Hormones
definition
Hormones are messenger substances that are formed in glands or specialized cells of the body. Hormones are used to transfer information to control metabolism and organ functions, with each type of hormone being assigned a suitable receptor on a target organ. To get to this target organ, hormones are usually released into the blood (endocrine). Alternatively, the hormones act on neighboring cells (paracrine) or on the hormone-producing cell itself (autocrine).

Classification
Depending on their structure, hormones are divided into three groups:
- Peptide hormones and Glycoprotein hormones
- Steroid hormones and Calcitriol
- Tyrosine derivatives
Peptide hormones are made up of protein (peptide = protein), Glycoprotein hormones also have a sugar residue (protein = protein, glykys = sweet, "sugar residue"). After their formation, these hormones are initially stored in the hormone-producing cell and only released (secreted) when required.
Steroid hormones and calcitriol, on the other hand, are derivatives of cholesterol. These hormones are not stored, but released directly after their production.
Tyrosine derivatives ("tyrosine derivatives") as the last group of hormones include catecholamines (Adrenaline, norepinephrine, dopamine) as well as thyroid hormones. The backbone of these hormones is made up of tyrosine, a amino acid.
General effect
Hormones control a large number of physical processes. These include nutrition, metabolism, growth, maturation and development. Hormones also influence reproduction, performance adjustment and the internal environment of the body.
Hormones are initially formed either in so-called endocrine glands, in endocrine cells or in nerve cells (Neurons). Endocrine means that the hormones are released “inwards”, i.e. directly into the bloodstream and thus reach their destination. The transport of the hormones in the blood takes place bound to proteins, whereby each hormone has a special transport protein.
Once at the target organ, hormones unfold their effects in different ways. First and foremost, what is required is a so-called receptor, which is a molecule that has a structure that matches the hormone. This can be compared with the “key and lock principle”: the hormone fits exactly like a key into the lock, the receptor. There are two different types of receptors:
- Cell surface receptors
- intracellular receptors
Depending on the type of hormone, the receptor is located on the cell surface of the target organ or within the cells (intracellular). Peptide hormones and catecholamines have cell surface receptors, steroid hormones and thyroid hormones, on the other hand, bind to intracellular receptors.
Cell surface receptors change their structure after the hormone binding and in this way set a signal cascade in motion inside the cell (intracellularly). Reactions with signal amplification take place via intermediate molecules - so-called “second messengers” - so that the actual effect of the hormone finally occurs.
Intracellular receptors are located within the cell, so that the hormones first have to cross the cell membrane (“cell wall”) that borders the cell in order to bind to the receptor. After the hormone has bound, the gene reading and the protein production influenced by it are modified by the receptor-hormone complex.
The effect of the hormones is regulated by activation or deactivation by changing the original structure with the help of enzymes (catalysts of biochemical processes). If hormones are released at their place of formation, this happens either in an already active form or, alternatively, they are only activated peripherally by enzymes. The deactivation of the hormones usually takes place in the liver and kidneys.
Functions of hormones
Are hormones Messenger substances of the body. They are used by various organs (for example thyroid, adrenal, testes or ovaries) and released into the blood. In this way they are distributed to all areas of the body. The different cells of our organism have different receptors to which special hormones bind and thus transmit signals. In this way, for example, the Cycle or the Regulates metabolism. Some hormones also act on our brain and influence our behavior and our feelings. Some hormones are even only IM Nervous system to find and convey the transfer of information from one cell to the next to the so-called Synapses.
Mechanism of action

a) Cell surface receptors:
After the to the Glycoproteins, peptides or Catecholamines hormones belonging to the cell have bound to their specific cell surface receptor, a multitude of different reactions take place one after the other in the cell. This process is known as Signal cascade. Substances involved in this cascade are called "second messenger"(Second messenger substances), in analogy to the as"first messenger“(First messenger substances) called hormones. The ordinal number (first / second) refers to the sequence of the signal chain. At the beginning there are the hormones as the first messenger substances, the second follow at different times. The second messenger include smaller molecules like cAMP (zcyclical A.denosinemonophsophat), cGMP (zcyclical Guanosinemonopphosphate), IP3 (I.nositoltripphosphate), DAG (D.iacylGlycerin) and calcium (Ca).
For the cAMP-mediated signal path of a hormone is the participation of so-called coupled to the receptor G proteins required. G proteins consist of three subunits (alpha, beta, gamma), which have bound a GDP (guanosine diphsophate). With hormone-receptor binding, GDP is exchanged to GTP (guanosine triphosphate) and the G-protein complex breaks down. Depending on whether the G-proteins are stimulatory (activating) or inhibitory (inhibiting), a subunit is activated or inhibited enzymewho have favourited adenylyl cyclase. When activated, the cyclase produces cAMP; when inhibited, this reaction does not take place.
cAMP itself continues the signal cascade initiated by a hormone by stimulating another enzyme, protein kinase A (PKA). These Kinase is able to attach phosphate residues to substrates (phosphorylation) and in this way initiate activation or inhibition of downstream enzymes. Overall, the signal cascade is amplified many times over: a hormone molecule activates a cyclase, which - with a stimulatory effect - produces several cAMP molecules, each of which activates several protein kinases A.
This chain of reactions ends when the G-protein complex has broken down GTP to GDP as well as by enzymatic inactivation of the cAMP by phosphodiesterase. Substances changed by phosphate residues are freed from the attached phosphate with the help of phosphate phases and thus reach their original state.
The second messenger IP3 and DAG arise at the same time. Hormones that activate this pathway bind to a Gq protein-coupled receptor.
This G protein, which also consists of three subunits, activates the enzyme phospholipase after hormone receptor binding C-beta (PLC-beta), which cleaves IP3 and DAG from the cell membrane. IP3 works on the calcium stores of the cell by releasing the calcium it contains, which in turn initiates further reaction steps. DAG has an activating effect on the enzyme protein kinase C (PKC), which equips various substrates with phosphate residues. This chain of reactions is also characterized by a strengthening of the cascade. The end of this signal cascade is reached with the self-shutdown of the G-protein, the breakdown of IP3 and the help of phosphatases.
b) intracellular receptors:
Steroid hormones, Calcitriol and Thyroid hormones have receptors located in the cell (intracellular receptors).
The receptor of steroid hormones is in an inactivated form, as so-called Heat shock protein (HSP) are bound. After hormone binding, these HSPs are split off, so that the hormone-receptor complex in the cell nucleus (nucleus) can hike. There the reading of certain genes is made possible or prevented, so that the formation of proteins (gene products) is either activated or inhibited.
Calcitriol and Thyroid hormones bind to hormone receptors that are already in the cell nucleus and represent transcription factors. This means that they initiate gene reading and thus protein formation.
Hormonal control circuits and the hypothalamic-pituitary system

Hormones are integrated into so-called hormonal control circuitswhich control their formation and distribution. An important principle in this context is the negative feedback of the hormones. By feedback we mean that the hormone triggered answer (signal) the hormone-releasing cell (Signaling device) is reported back (feedback). Negative feedback means that when there is a signal, the signal transmitter releases fewer hormones and thus the hormonal chain is weakened.
Furthermore, the hormonal control loops also influence the size of the endocrine gland and thus adapt it to the requirements. It does this by regulating cell number and cell growth. If the number of cells increases, this is referred to as hyperplasia, while it decreases as hypoplasia. With increased cell growth, hypertrophy occurs, with cell shrinkage, however, hypotrophy.
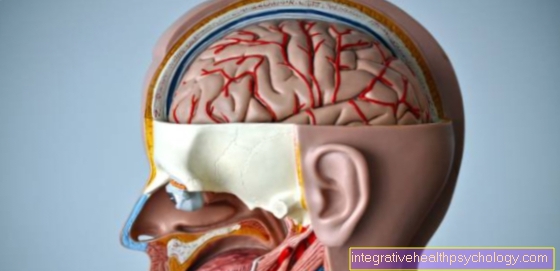
This presents an important hormonal control loop Hypothalamic-Pituitary System. The Hypothalamus represents part of the Brain represent that Pituitary gland is the Pituitary gland, which are in a Anterior lobe (Adenohypophysis) as well as one Posterior lobe (Neurohypophysis) is structured.
Nerve stimuli of the central nervous system reach the hypothalamus as a "switching point". This in turn unfolds through Liberine (Releasing hormones = releasing hormones) and statins (Release Inhibiting Hormones = Release-inhibiting hormones) its effect on the pituitary gland.
Liberins stimulate the release of pituitary hormones, statins inhibit them. As a result, hormones are released directly from the posterior lobe of the pituitary gland. The anterior pituitary lobe releases its messenger substances into the blood, which reach the peripheral end organ via the blood circulation, where the corresponding hormone is secreted. For each hormone there is a specific liberin, statin and pituitary hormone.
The posterior pituitary hormones are
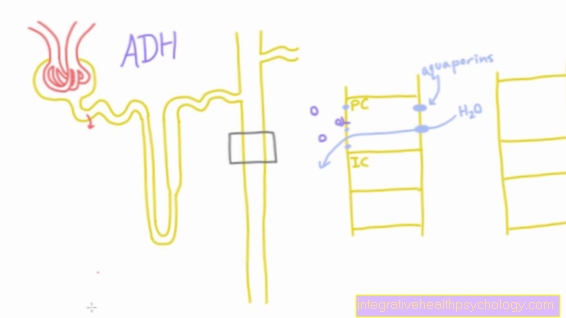
- ADH = antidiuretic hormone
- Oxytocin
The Liberine and Statins of the hypothalamus and the downstream hormones of the anterior hypophysis are:
- Gonadotropin releasing hormone (Gn-RH)? Follicle Stimulating Hormone (FSH) / Luteinizing Hormone (LH)
- Thyrotropin Releasing Hormones (TRH)? Prolactin / Thyroid Stimulating Hormones (TSH)
- Somatostatin ? inhibits prolactin / TSH / GH / ACTH
- Growth Hormone Releasing Hormones (GH-RH)? Growth hormone (GH)
- Corticotropin Releasing Hormones (CRH)? Adrenocorticotropic Hormone (ACTH)
- Dopamine ? inhibits Gn-RH / prolactin
The journey of the hormones begins in the Hypothalamuswhose liberins act on the pituitary gland. "Intermediate hormones" produced there reach the peripheral hormone formation site, which produces the "end hormones". Such peripheral sites of formation of hormones are, for example thyroid, the Ovaries or the Adrenal cortex. The “end hormones” include thyroid hormones T3 and T4, Estrogens or the Mineral corticoids the adrenal cortex.
In contrast to the route described, there are also hormones independent of this hypothalamus-pituitary axis, which are subject to other control loops. These include:
- Pancreatic hormones: Insulin, glucagon, somatostatin
- Kidney hormones: Calcitriol, erythropoietin
- Parathyroid hormones: Parathyroid hormone
- other thyroid hormones: Calcitonin
- Liver hormones: Angiotensin
- Adrenal medulla hormones: Adrenaline, noradrenaline (catecholamines)
- Adrenal cortex hormone: Aldosterone
- Gastrointestinal hormones
- Atriopeptin = atrial natriuretic hormone of the muscle cells of the atria
- Pineal melatonin (Epiphysis)
Thyroid hormones
The thyroid has the task of different amino acids (Protein building blocks) and the trace element iodine Produce hormones. These have a variety of effects on the body and are particularly necessary for normal growth, development and metabolism.
Thyroid hormones have an impact on almost all cells in the body and, for example, provide one Increase in heart strength, one normal bone metabolism for a stable skeleton and a sufficient heat generationto maintain body temperature.
At Children Thyroid hormones are especially important as they are for the Development of the nervous system and the Body growth (see also: Growth hormones) are required. As a result, if a child is born without a thyroid gland and is not treated with thyroid hormones, severe and irreversible mental and physical disabilities and deafness develop.
Triiodothyroxine T3
Of the two hormone forms produced by the thyroid gland, this represents T3 (Triiodothyronine) is the most effective form. It arises from the other and mainly formed thyroid hormone T4 (Tetraiodothyronine or thyroxine) by splitting off an iodine atom. This conversion is done by Enzymesthat the body makes in the tissues where the thyroid hormones are needed. A high enzyme concentration ensures a conversion of the less effective T4 into the more active form T3.
Tyroxine T4
The Tetraiodothyronine (T4), which is usually called Thyroxine is the most commonly produced form of the thyroid gland. It is very stable and can therefore be transported well in the blood. However, it is clear less effective than the T3 (Tetraiodothyronine). It is converted into this by splitting off an iodine atom using special enzymes.
For example, if thyroid hormones are due to a Subfunction usually have to be replaced Thyroxine or T4 preparations, as these do not break down so quickly in the blood and individual tissues can be activated as required. Thyroxine can also act directly on the cells like the other thyroid hormone (T3). However, the effect is significantly less.
Calcitonin
Calcitonin is made by cells in the thyroid (so-called C cells), but it is not actually a thyroid hormone. It differs significantly from these in its task. In contrast to T3 and T4 with their diverse effects on all possible body functions, calcitonin is only for the Calcium metabolism responsible.
It is released when calcium levels are high and ensures that it is lowered. The hormone does this, for example, by inhibiting the activity of cells that release calcium by breaking down bone substance. In the Kidneys Calcitonin also provides a increased excretion of calcium. in the Intestines it inhibits the uptake of the Trace element from food into the blood.
Calcitonin has one Opponent with opposite functions that lead to an increase in calcium levels. It's about that Parathyroid hormonemade by the parathyroid glands. Together with the Vitamin D the two hormones regulate the calcium level. A constant calcium level is very important for many body functions such as the activity of the muscles.
Calcitonin plays a further role in very special cases Diagnosis of thyroid diseases to. In a certain form of thyroid cancer, the calcitonin level is extremely high and the hormone can act as a Tumor markers serve. If the thyroid gland has been removed by surgery in a patient with thyroid cancer and a follow-up examination reveals significantly increased calcitonin levels, then this is an indication of cancer cells still remaining in the body.
Adrenal hormones
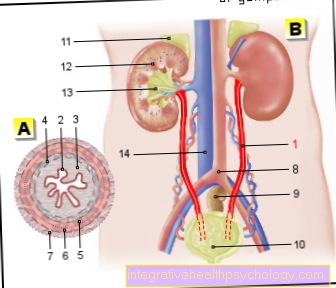
The adrenal glands are two small, hormone-producing organs (so-called endocrine organs), which owe their name to their location next to the right or left kidney. There, various messenger substances with different functions for the body are produced and released into the blood.
Mineralocorticoids
The so-called mineral corticoids are an important type of hormone. The main representative is that Aldosterone. It mainly acts on the kidney and is there to regulate the Salt balance significantly involved. It leads to a decreased delivery of sodium via the urine and, in turn, an increased excretion of potassium. Since water follows sodium, the aldosterone effects accordingly more water saved in the body.
A deficiency in mineral corticosteroids, for example in an adrenal gland disease like this Addison's disease, accordingly leads to high potassium and low sodium levels and low blood pressure. The consequences can include Circulatory collapse and Arrhythmia be. Hormone replacement therapy then has to take place, for example with tablets.
Glucocorticoids
Among other things, the so-called glucocorticoids are formed in the adrenal glands (Other names: corticosterody, cortisone derivatives). These hormones have an impact on almost all cells and organs in the body and increase willingness and ability to perform. For example, they raise the Blood sugar level by stimulating sugar production in the liver. They also have one anti-inflammatory effect, which is used in the therapy of many diseases.
Be used in the treatment of asthma, skin diseases or inflammatory bowel disease, for example man-made Glucocorticoids used. These are mostly Cortisone or chemical modifications of this hormone (for example Prednisolone or budesonide).
If the body is one too large amount exposure to glucocorticoids can cause adverse effects such as osteoporosis (Loss of bone substance), high blood pressure and Fat storage on the head and trunk. Excessive hormone levels can occur when the body produces too many glucocorticoids, as is the case with the disease Cushing's disease. More often, however, an oversupply is caused by treatment with cortisone or similar substances over a longer period of time. However, the side effects may be accepted if the benefits outweigh the treatment. With a short-term Corstison therapy usually no side effects are to be feared.
Hormone related diseases
In principle, any disorders of the hormone metabolism can occur Endocrine gland affect. These disorders are referred to as endocrinopathies and usually manifest themselves as over- or under-functioning of the hormonal glands of various causes.
As a result of the dysfunction, the hormone production increases or decreases, which in turn is responsible for the development of the clinical picture. An insensitivity of the target cells to the hormones is also a possible cause of an endocrinopathy.
Insulin: An important clinical picture related to the hormone insulin is Diabetes mellitus (Diabetes). The cause of this disease is a deficiency or insensitivity of the cells to the hormone insulin. As a result there are changes in the glucose, protein and fat metabolism, which in the long term cause severe changes in the blood vessels (Microangiopathy), Nerves (polyneuropathy) or wound healing. Affected organs are among others kidney, heart, eye and brain. The damage caused by diabetes manifests itself in the kidneys as so-called diabetic nephropathy, which is caused by microangiopathic changes.
In the eyes, diabetes occurs as diabetic retinopathy to days, being changes in the Retina (retina), which are also caused by microangiopathy.
Diabetes mellitus is treated with insulin or medication (oral antidiabetic agents).
As a result of this therapy, overdose of insulin occur, which causes discomfort in both diabetics and healthy people. Also an insulin-producing tumor (Insulinoma) can cause an overdose of this hormone. The consequence of this excess insulin is, on the one hand, a decrease in blood sugar (Hypoglycemia), on the other hand a decrease in the potassium level (hypokalaemia). Hypoglycemia manifests as hunger, tremors, nervousness, sweating, palpitations, and an increase in blood pressure.
In addition, there is reduced cognitive performance and even loss of consciousness. Since the brain relies on glucose as the only source of energy, long-term hypoglycemia results in damage to the brain. H
ypokalemia caused as a second consequence of insulin overdose Arrhythmia.



.jpg)