Cardiac arrhythmia
Synonyms in the broadest sense
- Cardiac arrhythmias
- arrhythmia
- Tachycardia
- Bradycardia
- Atrial fibrillation
- Atrial flutter
- Extrasystoles
- Sick sinus syndrome
- AV block
- supraventricular arrhythmia
- ventricular arrhythmia
definition
A cardiac arrhythmia (also called arrhythmia, "non-rhythmic") is a disruption of the normal heartbeat sequence, caused by irregular processes in the formation and conduction of excitation in the heart muscle. Cardiac arrhythmias can be life-threatening and occur as a result of diseases of the heart or other diseases. But they also occur in organically healthy people and cannot have any disease value.
anatomy
The cardiac arrhythmia is a change in the "normal" heart rhythm. To understand how the different types of cardiac arrhythmias differ and how they arise, it is helpful to take a look at the basics of the anatomy and physiology of the heart.
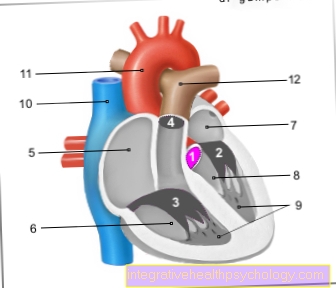
The human heart has four components: the right and left atria, and the left and right ventricles. The right and left halves of the heart are separated from the heart septum. The oxygen-poor blood of the circulatory system reaches the right atrium via the large vena cava inferior and superior vena cava. When the right atrium contracts, the blood is forced into the right ventricle. The contraction of the right atrium is followed by the contraction of the right ventricle, which pumps the blood into the lungs. The now oxygenated blood flows from the lungs into the left atrium, then into the left ventricle and from here into the aorta.
The blood can only flow in one direction in the heart, this is ensured by the heart valves. There are four heart valves, two so-called leaflet valves that lie between the atrium and ventricle and two so-called pocket valves that lie between the heart chambers and the large outflowing vessels, i.e. the pulmonary arteries and the aorta.

- Right atrial -
Atrium dextrum - Right ventricle -
Ventriculus dexter - Left atrium -
Atrium sinistrum - Left ventricle -
Ventriculus sinister - Aortic arch - Arcus aortae
- Superior vena cava -
Superior vena cava - Lower vena cava -
Inferior vena cava - Pulmonary artery trunk -
Pulmonary trunk - Left pulmonary veins -
Venae pulmonales sinastrae - Right pulmonary veins -
Venae pulmonales dextrae - Mitral valve - Valva mitralis
- Tricuspid valve -
Tricuspid valva - Chamber partition -
Interventricular septum - Aortic valve - Valva aortae
- Papillary muscle -
Papillary muscle
You can find an overview of all Dr-Gumpert images at: medical illustrations

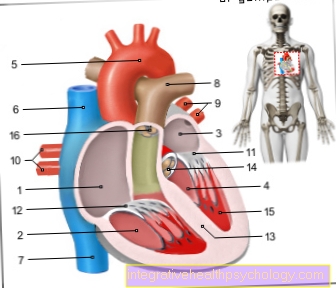
- Sinus node -
Nodus sinuatrialis - AV node -
Nodus atrioventricularis - Trunk of the excitation conduction
systems -
Atrioventricular fasciculus - Right thigh -
Crus dextrum - Left leg -
Crus sinistrum - Rear thigh branch -
R. cruris sinistri posterior - Front thigh branch -
R. cruris sinistri anterior - Purkinje fibers -
Subendocardiales - Right atrial -
Atrium dextrum - Right ventricle -
Ventriculus dexter
You can find an overview of all Dr-Gumpert images at: medical illustrations
Basics / Physiology of the Heart
The heart rhythm is the chronological sequence of contractions of the "pumping organ" heart.The cardiac performance is ensured by a regular rhythm of the heart's actions. A “heartbeat” actually consists of two contractions in quick succession (contraction of the Heart muscle), those of the atrium and the subsequent contraction of the ventricle. A cardiac arrhythmia can therefore be classified based on two criteria:
- Place of origin = where the disorder occurs, in the atrium or the ventricle
- Type of rhythm change = the heart beats faster overall (tachycardia) or slower (bradycardia)
There are many other ways of classifying cardiac arrhythmias, some of which are, however, very complicated because they require a great basic knowledge of physiology (the function of the organ systems). The classification chosen here is one of the most common in everyday clinical practice.
What makes the heart beat? The peculiarity of the heart is its own generation of electrical stimuli, which cause the muscle cells to contract. A distinction is made between the actual working muscles and the stimulus conduction or stimulus generation system. Different areas of the heart have cells that can independently generate electrical potentials. These potentials are then led to the actual working muscles through the conduction system. It converts the electrical stimuli into a contraction.
The stimulation system includes the sinus node, the AV node and subordinate excitation centers. The Sinus node can best be imagined as the great pacemaker. In healthy people, the frequency of the sinus node determines how often the heart beats per minute (approx. 60-90 times).
Its cycle is passed on by the stimulus conduction system to the other stimulation centers, which then adjust their frequency, one speaks of Sinus rhythm. If the sinus node fails, however, the other excitation centers can partially take over its task. The sinus node is located in the right atrial muscles, its stimuli are transmitted directly to the working muscles of the atria and to the AV node forwarded. He is also the authority that the Heart rate permanently adapted to the needs of the organism, e.g. it accelerates the heartbeat during exercise and slows it down during sleep. The AV node is located in the muscles between the atria and ventricles, it transmits the sinus impulses to the bundle of His with a delay. If the sinus node fails or the stimulus conduction is blocked, it can also become a clock itself. However, its frequency of 40-50 beats per minute is well below the rate of the sinus node.
The Conduction system connects the sinus and AV nodes and leads from there to the working muscles of the chambers. After the AV node, the so-called closes His bundle that according to the discoverer into a right and left Tawara thigh is divided. These finally conduct the electrical stimuli to the Purkinje fibersthat end in the cardiac muscle layer of the chambers.
This results in a further classification option for cardiac arrhythmias:
- Charmeducationaldisorder (here the problem lies in the sinus or AV node) or
- Charmmanagementdisturbance (this is where the problem lies with the transmission of the impulses)
Classification of cardiac arrhythmias
In bradycardia, the heart beats slowly and the pulse is less than 60 beats per minute. Bradycardia can often be observed in competitive athletes without being pathological.
The two main arrhythmias associated with bradycardia are:
Bradycardium =
- Sick sinus syndrome
- AV block
In tachycardia, the heart beats unusually fast, the pulse is over 100 beats per minute. Tachycardia can also occur with great excitement and physical exertion.
Tachycardiac arrhythmias are further subdivided according to their origin:
Tachycardia supraventricular arrhythmias
(Supraventricular = supra- = over -ventricular = from the ventricles (chambers), i.e. in the atria.)
- Supraventricular extrasystoles
- Supraventricular tachycardias
- AV Node Reentry Tachycardia = Wolff-Parkinson-White (WPW) Syndrome
- Atrial flutter
- Atrial fibrillation
Tachycardia ventricular arrhythmias
- Ventricular extrasystoles
- Ventricular tachycardias
- Ventricular flutter
- Ventricular fibrillation
Causes: As already mentioned, cardiac arrhythmias can also occur in physically healthy people. They usually only appear sporadically in special situations and are of short duration. Frequent or prolonged arrhythmias, on the other hand, can usually be traced back to three specific causes:
- Metabolic disorders e.g. medication or an overactive thyroid
- Heart diseases e.g. a heart attack
- congenital abnormalities
Various heart diseases are the most common cause of the development of irregular heartbeat. Due to a reduced oxygen supply or direct damage to the heart muscle cells, these can no longer work properly. Heart diseases that can lead to arrhythmias include:
- Coronary heart disease (CHD),
- Heart failure (heart failure),
- Valvular heart disease,
- Myocarditis or
- High blood pressure.
Conditions that can lead to arrhythmias
This also includes metabolic disorders, the risk factors for the aforementioned heart diseases, in particular for CHD.
- Hyperthyroidism: With an overactive thyroid, the increased secretion of thyroid hormones can lead to tachycardiac arrhythmias.
- Sleep apnea syndrome: sleep apnea syndrome refers to the occurrence of short pauses in breathing during sleep. This can lead to bradycardia and other cardiac arrhythmias.
- Hypoxia (insufficient supply of oxygen): diseases of the lungs that lead to a reduced supply of oxygen to the organism or states of shock can cause secondary damage to the heart. This in turn can lead to the occurrence of arrhythmias.
- Obesity (abnormal overweight): It is a risk factor for arrhythmias, especially atrial fibrillation, as well as for CAD
- Diabetes mellitus ("sugar"): the large and small vessels of the body are damaged by diabetes mellitus, it is a risk factor for CHD
- Medication: many medications can lead to arrhythmias as a side effect, which is why a precise medication history is essential if arrhythmias occur.
- Alcohol: Excessive consumption of alcohol can lead to cardiac arrhythmias.
- Stress: The first thing that can happen is a palpitations of the heart due to stress, which can develop into cardiac arrhythmias with prolonged stress and persistent palpitations.
- Pulmonary hypertension (pulmonary hypertension): The right half of the heart has to constantly pump against the high blood pressure in the lungs when the disease occurs.
If the heart can no longer apply the necessary pressure, however, the right ventricle and the right atrium in the heart enlarge.
The result is cardiac arrhythmia.
Read more on the topic: Symptoms of a heart attack
Certain arrhythmias
In the following, the individual arrhythmias are described in more detail and explained how they arise and what symptoms they are associated with.
The most important tool for diagnosing cardiac arrhythmias is the EKG (electrocardiography). Various cardiac arrhythmias lead to characteristic changes in the EKG. These are also described here. To be able to “read” an EKG correctly is unfortunately a very difficult thing that requires a great deal of knowledge of the physiological processes in the heart. Following the description of the individual cardiac arrhythmias, you will find some explanations of the basic functionality of an ECG.
Read more about this:
- Absolute arrhythmia
- Heart rhythm disorder
Therapy cardiac arrhythmias
general therapy
Not every Cardiac arrhythmia Immediate therapy is required, as many forms - especially for people with otherwise healthy heart - pose no threat and do not lead to any physical limitations.
The most common rhythm disturbances in people with healthy heart are the extra beats, also called extrasystoles. Therapy is therefore only necessary if a rhythm disturbance occurs in an already stressed heart or the accompanying symptoms lead to subjectively strong physical or psychological impairments.
A distinction is generally made between:
- medicinal
- electrical and
- invasive therapy,
the type of rhythm therapy depending on the type of disorder (tachycardiac, bradycardiac disorder, extra beats Etc.). In the drug, antiarrhythmic therapy, several drugs are used, which are divided into four different classes:
to 1st class include substances that block so-called sodium channels in the heart (e.g. flecainide)
to 2nd class those that block? 1 receptors (beta blockers, e.g. metoprolol)
to 3rd class Potassium channel inhibitors (e.g. amiodarone) and
to 4th grade those that inhibit calcium channels (e.g. verapamil).
The aim of all of these drugs is to regulate and stabilize the heart rate.
The so-called electrical therapy includes, on the one hand, the implantation of a cardiac pacemaker for cardiac arrhythmias that cause a heartbeat that is too slow. The electrical device stimulates the muscles of the heart to contract in a certain rhythm, so that sufficiently regular pumping is guaranteed.
On the other hand, it also belongs Implantation of a defibrillator for electrical therapy, which is preferably used for rapid rhythm disturbances (e.g. ventricular fibrillation). If the device registers the rhythm that is getting out of hand, it sends a surge of electricity to the heart, which usually returns it to a normal, regulated rhythm.
An external electric shock can also be used to protect the heart in the event of cardiac arrhythmias, especially in the atrium (e.g. Atrial flutter, atrial fibrillation) to bring it back into its normal rhythm. This procedure is called electrical cardioversion and is performed under brief anesthesia with a lower dose than defibrillation (medical cardioversion can also be performed without anesthesia!).
The so-called catheter ablation is one of the invasive rhythm therapy methods. The locations of the arrhythmias are specifically searched for during a cardiac catheter examination and then the heart tissue, which is responsible for the arrhythmia, is electrically obliterated.
Beta blockers
Beta blockers are drugs that are able to use certain receptors, so-called? -Receptors (Beta receptors) to block the human body and thus the effects of stress hormones adrenaline/ Norepinephrine to prevent these receptors.
They are preferably used in so-called tachycardiac arrhythmiasas arrhythmias in which the heart beats with too many beats per minute.
There are two different forms of these receptors in the human organism, one variant is located on the heart (? 1) and the other on the blood vessels (? 2), so there are also different types of beta blockers, depending on which receptor is to be blocked (selective? 1 or? 2 or unselective both receptors).
As part of the therapy of cardiac arrhythmias, preference is given to using beta blockers that only act on the? 1 receptors of the heart (e.g. Metoprolol, Bisoprolol) and dampen the heart's beating activity. Since there are also some other antiarrhythmics available for the therapy of arrhythmias, these are divided into 4 classes, with the beta blockers forming the 2nd class.
In contrast to most other antiarrhythmics, beta blockers have a proven, life-prolonging effect, so that they are of great importance in cardiac rhythm therapy and are used as the means of choice to down-regulate and normalize the conduction of excitation in the heart.
What are the signs of an arrhythmia?
Recognize an abnormal heart rhythm
In addition to the typical symptoms that can cause cardiac arrhythmias, an initial physical examination can already provide evidence of a rhythm disorder:
By feeling the pulse (e.g. on the wrist; also very easy to do independently) or by listening to the heart with a stethoscope by a doctor, irregularities in the beat of the heart can easily be detected.
Often the blood pressure is also measured so that the doctor can get an overall picture of the condition of the cardiovascular system. In order to secure the diagnosis of a cardiac arrhythmia and above all to determine the exact type of the arrhythmia, an ECG (Electrocardiography) written.
The electrical currents of the heart are measured by electrodes and recorded by a device.
The EKG can under rest conditions (relaxed while lying down) or under stress conditions (while running or cycling), depending on whether it is a rhythm disturbance that only occurs during physical exertion or even at rest. If the cardiac arrhythmia does not persist, a long-term ECG (a portable EKG device measures the heart rate 24 hours a day) or a so-called event recorder (Portable ECG device that the patient uses to take measurements whenever symptoms occur) enable the sporadic arrhythmias to be recognized.
Symptoms of arrhythmia
The symptoms of cardiac arrhythmias can be just as diverse as there are different types of arrhythmia. As a rule, they occur with changes in the beat frequency> 160 / min and <40 / min and with all beat irregularities that lead to disorders in the cardiovascular system.
In some cases they can appear completely symptom-free, so that the person concerned does not feel any changes and the diagnosis is made by chance as part of routine examinations at the family doctor.
However, arrhythmias are often accompanied by more or less mild symptoms, so that otherwise hearty people will notice the rhythm changes in the form of so-called palpitations:
This means a palpable racing heart, stumbling or beating loudly, caused by extra blows, dropouts or short-term accelerations. Many people affected even report that the irregular knocking can even be felt in the throat.
Whenever the cardiac arrhythmias lead to disturbances in the blood supply to the body (e.g. in the case of slow rhythm disturbances or disturbances with stopping strokes, so that the blood flow is (briefly) restricted), additional symptoms such as dizziness and disorientation can - depending on the severity , Visual or speech disorders, collapse or fainting (syncope).
If cardiac arrhythmias occur in patients who already have a previously damaged heart (heart failure), this can lead to a deterioration in the condition of the heart. This usually manifests itself in a new or worsening shortness of breath, feelings of tightness in the chest, heart pain (angina pectoris) or even an accumulation of fluid in the lungs (pulmonary edema).
Cardiac arrhythmias are generally common and often they are not life-threatening. It always becomes dangerous if an already damaged heart suffers from an additional rhythm disturbance or if there are severe conduction disorders that the blood output of the heart is no longer sufficient. Such life-threatening conduction disorders include z. B. Ventricular flutter, ventricular fibrillation and 3rd degree AV block without a substitute rhythm.
Signs of an abnormal heart rhythm
Not every cardiac arrhythmia causes clear physical symptoms, so that in many cases they go unnoticed for a long time and are more likely to be discovered by chance during routine examinations.
However, if they lead to noticeable symptoms, the first signs of arrhythmia can be a sensation of palpitations (palpitations, with extra beats or short skips) heart palpitations or palpitations (with fast heartbeat), which can be felt up to the neck.
If the pumping function of the heart and thus the blood ejection is impaired by the rhythm disturbance, dizziness, lightheadedness, fainting or unconsciousness attacks can also be signs.
But heart pain and tightness in the chest (angina pectoris) can also be a sign of cardiac arrhythmias, especially when the heart can no longer be adequately supplied with blood and oxygen itself due to the irregular beats and is overloaded.
Read more on this topic at: Heart pain and pressure in the chest- what to do
Cardiac arrhythmia in children
In principle, all types of cardiac arrhythmias that occur in adults can also be present in childhood. In most cases, however, these are not acquired, as is the case with adults, but rather from the beginning congenital arrhythmias (e.g. congenital heart defects, heart valve defects, heart muscle diseases, etc.).
In some cases, cardiac arrhythmias can occur sporadically in adolescents and "grow together" again in the course of development. It should also be noted that it is completely normal for children to have a faster heartbeat than adults and therefore not always have a rapid cardiac arrhythmia.
The symptoms in children and adolescents are similar to those in adults, but they are less Signs in small children and infants due to the limited or insufficient ability to communicate from:
Changes in behavior, tiredness or restlessness, tearfulness, unwillingness to drink / eat, paleness, blue discoloration and lack of strength can all indicate cardiac arrhythmias that lead to physical impairment.
Cardiac arrhythmia in menopause
The Menopause the woman - too climacteric called - mean a significant hormonal change for the female body:
by the decrease in the production of the hormones estrogen and progesterone in the Ovaries the woman.
The typical symptoms of menopause arise in particular from the lack of estrogen, so that, for example:
- Hot flashes
- Sweats
- sleep disorders
- Irritability and nervousness as well too
- Joint and muscle pain
- Painful intercourse
- Bleeding disorders and osteoporosis
can come.
But the hormone deficiency is also noticeable in the heart, so that many women during menopause complain of palpitations and noticeable palpitations or stumbling.
The cause lies in the lack of effectiveness of the female hormones:
In the area of the cardiovascular system, estrogen is primarily responsible for expanding the blood vessels, so that on the one hand the blood pressure is lowered, the heart does not have to pump as hard and is better supplied with blood.
A lack of estrogen therefore causes a constriction of the vessels and thus an increase in blood pressure and extra work for the heart. In addition, an estrogen deficiency has a positive effect on the autonomic nervous system, making it more easily excitable. Since the vegetative Nervous system is also involved in controlling the heart, the increased sensitivity makes itself excitable here too, so that an increase in the Beat frequency and Arrhythmia may occur.
Arrhythmia and thyroid
The thyroid can always cause cardiac arrhythmias if it is overactive in its function and produces too many thyroid hormones, so that an excess of these occurs in the blood system (hyperthyroidism = Hyperthyroidism).
A benign lump in the thyroid tissue also leads to an overactive thyroid. This also affects the functioning of the heart. Read more on the subject below: Autonomous adenoma of the thyroid gland
This is mostly the case in the context of certain thyroid diseases, such as the autoimmune disease Graves' disease or an autonomy of thyroid tissue. Excessive intake of drugs containing thyroid hormones can also lead to an oversupply.
The effect of thyroid hormones in the body is varied, so that, among other things, they increase the basal metabolic rate, increase the excitability of nerve and muscle cells and stimulate the phosphate and calcium metabolism.
In the heart they also cause an increase in the sensitivity of the ß1 receptors to stress hormones, so that the effect of adrenaline and noradrenaline on the heart is increased. An oversupply of thyroid hormones therefore means that the heart is made overexcitable, so that cardiac arrhythmias such as tachycardia (strongly accelerated heartbeat,> 100 beats / minute), extra beats or even atrial fibrillation can occur.