Cardiomyopathy
Synonyms
Heart muscle disease, cardiomyopathy (English)
introduction
The Cardiomyopathy One of the heart muscle diseases is not necessarily an undersupply of the heart with blood, valve defects or a Pericarditis underlying. In the Cardiomyopathy is primarily the Heart muscle damaged and as a result, it can lead to a functional impairment of the heart. The functional restriction is mostly the result of a structural change in the heart, during which the heart enlarges and thus cannot contract enough to ensure sufficient ejection.
The heart can also thicken, which means that not enough blood can flow into the heart chamber. The result of one or both of these structural changes can be so-called heart failure, in which the pumped amount of blood is not sufficient to adequately supply the organs. In particular, suffer from this brain and the lungs.
The WHO (World Health Organization) distinguishes 5 types of cardiomyopathy. The hypertrophic obstructive cardiomyobathy (HOCM) that restrictive cardiomyopathy (RCM), the dilated cardiomyopathy (DCM), the right ventricular (right ventricle) Cardiomyopathy and the cardiomyopathies for which the cause is reported as unknown or unclassified. There is also a difference primary from secondary Cardiomyopathies. Primary cardiomyopathies are diseases that take place exclusively in the heart muscle, while secondary cardiomyopathies can be the result of an existing disease.
The hypertrophic obstructive cardiomyopathy is a disease of the heart muscle in which the muscles of the left ventricle thicken (hypertrophy), especially the ventricular partition (ventricular septum). Since the outflow path of the left ventricle is also located here, there is an obstruction to the outflow due to the increased muscle mass. This outflow disorder can ultimately produce clinical symptoms.
In the restrictive cardiomyopathy the muscle tissue is stiffened and thus prevents the heart from filling up enough with blood during the relaxation phase. The actual pumping function is not disturbed here. In this case, the heart only lacks the necessary blood volume.
The dilated cardiomyopathy is a disease of the heart muscle in which the left, right or both chambers of the heart expand. Due to the pathological expansion of the heart chambers, the heart cannot contract effectively enough to allow the blood to flow into the Body circulation to transport.
The right ventricular cardiomyopathy is characterized by a breakdown of muscle cells in the right ventricle. These are then gradually replaced by fat cells and / or connective tissue cells, which means that the heart loses important functional muscle cells.
Unclassified cardiomyopathies include heart muscle diseases that occur very rarely and are difficult to distinguish from the more common cardiomyopathies.
Frequency of cardiomyopathy
The most common cardiomyopathy is dilated cardiomyopathy. It has a prevalence, i.e. an occurrence, of 40 cases per 100,000 inhabitants.
Men get sick twice more often than women. The disease can occur at any age, but the age peak is mainly between the ages of 20 and 50. The prevalence of hypertrophic obstructive cardiomyopathy is very low, around 0.2% of the population.
The rarest form of cardiomyopathy in the western world is the restrictive form. In tropical countries, however, it can account for up to 25% of cardiac muscle diseases, which essentially depends on the number of pericardial diseases. Right ventricular cardiomyopathy mostly affects young men and has a prevalence of 1 in 10,000 cases. It also accounts for about 10-20% of sudden cardiac death and is geographically concentrated in Italy. The number of unclassified cardiomyopathies is extremely rare.
history
Cardiomyopathy was referred to as such relatively late. In the 18th century it was initially only chronic Myocarditis known until around 1900 when the term primary heart muscle disease was established in medicine. In 1957 the term cardiomyopathy appeared for the first time. In the 1980s, cardiomyopathy was defined as a heart disease of unknown cause, and finally in 1995 the WHO expanded the definition to include cardiac muscle diseases that lead to malfunction of the heart.
Symptoms of cardiomyopathy
The symptoms of cardiomyopathy can be derived from their respective functional impairment. The main symptoms include shortness of breath, signs of fatigue, short-term loss of consciousness, water in the lung and Chest pain. Here the individual symptoms cannot necessarily be assigned to a specific form of cardiomyopathy, since the different mechanisms often lead to a similar clinical picture. Shortness of breath and reduced stress are the main complaints with which a patient visits his doctor.
The chest pain comes for example with the hypertrophic cardiomyopathy often because the body does not manage to supply the increased heart mass with additional oxygen under stress. The shortness of breath is caused by a backlog of blood in the lungs. The heart here no longer has the strength to pump the blood away from the lungs, and the liquid part of the blood can pass into the lungs. This ultimately prevents oxygen from being transported and can also lead to water in the lungs (Pulmonary edema).
Causes of cardiomyopathy

The causes of the various cardiomyopathies are diverse and can be assigned to different disease mechanisms.
These include, for example, genetic causes, bacterial / viral pathogens and systemic diseases. The dilated Cardiomyopathy can be converted into a primary and a secondary Divide shape.
In the primary form, the disease starts directly from the heart muscle itself and accounts for around 10% of all cases of dilated cardiomyopathy.
The secondary form of dilated cardiomyopathy can be divided into 3 other main causes, each accounting for about 30% of the secondary forms. The familial causes are based on a genetic defect, whereby the genetic information that ensures that important cardiac muscle proteins are created is faulty. These are particularly important for developing the strength of the heart muscle. Inflammatory processes also play an important role, as bacteria and / or viruses can damage the heart muscle here. In addition, the body can also use its own proteins (antibody) damage the heart muscle.
A so-called autoimmune disease would then be present here. Toxic damage also accounts for 30% of the secondary causes. alcohol seems to play a leading role and has established itself as the main cause, especially in the industrialized countries.
Hypertrophic cardiomyopathy is a heritable disease and positive family cases can be detected in around 50% of cases. Meanwhile, 10 gene locations and over 100 different mutation sites for the cause of the cardiomyopathy can be detected, which can lead to a hypertrophic cardiomyopathy. As mentioned above, restrictive cardiomyopathy occurs more in the tropical regions of the world and can also be divided into primary and secondary forms.
The primary form causes a connective tissue remodeling of the heart muscles, which leads to the heart stiffening and no longer working properly. This is where Löffler's endocarditis plays (Spoonbill pericarditis) plays a very important role. It begins with an inflammation of the heart and ends in a stiff, impaired heart.
The secondary form is mostly caused by so-called storage diseases. Storage diseases occur when a substance increasingly remains in the body or cannot be broken down. These substances can be deposited anywhere and thus lead to the functional impairment of the respective organ. Storage diseases that lead in particular to a restrictive cardiomyopathy are amyloidosis, sarcoid and various fat and sugar storage diseases.
Right ventricular cardiomyopathy is a genetically inherited disease and can often be confirmed in isolated cases in the family. The unclassified cardiomyopathies are usually also based on a genetic defect.
diagnosis

The diagnosis of cardiomyopathy is made after routine cardiology examinations, and in special cases genetic tests are also performed to establish the final diagnosis.
To the routine examinations of the cardiology includes the physical exam, that electrocardiogram (EKG), the echocardiogram, the cardiac catheter examination, the chest X-ray and in some cases the heart muscle biopsy.
With the physical examination, the cardiologist approaches the diagnosis by looking for typical changes in the body related to cardiac disorders. The electrocardiogram allows the doctor to check the electrical function of the heart.
Here the cardiologist can make a statement about the functionality of the electrical lines and can thus also record the electrical disturbance typical of a specific cardiomyopathy. The echocardiogram has meanwhile become the standard examination in cardiological diagnostics. Here the doctor can get a direct picture of the heart and, if necessary, the disorder.
The doctor also sees the Echocardiography how the blood flow is inside the heart. The flow of blood within the heart says a lot about how functional the heart muscle is. The Myocardial biopsy is a procedure in which a small piece of heart tissue is removed in order to later make a statement about the pathological changes in the heart at the cellular level. This examination often goes along with other areas of medicine such as pathology.
The cardiac catheter examination is often used to rule out that one of the heart vessels is clogged and thus can potentially trigger symptoms typical of the heart.
How is the therapy of cardiomyopathy carried out?

The therapy of Cardiomyopathy depends on the disorder caused by the cardiomyopathy.
Accordingly, the doctor must of course recognize whether it is a primary or one secondary Cardiomyopathy. Dilated cardiomyopathy is based on the fact that the heart chamber is abnormally enlarged and the blood volume cannot be adequately pumped.
Here the therapy aims at:
- a Decrease in the circulating volume
- Lowering blood pressure and a
- Lowering the work of the heart.
So that becomes heart protected and can pump more efficiently. By expanding the heart it can too Cardiac arrhythmias come, which must also be treated.
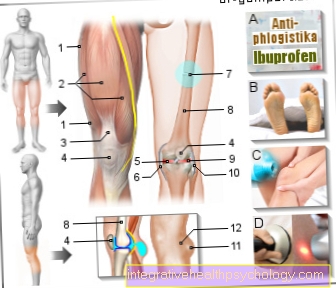
The therapy uses blood thinners and drugs that regulate the heart rate. In severe cases it must be considered whether a Pacemaker therapy makes sense. In hypertrophic obstructive cardiomyopathy, the heart is fighting a constant obstacle. This costs the heart a lot of strength, which can ultimately lead to heart fatigue.
Come to lessen the work of the heart beta blocker and Calcium inhibitors used because they reduce the heart's strength and improve the filling of the heart. If the drug therapy for cardiomyopathy is ineffective, the parts of the heart that represent the obstacle can also be rendered ineffective by invasive measures, or removed as part of a surgical procedure.
The therapy of restrictive cardiomyopathy is also carried out according to the given symptoms and can be treated in a similar way to dilated cardiomyopathy or hypertrophic obstructive cardiomyopathy. Since in many cases there is also inflammation of the heart muscle with involvement of the pericardium, these must also be treated with anti-inflammatory drugs.
The unclassified and right ventricular cardiomyopathies can also only be treated symptomatically.
Rehabilitation / prophylaxis
Cardiomyopathy rehabilitation aims to improve quality of life and life expectancy. This is achieved in particular with the help of medication and the prevention (prophylaxis) of other diseases. Important diseases that should be prevented are the Diabetes mellitus and the high blood pressure. In addition, attention should be paid to diet, as poor nutrition can lead to the diseases mentioned above and thus worsen cardiomyopathy.Regular and controlled exercise reduces the risk of suffering from other diseases and promotes training of the cardiovascular system. Besides, that should Smoke should be avoided, as it has been proven that smoking is largely involved in the development of cardiovascular diseases. This is where toxins develop that attack the vascular walls and, in particular, can constrict the coronary vessels.
forecast
In primary dilated cardiomyopathy, the course of the disease can either be stable and more or less controlled, or there can be a rapid deterioration in cardiac function. As a rule, the 5 year survival rate with adequate drug therapy is 20%.
Sudden cardiac death is the cause of death in 20-50% of patients. Patients with hypertrophic obstructive cardiomyopthia usually suffer sudden cardiac death between the ages of 10 and 30.
Clinical prognostic factors are used here to predict the probability of sudden cardiac death. These are, for example, how well the heart pumps and whether certain laboratory values are elevated. The prognosis of dilated cardiomyopathy essentially depends on the comorbidities causing the cardiomyopathy and, if applicable, how well the anti-inflammatory therapy responds to the myocarditis.











.jpg)