure platelet donation brings a slightly higher expense allowance of approx. € 25-40, as the procedure takes longer overall.


















.jpg)