Lens of the eye
Synonyms
Lens oculi
introduction
The lens is part of the eye system, lies behind the pupil and, together with other structures, is responsible for refracting the incident light beam.
It is elastic and can be actively arched over the muscles. In this way, the refractive power can be adapted to the various requirements. With age, the inherent elasticity and transparency decrease.

Classification of the lens
- Inner lens nucleus
- Lentil rind
- Lens capsule
- Hanging and accommodation apparatus
Anatomy of the lens of the eye
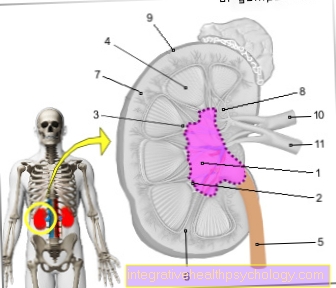
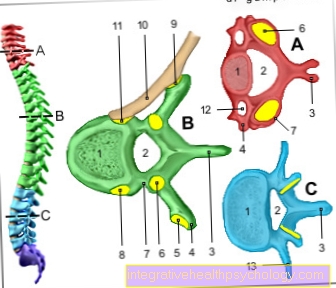
The lens is behind the pupil in the eye. The lens is encased in a lens capsule. The inside of the lens is transformed into a lens cortex (Outside) and a lens core (Inside) assigned.
The lens cortex and nucleus contain the lens fibers. On the inside of the anterior lens capsule and on the lens equator are cells (Lens epithelial cells), which form lens fibers for a lifetime. The fibers are deposited on the outside in a shell-like manner on the already existing fibers, release more and more water over time and become thinner and thinner. This creates the lens nucleus, which is denser and harder.
The lens is subject to age-related changes, so it gets bigger and harder. The result is a loss of self-elasticity, which leads to a certain degree of presbyopia in every person. In the course of life, the weight of the lens can increase fivefold. The lens is about 8-10 mm in diameter, about 2-5 mm thick and transparent. she is biconvex and slightly more curved at the back than at the front. The posterior part of the lens borders the vitreous humor.

- Cornea - Cornea
- Dermis - Sclera
- Iris - iris
- Radiation body - Corpus ciliary
- Choroid - Choroid
- Retina - retina
- Anterior chamber of the eye -
Camera anterior - Chamber angle -
Angulus irodocomealis - Posterior chamber of the eye -
Camera posterior - Eye lens - Lens
- Vitreous - Corpus vitreum
- Yellow spot - Macula lutea
- Blind spot -
Discus nervi optici - Optic nerve (2nd cranial nerve) -
Optic nerve - line of sight - Axis opticus
- Axis of the eyeball - Axis bulbi
- Lateral rectus eye muscle -
Lateral rectus muscle - Inner rectus eye muscle -
Medial rectus muscle
You can find an overview of all Dr-Gumpert images at: medical illustrations
Composition of the lens
The lens is made up of around 60% proteins, which consist of dense, stable crystallines. The remaining 40% contain water. The crystalline ensure stability against protein destruction (Denaturation). Furthermore, the lens has a high proportion of vitamin C (Ascorbic acid) and certain enzymes that are responsible for a certain "stress resistance" (anti-oxidative) to care. The high water content ensures transparency and, like the refractive power or elasticity, decreases in the course of life. Lens clouding also occurs with age.
Nutrition of the lens
The lens is nourished by the aqueous humor. The crystallines are negatively charged, so that predominantly positively charged salts (Cations) are important. The lens epithelium has a pump that transports potassium into the lens and sodium back into the aqueous humor. The lens does not contain any nerves or blood vessels.
physiology
The lens the eye is about fibers (Zonular fibers) in the so-called ciliary body of the Eye hung up. The ciliary muscle is located in the ciliary body. It is a ring-shaped muscle that contracts when you contract.
If the muscle tenses, the zonular fibers are relaxed and the lens becomes rounder thanks to its inherent elasticity. When the ciliary muscle relaxes, the zonular fibers are tightened and the lens becomes flatter. In this way, the refractive power of the lens can be adjusted and objects near and far can be seen clearly. This process is called Accommodation. At the See nearby (e.g. while reading) the muscle is actively tensed to increase the refractive power. This explains why, after a while, the activity of the muscle makes close vision more and more strenuous. When seeing in the distance, the muscle is maximally relaxed.
Other parts of the eye also have a certain refractive power, but it cannot be changed. Have so Cornea, Aqueous humor and Vitreous a rigid refractive power. The refractive power of the eye can only be varied and adapted by means of spherical and flattening the lens. The refractive power of the cornea is approx. 43 dpt. The refractive power of the lens is 19 dpt and. Accommodation width, i.e. the range that can be varied, is 10 - 15 dpt and depends on age.
Children and young adults usually show a full range of accommodation. It decreases with age (Presbyopia).
Function of the lens
The lens is responsible for the refraction of light with the eye chambers and the chamber fluid. This process is important so that what you see in your environment is correctly displayed on the retina. The refractive power of the light-refracting apparatus can be adjusted by deforming the lens.
The lens is biconvex in humans, that is, it is curved on both sides. The lens is deformed by pulling the zonular fibers on the lens capsule. The condition of the zonular fibers in turn depends on the tension of the ciliary muscles. The more the ciliary muscles contract, the more relaxed the zonular fibers are.
When the ciliary muscles relax again, the zonular fibers are under tension. The tensioned zonular fibers then exert tension on the lens capsule and so the lens deforms and becomes flatter. When the zonular fibers relax, the pressure on the lens capsule is reduced and the lens takes on a round shape again due to its own elasticity.
The lens consists of lens fibers and one Lens nucleus. The core loses water with age. This loss contributes to the fact that the elasticity, i.e. the deformability, of the lens decreases with age. If the lens is round, the refractive power is greater, that is, light is refracted more strongly. The ciliary muscles are mainly supplied by the parasympathetic nervous system, but some of them also receive sympathetic signals.
There are two main processes involved in adjusting the refractive power: near and far accommodation. The near accommodation is used to adapt the refractive power to objects that are close to the eye. For this, the ciliary muscles are tensed by the action of the parasympathetic nervous system and thus the lens relaxes and becomes round. The curvature of the lens is thus maximal and the light is refracted more strongly.
The opposite happens with distance accommodation. The parasympathetic innervation is inhibited and the lens becomes flatter. If the sympathetic system is also activated, the lens is completely relaxed and reaches its lowest refractive power. As mentioned above, the lens loses its elasticity with age and this reduces the maximum refractive power. As a result, the near point, the point from which one can see clearly, moves further and further away and one develops presbyopia.
What is lens opacification?
The lens opacity is also known as cataract or cataract. In Germany, the most common form is age-related lens opacification. A number of factors, including injury, diabetes, radiation, and mostly age, cause the lens to become cloudy. As a result, vision is clearly restricted. Those affected describe the symptoms like a thick fog that lays in front of the eye. The discomfort may improve when looking at nearby objects. The reason for this is that the lens is deformed to fixate a nearby object. A causal therapy for the disease has not yet been researched, but an operation in an advanced stage can significantly improve vision again. Here the diseased lens is replaced by an artificial implant.
Operation on the lens
There are several reasons to perform an operation on the lens.
For example, a refractive lens exchange can be carried out in the event of severe visual disturbances. The aim of this operation is to reduce the limitations of severe farsightedness or nearsightedness. As a rule, the operation is only carried out after the age of 50 or after presbyopia has set in. The old lens is removed and replaced with an artificial lens. Replacing the lens, however, leads to a loss of the natural ability to accommodate, and for this reason, lens replacement only makes sense if there is an existing visual impairment. The new lens is set to a certain refractive power, mostly for distance vision, and then often has to be accompanied by a supporting visual aid for near vision.
In addition to replacing the lens for farsightedness or nearsightedness, artificial lenses are also used for cataracts. Here the clouded lens is also replaced by an artificial one. In order to be able to plan the procedure well, a number of examinations must take place before the operation. In this way, the doctor can weigh up whether or not it makes sense to exchange lenses, since artificial lenses cannot correct all visual defects. A common treatment goal should also be set and it should be clear in advance to what extent additional visual aids (e.g. reading glasses) will be required afterwards.
The procedure itself is usually carried out on an outpatient basis and under local anesthesia. During the operation, the old lens must be removed and the new lens inserted and fixed. To remove the old lens, it is first disassembled into small pieces. This is done using ultrasound and is completely painless. A small suction device is then inserted through a small opening and the fragments of the old lens are sucked off. The lens capsule is retained and can then serve as a holder for the new lens. The new lens is folded over the same opening and inserted into the capsule. Here it unfolds completely and can therefore replace the old lens. There is also the option of using a femtosecond laser for cutting support. This makes opening the capsule and the cornea easier.
Read more on the topic: Cataract surgery
Artificial lenses
So-called intraocular lenses (IOL) are mostly used as lens replacements. The intraocular lens consists of an optical part that replaces the original lens and a holder (haptic) for fixing the lens in the eye.
Artificial lenses can be either hard or soft. Hard lenses are made from polymethyl methacrylate. Soft lenses are foldable, which can be beneficial for the procedure, and are made of silicone, acrylic or hydrogel. The diameter of the optical zone is usually about 6 mm. A distinction is made between different lenses depending on the shape and area of application.
In order to correct poor eyesight, positive or negative refractive intraocular lenses are usually used. The positive refractive intraocular lens is used to correct farsightedness, while the negative refractive intraocular lens is used to correct myopia.
Multifocal lenses are used to correct presbyopia combined with pre-existing poor eyesight. There is also the possibility of using an accommodating lens, which can mimic the natural accommodation of a lens.
A toric lens can be used to improve visual impairment caused by astigmatism. Toric lenses have a special shape and can therefore compensate for the curvature of the cornea. Phakic intraocular lenses (PIOL) can also be used as an alternative to intraocular lenses. With phakic intraocular lenses, the natural lens is not removed, but the artificial lens is only inserted additionally. These lenses are suitable for the correction of ametropia, but not for the treatment of cataracts.
Can you see something without a lens?
The main task of the lens is to adjust the refractive power of the eye. By deforming the lens, it is possible to fix individual objects precisely. However, the lens is not the only part of the eye that can focus incident light rays. It is not the lens that has the greatest share in the refraction of light, but the cornea further forward in the eye. The lens itself contributes about 20 diopters to the total refractive power of the eye. A missing lens can therefore be compensated for with suitably strong glasses without any problems. As a result, however, it is no longer possible to fix objects in the vicinity. Before the development of modern implants, simply removing or destroying the lens was an often used therapy for lens opacity. This operation, known as star stitch, has been known around the world since pre-Christian times.