Vaccinate
Synonyms in the broadest sense
Immunization, vaccine
English: immunization, immunization, vaccination
definition
Vaccinations are there to protect the human organism from disease by preparing it for it. This is done with the help of weakened pathogens or ready-made antibodies that are injected.

introduction
Childhood vaccinations are still controversial today. Vaccination is important, but in addition to the obvious benefits, it also has undesirable side effects. To protect a child from seemingly harmless diseases (e.g. chicken pox) and more obvious dangerous diseases (e.g. diphtheria), there are a number of vaccinations available today.
You may also be interested in this topic: Why you should vaccinate
Why should you have your child vaccinated?
Vaccination is still very important today. Your child is thus protected against diseases that can have unpleasant and devastating consequences through a vaccination.
Even if a disease such as chickenpox sounds harmless, children can suffer complications such as - in the worst case pneumonia or meningitis - which can even be fatal. These complications are certainly rare, but still more common than the vaccine damage often feared by parents.
You might also be interested in this in this context: Vaccination against meningitis
In Germany, compulsory vaccinations have been abolished. Parents are therefore responsible for whether or not their children are vaccinated. Nowadays, many parents can no longer imagine that diseases like polio still exist. Indeed, in Europe, thanks to the high vaccination rates of the population, such diseases are almost eradicated. If you have the attitude that you don't have to vaccinate your child because of that, you unfortunately contribute to the fact that these illnesses increase again without vaccination.
For example, tuberculosis from the eastern countries is on the rise again. Once we get here, this can mean major problems, as in Germany, for example, children are no longer vaccinated against tuberculosis, so they can become infected with this dangerous disease.
Many parents worry about their children when it comes to vaccination. Many fear that their child could retain permanent damage. It should be said that in Germany there is no vaccine officially approved by the STIKO in which permanent damage could be reliably proven.
If you are wondering whether vaccination makes sense, read: Should I get my baby vaccinated?
Recommended vaccinations for the baby
The vaccination recommendations are issued by the STIKO (permanent vaccination committee of the Robert Koch Institute). Pediatricians advise parents on necessary and useful vaccinations according to this scheme.
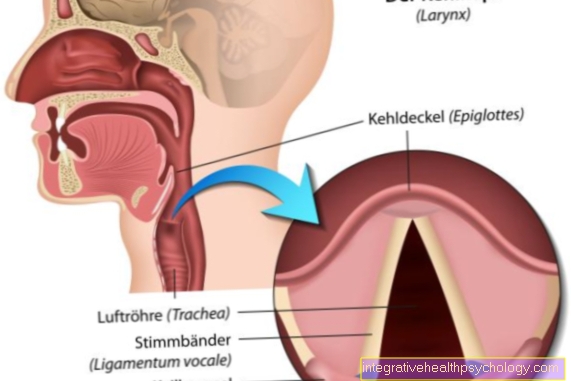
According to the STIKO vaccination calendar, vaccinations for babies start at 1.5 months with an oral vaccination against rotaviruses.At the age of 2 to 15 months, vaccinations are given against Tetatnus, Polio (polio), pertussis (whooping cough), diphtheria, as well as hemophilus influenza, the causative agent of epiglottitis, hepatitis B (chronic inflammation of the liver) and pneumococci, the cause of pneumonia.
These vaccinations are carried out four times up to the age of 15 months.
There will also be further vaccinations against rotaviruses. Booster vaccinations follow in childhood and adolescence.
You can find detailed information at: Vaccinations in the baby
Infanrix / 6-fold vaccination
The 6-fold vaccination Infanrix®, also called Infanrix hexa, protects against six different infectious diseases. These include poliomyelitis (polio), diphtheria (a condition that can cause severe throat infections and shortness of breath), tetanus (tetanus), pertussis (whooping cough), hepatitis B (a chronic inflammation of the liver that can lead to liver failure), and Infections with the bacterium Haemophilus influenza type B (a bacterium which can cause meningitis and severe laryngitis).
The vaccination is usually carried out after the second, third and fourth month of life. Another vaccination dose will follow six months later. After the vaccination, the injection site may appear temporarily red and swollen.
Other common side effects of Infanrix hexa are:
- fever
- Loss of appetite
- Restlessness
- irritability
- diarrhea
- and vomiting.
All listed side effects disappear completely within a few days. Infanrix hexa is one of the recommended vaccinations for children. The price for the vaccination is therefore covered by all health insurance companies.
Also read our main article: Infanrix
Vaccination against whooping cough
It is recommended to vaccinate everyone against whooping cough. According to the vaccination calendar, children are vaccinated against whooping cough together with other infectious diseases by the pediatrician for the first time after they are two months old. Then 3 more vaccinations take place after the 3rd month of life, the 4th month of life and the 11th to 14th month of life.
Booster vaccinations are given between the ages of 5 and 6 and 9-17. Age. A booster vaccination is given once in adulthood. There should be at least 10 years between the vaccination and the last vaccination in childhood. If vaccinations are missed, they can be made up - even in adulthood.
Unlike the vaccination against tetanus and diphtheria, the booster vaccination against whooping cough is only given once in adult life. The booster vaccination in adulthood ensures immunity to whooping cough of the vaccinated person and prevents the transmission of the disease to other people.
Vaccination against whooping cough is especially important in adults who have a lot to do with children. This applies particularly to kindergartens, pediatric nurses, child minders, KiTA staff, etc. Since the infection in adults can look like the flu and the infection with whooping cough can be overlooked, it can be transmitted to children or newborns who cannot be vaccinated.
You can read more about this topic at: Vaccination against whooping cough
Vaccination against polio
Polio, also known as poliomyelitis, is a serious viral disease that in rare cases can lead to permanent flaccid paralysis.
Today Europe is considered polio-free, but there are always polio cases in other regions of the world. The vaccination against polio is included in the six-fold vaccine Infanrix hexa®, which is administered after the second, third and fourth month of life. A fourth vaccination takes place between the ages of 11 and 14 months. Fever often occurs as a temporary vaccination reaction. Swelling and reddening of the injection site and flu-like symptoms can also be observed. All symptoms disappear completely after a few days.
Are you interested in this topic? Read detailed information at: Vaccination against polio
Measles vaccination
Nowadays the measles vaccination is part of the basic immunization for babies from the age of 12 months. As the measles continues to exist and in rare cases it becomes the fatal complication of the subacute scleorizing panencephalitis With brain destruction, vaccination is also recommended for adults.
This mainly affects all people who were born after 1970 and have no vaccination or an unclear vaccination status.
Since a measles infection during pregnancy can lead to abortion or malformations in the child, women in particular should be vaccinated before pregnancy if the vaccination status is not clear.
Since the measles vaccination is a live vaccine with weakened pathogens, a new booster vaccination is not necessary.
Read more about this under Vaccination against measles
Vaccination against rotavirus
The vaccination against rotaviruses takes place after 1½, 2 and 3 months by oral vaccination. The vaccine should be given approximately every four weeks. The rotavirus vaccination is a live vaccine. That is, the weakened pathogen will be vaccinated, which will cause the immune system to make antibodies against the virus.
The rotavirus is very common and causes severe vomiting and diarrhea in both children and adults. As this can be dangerous for children and the elderly, vaccination against rotaviruses should be carried out.
You can find a lot more information under our topic: Vaccinate against the rotavirus
The vaccination calendar provides information
Parents often wonder when to vaccinate their child against which disease. The so-called vaccination calendar provides information here. All recommended child vaccinations are listed here with the recommended vaccination age. The vaccination calendar is published by the permanent vaccination committee (STIKO) of the Robert Koch Institute for Infectious Diseases and is constantly revised. Vaccinations relating to stays abroad are not specified here. Indicated vaccinations, such as TBE (early summer meningoencephalitis), are also not included. The following is a calendar based on the vaccinations recommended by STIKO:
Vaccination calendar
- tetanus
- 2 months (1st vaccination)
- 3 months (2nd vaccination)
- 4 months (3rd vaccination)
- 11-14 months (4th vaccination)
- 5-6 years (1st refresher)
- 9-17 years (2nd refresher)
- Diptheria
- see tetanus
- whooping cough
- see tetanus
- Hib
- see tetanus (without refresher)
- polio
- see tetanus (only 2nd refresher)
- Hepatitis B.
- see tetanus (without refresher)
- Pneumococci
- 2 months (1st vaccination)
- 4 months (2nd vaccination)
- 11-14 months (3rd vaccination)
- Meningococci
- 11-14 months
- MMR (measles, mumps, rubella)
- 11-14 months (1st vaccination)
- 15-23 months (2nd vaccination)
- chickenpox
- 11-14 months (1st vaccination)
- (possibly 15-23 months (2nd vaccination))
- Rotaviruses
- 1.5 months (1st vaccination)
- 2 months (2nd vaccination)
- possibly 3 months (3rd vaccination)
- Human papillomavirus
- 9-14 years (1st vaccination)
- 9-14 years, 5 months after the 1st vaccination (2nd vaccination)
- if the vaccination is> 14 years old, three vaccinations must be given
This calendar is only intended to be a guide and is by no means to be seen as the ultimate solution. Special situations require different vaccination procedures. For example, if a child has an HIV infection, which is very common in Africa, the vaccination indication must of course be made individually.
What types of vaccination are there?
When it comes to vaccinations, a distinction must be made between what is known as passive vaccination and active vaccination / immunization.
- Active immunization / vaccination
In active vaccination, weakened pathogens or components of the pathogen are injected so that the body's immune system makes antibodies against this pathogen in response.
This has the disadvantage that several doses of the vaccine are often required for the final vaccination.
An example of this is the Hepatitis A vaccination and hepatitis B vaccination: There are 3 vaccinations at intervals of 4 or 12 weeks. Since the pathogens occur in a weakened form, there is almost no risk of getting the actual infection. If an infection does occur, it is usually present to a lesser extent. Unfortunately there is the possibility of vaccination damage. The patient or his parents will be informed about this risk before the vaccination! - Passive immunization / vaccination
In the case of passive vaccination, the principle is different: Here the antibodies (Immunoglobulins), i.e. the antibodies against a disease, are injected. If the person comes into contact with a sick person, the immune system of the vaccinated person already has the antibodies to immediately “drive away” the pathogens. With this type of vaccination, the result usually lasts shorter than that of active vaccination. The advantage of this vaccination, however, is that this type of vaccination can be used very well for short-term vaccinations (for example before traveling). This does not only apply to children, but also as an adult, one should take care of the required or recommended vaccinations before going abroad outside of Europe.
In order to save the children multiple vaccinations, there are so-called combination vaccines that protect against several diseases at the same time. (Example: six-fold vaccination: Tetanus, diphtheria, whooping cough, poliomyelitis , Hepatitis A and B and Hib (Haemophilus influenza b)).
Since the pathogens contained in the vaccines, despite their weakened form, challenge the body's defense system, the child should not be seriously ill. Contrary to popular belief, smaller infections, such as a runny nose, have no influence on the success of the vaccination.
You might also be interested in the topic: Vaccinations for adults
What is a live vaccination?
With a live vaccination, the vaccination contains a small amount of live pathogens. However, the pathogens are so weakened that an outbreak of the disease is extremely unlikely. The immune system recognizes the pathogen as foreign and can form antibodies against it.
When contact is made again, the immune system is prepared and the disease does not break out.
Live vaccinations are for example:
- measles
- mumps
- rubella
- chickenpox
- Rotaviruses
In rare cases, the pathogens contained in the vaccine can trigger a mild vaccine disease, for example the so-called vaccine measles. A non-contagious rash similar to the measles rash may appear a few weeks after the vaccination. As a rule, people with immunodeficiency should not receive any live vaccinations.
Further information on this topic can be found at: Live vaccination
What is a dead vaccination?
In the case of a dead vaccination, the vaccination contains only killed pathogens or even only components of the pathogen, for example parts of the shell or capsule. These are sufficient for the immune system to form antibodies that protect against the respective disease. Most of the vaccines available on the market are dead vaccines; including the six-fold vaccine against poliomyelitis, whooping cough, diphtheria, hemophilus influeza type B, hepatitis B and tetanus.
Side effects of vaccinations
Pain after vaccination
The pain after vaccination is one of the general and natural reactions to vaccination.
The vaccination is given into the muscle with a needle. This leads to irritation of the muscle and the surrounding tissue. The pain is exacerbated if the muscle is tensed during the injection, which makes it harder for the needle to penetrate the muscle and thus requires more pressure.
The pain after a vaccination usually appears like sore muscles at the injection site. This pain should subside after one or two days; if the pain is severe, the injection site should be cooled.
If the pain gets worse, or if the puncture site swells, is reddened or overheated, a doctor should be consulted. This could be an infection at the injection site.
You can find a lot more information under our topic: Pain after vaccination
Fever after vaccination
The fever that can develop after a vaccination is also one of the possible vaccination reactions that can occur after a vaccination. These vaccine reactions include fever, reddening of the injection site and muscle pain (compared to aching muscles) as well as flu-like symptoms. Usually these reactions occur within 72 hours of vaccination and should not last longer than 1-2 days.
If the fever has persisted for several days, the injection site is swollen and overheated, or if you feel very sick, you should see a doctor.
For more information, see: Side effects from vaccinations
These vaccine reactions are the result of an immune response to the vaccine, which is necessary to obtain vaccination protection.
Most vaccines produce antibodies to the administered vaccine, which are essential for immunity to the vaccinated disease. If pathogens get into the body after a successful basic vaccination (depending on the vaccine after a few vaccine doses), these are recognized by the antibodies that were previously formed and eliminated immediately. This prevents the disease from breaking out.
Cold leg compresses are available as home remedies to lower the fever. It is important to always maintain adequate hydration. However, if the temperature rises despite the calf wrap, drug therapy should be started to lower the fever. Paracetamol and ibuprofen are available here. Aspirin also has a fever-lowering effect, but aspirin must never be used in children.
Also read: Fever in the baby after vaccination
What are vaccine damage?
Damage caused by a vaccination is a serious, sometimes permanent damage to health that goes beyond the normal vaccination reaction - fever, tiredness, pain at and around the injection site - as a result of a vaccination. In the event of a vaccination damage, it is important whether the vaccination is recommended by the STIKO (permanent vaccination commission). Fortunately, serious damage from a vaccination is rare, but should be reported to the welfare office immediately. They can also appear weeks, months or years after the vaccination.
There are recognized vaccination damages for certain vaccinations. Here are a few examples:
- Reactions such as febrile seizures and allergic reactions are recognized for all vaccines.
- Tetanus diphtheria: Guillain-Barré syndrome (damage to the peripheral nerves)
- Mumps, measles and rubella: decrease in red blood cells
- Whooping cough: meningitis
- Flu: Guillain-Barré Syndrome
Before a vaccine is approved, of course, its safety is checked using standardized procedures of the European and national approval authorities.
The vaccination reactions must be clearly distinguished from the vaccine damage. These often occur after a vaccination, but are harmless and go quickly (usually within 2 days) back again. After all, the vaccination is supposed to cause a reaction in the body. This reaction is then expressed in the so-called reaction of the vaccination, which can be differently strong or weak from child to child. These include, for example:
- Reddening of the puncture site
- Injection site pain
- Fever (rare)
For more information on side effects after vaccinations, see: Side effects from vaccinations in the baby or vaccination side effects
When can or should not be vaccinated?
If your child is seriously ill, he should be spared further suffering and should not be vaccinated. The already weakened immune system might be overwhelmed.
Unfortunately, it is often the case that children who cannot be vaccinated because of their health condition are precisely those children who absolutely need a vaccination. This particularly affects children with immune deficiencies.
Vaccination with a live vaccine should not be given if:
- the child suffers from a severe immune deficiency (B or T cell defect)
- your child has previously received a blood transfusion
- You are pregnant and can be switched to an alternative preparation (If you want to know more about medication during pregnancy, read our topic: Medication during pregnancy)
- the vaccine has caused an allergic reaction in your child
In adults, the immune system should not already be weakened by an infection or other illness at the time of vaccination.Some vaccines also do not work when antibiotics are taken at the same time.
Which situations are vaccine-specific harmless?
Contrary to the popular opinion of many parents who are very concerned about vaccinations, the child can definitely be vaccinated if they have a cold. Here are a few more situations in which parents usually worry for no reason:
- mild runny nose or diarrhea
- Premature birth: they need protection from potentially dangerous diseases even more
- Even if you are breastfeeding your child (see breastfeeding), a vaccination can be carried out and is in no way "superfluous"
- Child's allergies
- Congenital heart defects: these children also urgently need vaccination protection in order not to unnecessarily burden the already damaged heart with an illness
None of the above and many more do not limit your child's ability to vaccinate.
Other important vaccinations
Typhoid vaccination
Typhus is an infectious disease caused by the bacterium Salmonella typhi. Symptoms are:
- stomach pain
- nausea
- severe diarrhea
- and fever.
In rare cases, intestinal perforations (perforations) can occur. Typhoid bacteria are found in contaminated food and in stale water. That is why particular caution is required when choosing food and drinks in risk areas.
Oral vaccine and muscle-administered vaccine are available for typhoid fever. Both show an effectiveness of 50-80%.
The oral vaccination is taken on the first, third and fifth day and offers protection against typhoid infection for about a year. However, the vaccination is ineffective if antibiotics or malaria prophylaxis are taken at the same time.
The vaccination given by injection into the muscle only needs to be given once. The protective effect then lasts for about three years. It is reported that this form of vaccination has slightly more side effects than oral vaccination. For example, fever is more common. In general, however, both forms of vaccination have few side effects.
Read more on the topic: Typhoid vaccination
Hepatitis vaccination
There is a vaccination for hepatitis B and hepatitis A. In addition to these two forms of hepatitis, there is also hepatitis C, D and E. No vaccinations are available for these three forms. The most important vaccination, which is given in childhood, is hepatitis B. Hepatitis is an inflammation of the liver, which varies depending on the pathogen.
Hepatitis B is usually chronic and ends in cirrhosis of the liver. Hepatitis B is transmitted through body fluids. The most important carrier is blood, followed by sperm and cervical mucus, and saliva. To avoid transmission, all available vaccinations against hepatitis should be obtained.
The hepatitis vaccination takes place for the first time at the age of 2 months and consists of four vaccinations up to the age of fifteen. Then the basic immunization is completed. Booster vaccinations are given between the ages of five and six and then between the ages of 9 and 17. Afterwards, the vaccination titer (antibodies against hepatitis B) should be determined regularly. If the titer falls below 1000, the vaccination should be refreshed.
Hepatitis A can be vaccinated in people who are at increased risk of infection. These include pediatric nurses and paediatricians. People who travel to certain areas should also be vaccinated. Hepatitis A occurs in countries with poor hygiene. It is transmitted faecal-orally, so it can be ingested through food. This concerns any kind of food, as the germs are transferred to the food during the preparation of food due to insufficient hand hygiene.
For more information, see:
- Hepatitis A vaccination
- Hepatitis B vaccination
Twinrix
Twinrix is the name of a combination vaccine against the two viral diseases hepatitis A and B. Both diseases can cause severe liver inflammation, which in the case of hepatitis B can often become chronic and lead to liver failure. Vaccination with Twinrix is usually only indicated for groups of people who are particularly at risk. In addition to medical staff, this also includes travelers to various countries (for example the Mediterranean region).
The basic vaccination consists of three vaccinations: the first vaccination is followed by the second dose one month later and the third dose six months later. The most common side effects include a local reaction at the injection site, as well as headache, nausea and loss of appetite.
You can find detailed information at: Twinrix
Vaccination against pneumonia
Pneumococci are among the most common pathogens causing pneumonia. In addition to pneumonia, they also cause meningitis and otitis media.
Vaccination against these bacteria is recommended for children from the age of two months and for older people from the age of 60. Babies are vaccinated after the age of two, four and around 11-14 months. Subsequently, if the immune system is normal, no further refreshment is necessary. Older people from the age of 60 are vaccinated once. A refresher after six years at the earliest is only necessary under certain circumstances.
Immunocompromised people and people at risk can receive a booster vaccination every six years even before the age of 60.
You can find more information on the topic here: Vaccination against pneumonia
Vaccination against meningococci
Meningococcal vaccination exists against serotype C. This is the most common type of meningococcal. Meningococci are the causative agents of meningitis (meningitis). This is an acutely life-threatening illness that is associated with a high fever, severe headache, vomiting and stiff neck. In the advanced stage, the disease leads to a clouding of consciousness and, without treatment, death within a few hours to days.
Since meningococcal infection is highly contagious, anyone who has come into contact with an infected person should take an antibiotic prophylactically. Meningococcal vaccination is permitted from the age of one year.
You might also be interested in: Vaccination against inflammation of the skin
HPV vaccination / vaccination against cervical cancer
HPV (Human Papilloma Virus) is a virus that can cause cancer of the cervix, but also of the anus, the oral cavity and the penis. An infection can also lead to genital warts.
Vaccination against some high-risk types of the virus (especially HPV 16 and 18) has been recommended for girls since 2007 and for boys since 2018. Basic vaccination takes place in two or three individual doses, depending on age. The age recommendation for the vaccination is now 9 to 17 years.
However, vaccination should be given before the first sexual contact, as the viruses are most often transmitted this way. Side effects usually only occur in the form of pain and redness in the area of the injection site. Headache and muscle pain, a slight fever and nausea are less common. The costs of the HPV vaccination are covered by the health insurance for girls up to 17 years of age. Many health insurers already cover the cost of vaccinating boys.
Read more on this topic at: Vaccination against cervical cancer
Vaccinations for different travel destinations
What vaccinations are recommended for Thailand?
For Thailand the following vaccinations are recommended regardless of the local risk:
- tetanus
- diphtheria
- Hepatitis A
- rabies
In addition, it is important to pay attention to how the accommodation takes place on site, whether there is contact with locals or animals, how long the stay is planned and what time of the year you travel. This also results in the following vaccinations:
- Hepatitis B.
- Typhus (if there is a lack of hygiene),
- Polio (for stays away from civilization, for longer stays and for hygiene deficiencies),
- Measles (only in children),
- Japanese encephalitis (for long stays and for stays away from civilization).
In general, care should be taken in Thailand not to touch wild animals and their excrements. Sufficient mosquito protection should also be ensured in order to avoid diseases such as dengue fever and the Zika virus as far as possible.
Malaria prophylaxis is also recommended. In order to get adequate advice prior to a stay in Thailand, travelers should ask their family doctor or a tropical medicine specialist for travel vaccination advice.
Vaccination against Japanese encephalitis
Japanese encephalitis is a viral disease that is mainly transmitted via mosquitoes.
It occurs in the Asian region and in northern Queensland (Australia) mainly in rural regions. The Ixiaro® vaccine protects against the disease, but can only be administered by doctors trained in tropical medicine.
The vaccination takes place twice at an interval of four weeks. How long the vaccination protection lasts has not yet been investigated. Under certain circumstances, a refresher can take place after 12-24 months.
Common side effects are local reactions such as redness and swelling at the injection site. In addition, flu-like symptoms, headache and muscle pain, and fever can occur. Travel vaccination advice is recommended for people planning to travel to the above regions.
Read detailed information on this topic: Japanese encephalitis
Vaccination against dengue fever
Dengue fever is a mosquito-borne infectious disease. It occurs in tropical and subtropical regions of the world. This includes parts of Africa, Central and South America, as well as South and Southeast Asia. Symptoms of dengue fever are:
- Fever attacks,
- severe muscle pain,
- occasionally with a rash.
Severe forms of disease that can potentially be fatal are rare. A vaccination against dengue fever has been available since 2017. However, this is only administered to locals, because tourists hardly run the risk of developing severe forms of the disease, as these practically never occur during the initial infection. Tourists are therefore advised to use insect repellants and mosquito nets in particular.
You can find further information on this topic at: dengue fever
Yellow fever vaccination
Yellow fever is a serious infectious disease that occurs in parts of Africa near the equator and in Central and South America. It is transmitted via mosquitoes and leads to:
- severe fever,
- Nausea,
- Vomit,
- Body aches
- and yellowing of the skin and eyes.
The vaccination against yellow fever is a live vaccination and may only be carried out by doctors who are active in tropical medicine. The basic immunization consists of just one dose of vaccination, which must be carried out at least 10 days before the stay abroad. Some affected countries require proof of the vaccination carried out upon entry. The vaccination has few side effects. Nevertheless, local reactions at the injection site and mild flu-like symptoms can occur.
Read more detailed information at: Yellow fever vaccination
TBE vaccination
TBE (early summer meningo encephalitis) is a viral disease that is transmitted by ticks. Those affected often only suffer from:
- fever
- a headache
- and dizziness,
Signs of meningitis or meningitis are also less common:
- Neck stiffness,
- strongest headache,
- Confusion,
- Drowsiness
In Germany, the disease occurs mainly in Bavaria and Baden-Württemberg. Primary vaccination requires three doses of vaccine. The second vaccination follows 1-3 months after the first. The third is given 5-12 months later. Booster vaccinations are given about every 3-5 years, depending on the vaccine used. The vaccination has few side effects; The most common vaccine reactions include redness, swelling and pain around the injection site.
Read more on the topic: Vaccination against TBE
What is the STIKO?
STIKO stands for the permanent vaccination committee of the Robert Koch Institute for Infectious Diseases. Its members are medical professionals who work in various fields. The pediatrician and the occupational physician work hand in hand here. None of the doctors are paid for membership in the STIKO. The office is an honorary post. This removes doubts about the credibility, because no member has any personal benefit from vaccination recommendations. Not only medical professionals are represented in the STIKO, there is also close cooperation with the manufacturers of vaccines. The STIKO has the task of thinking about vaccines and their benefits or side effects and then making an official recommendation based on studies. If vaccines are recommended by the STIKO, they are considered safe and harmless.