Esophageal cancer diagnosis
All information given here is only of a general nature, tumor therapy always belongs in the hands of an experienced oncologist!
Diagnosis
Diagnostics initially has two goals:
Exclusion or confirmation of a tumor of the esophagus:
If you suspect one Esophageal tumor the patient must first be questioned in detail (anamnese), especially about previous illnesses, about theirs Alcohol consumption (alcohol dependence) and Nicotine consumption (smoking) and familial accumulations certain diseases.
Then the patient is thoroughly examined.
In the Analysis of the blood (laboratory) certain blood values (Laboratory values), in combination with the patient's complaints and physical examination findings, indicate esophageal cancer, even if they ultimately cannot be regarded as conclusive.
For example, low blood pigment levels (Hemoglobin) indicate chronic blood loss in the blood. However, this also applies to many other diseases. So-called Tumor markers are substances in the blood that are often found in some types of cancer and can therefore indicate a disease.
They do not play an essential role in the initial diagnosis of esophageal carcinoma, since it does no reliable tumor markers in this condition. However, if you find a certain tumor marker value elevated before the operation, which disappears after the operation, you can use this marker particularly well to prevent the tumor from breaking out again (Tumor recurrence) can be quickly diagnosed with a blood test.
In the case of squamous cell carcinoma (a form of esophageal cancer that originates from the cover cells), the tumor marker value can sometimes be found SCC in the blood and in adenocarcinoma (a form of esophageal cancer that starts from the gland cells) CA 19-9 be increased.
If the symptoms match, one is as soon as possible Esophagoscopy (Esophago gastroscopy).
Of the roentgen - Swallowing porridge can in some cases also suggest a tumor.

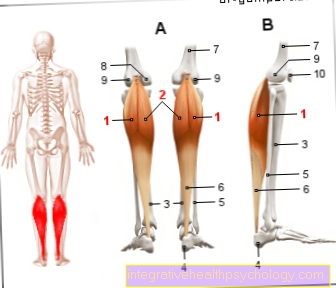
- esophagus
(Neck section) -
Esophagus, pars cervicalis - Nasal cavity - Cavitas nasi
- Oral cavity - Cavitas oris
- Windpipe (approx. 20 cm) - Trachea
- esophagus
(Chest section) -
Esophagus, pars thoracica - esophagus
(Abdominal section) -
Esophagus, pars abdominalis - Stomach entrance -
Cardia - Stomach body -
Corpus gastricum - Throat -
Pharynx - Thyroid -
Glandula thyroidea
You can find an overview of all Dr-Gumpert images at: medical illustrations
X-ray - swallow of porridge:
This non-invasive imaging exam will use the esophagus X-rayed while the patient swallows an X-ray contrast medium. The contrast agent is placed on the esophageal wall, whereupon it is accessible for assessment. The typical finding in a tumor is frayed and irregular, it is also said "Pitted" mucous membrane wall. You can also choose the degree of Narrowing of the esophagus (stenosis) through a tumor.
However, the X-ray swallow is not a diagnostic procedure by which every esophageal tumor can be reliably detected. For this, the direct assessment of the esophagus wall by means of an esophagoscopy is necessary.
Nevertheless, it is often used for tumors that cannot be passed with the endoscope (camera of the esophagus specimen). Despite this handicap, the length of a tumor and the degree of narrowing of the esophagus can be determined. In addition, this investigation is the means of choice for one esophago-tracheal fistula to diagnose. In this case, a small duct-like structure can be seen on the X-ray swallow image as a connection between the esophagus and the Windpipe (trachea).
Note diagnostics
If such a fistula is suspected, a water-soluble contrast medium should always be used, as contrast medium containing barium triggers a severe foreign body reaction in the lungs.
Endoscopy (esophago-gastroscopy = esophagus-gastroscopy)
"Endoscopy" of the esophagus and stomach is the method of choice for direct assessment and classification of mucosal damage and should be performed as soon as possible if an esophageal tumor is suspected. During this examination, images are transmitted to a monitor via a tube camera (endoscope). When doing the reflection, the examiner also pays attention to very discreet changes in the mucous membrane and local flat color changes so as not to miss a small carcinoma. During the endoscopy, tissue samples (biopsy) can also be taken from suspicious areas of the mucous membrane. The tissue assessment under the microscope (histological finding) is far more informative than the (macroscopic) finding with the naked eye. Only in the histological examination can the suspected tumor be proven and the tumor type determined, as well as its spread in the wall layers of the esophagus.
Chest x-ray
An overview x-ray of the chest (chest x-ray) can sometimes be an indication of a tumor in the middle of the chest. Particularly in the late stages, you will find a widened middle chest (mediastinum), affected lymph nodes, you may even see lungs and skeletal metastases or pneumonia as a result of a fistula formation between the trachea and esophagus.
Read more on the topic: Chest x-ray (chest x-ray)
Such clues should further intensify the search for a tumor.
Determination of the tumor stage (tumor staging)
Once the diagnosis of esophageal cancer is confirmed, the tumor stage is then determined in order to plan further therapeutic action. In particular, patients who are at an early stage of the disease must be selected in order to subject them to an operation that may still be healing (curative) as quickly as possible.
Endosonography (endoluminal ultrasound)
With endoscopic ultrasonography, as with endoscopy, the patient has to swallow a tube during light anesthesia. However, in this examination, an ultrasound head is attached to the end of the hose instead of the camera. With this method, the spread of the tumor can be made visible by placing the transducer on the tumor (infiltration) and local (regional) lymph nodes can also be assessed. This method is superior to computed tomography (CT = X-ray sectional imaging) for tumor staging of esophageal cancer.
Computed Tomography
The spiral computed tomography (spiral CT) can provide information about the extent of the tumor, the lymph node involvement and, in addition, about distant metastases. You need a CT of both the chest (thorax), the abdomen (abdomen) and, if necessary, the neck. Depending on the location of the tumor, for example, lymph node metastases in the neck area and metastases in the lungs can be diagnosed in the case of a tumor located in the neck part and metastases in the liver in the case of tumors located further down.
Magnetic resonance imaging (MRI) also provides similar results.
Sonography
With sonography (ultrasound) as a non-invasive and fast procedure, metastases and affected lymph nodes can be identified. During the ultrasound scan of the abdomen (abdomen), for example, metastases in the liver or affected lymph nodes can be seen.
In the case of sonography of the neck, the cervical lymph nodes can be clearly visualized and assessed for tumor involvement.
Skeletal scintigraphy and F-18 fluorine PET
Skeletal scintigraphy and F-18 fluorine PET are nuclear medical examinations and are used as part of tumor staging to discover distant metastases. For this purpose, a radioactively labeled substance, such as phosphonate or fluorodeoxyglucose, is administered intravenously to the patient and then the radioactive substance, e.g. in the bone, made visible with a special camera. The radioactive substances accumulate in the tissue of the metastasis. Bone metastases appear as an increase in accumulation (less often due to reduced storage) of the radioactive substance in the image.In skeletal scintigraphy, the reasons for the increased radioactive storage lie in the increased blood flow to the tumor, increased permeability of the vessels and the nature of the surface of the metastasis.
The F-18-PET makes good use of the fact that the tumor has an increased metabolism. In this way, the tumor can absorb more of the radioactively labeled substance compared to the neighboring tissue. In this way, the overactive skeletal metastases are made visible.
PET / CT
The diagnostic examinations normally carried out (computed tomography and endosonography) are not sufficient for very small metastases. PET / CT is what is known as fusion imaging because it combines the advantages of PET (see above) and CT (see above).
The disadvantage of PET is that it is difficult to establish the anatomical relationship between the metastasis and normal tissue. If the good spatial resolution of the CT is combined with the “staining” of the metastasis in the PET, a better statement can be made about the anatomical position of the tumor or metastasis.
Read more on the topic: Positron emission tomography
During or after chemotherapy or radiation therapy, this method can be used to monitor the therapeutic response of the tumor and that of the metastases.
Additional diagnostics
Sometimes it may be necessary to use additional diagnostic methods. Especially with tumors in the neck area, a thorough ENT examination aimed at. In tumors that are in close contact with the windpipe, a Lungoscopy (Bronchoscopy) can be helpful to assess the involvement of the windpipe (trachea). If the tumor is deep-seated adenocarcinoma, one may need one Laparoscopy (laparoscopy) in order to correctly assess the regional expansion.



.jpg)