Medication for epilepsy
introduction
There are a number of therapeutic and medicinal options for treating epilepsy which are presented below.

Therapeutic options
The therapy of epilepsy should be causal as possible. This means that if a cause is known, it should be treated. If the cause is unknown, epilepsy can in principle be treated both with drugs and surgically.
The patient should always receive extensive advice on lifestyle. This includes, for example, information on sleep rhythm or how to avoid triggers such as alcohol.
Genetic counseling may also be offered.
Medicines are usually only used after at least two unprovoked seizures have occurred; a single seizure is not a sufficient indication for treatment. However, there are exceptions, for example if epilepsy is a vital threat, or in certain social circumstances, e.g. some professions. Furthermore, in the presence of epilepsy-typical changes in the EEG.
Under certain circumstances, the medication does not have to be taken for life: If no seizures occur while taking the tablets for 2-3 years, they can be gradually reduced over a period of 6-12 months and finally stopped completely.
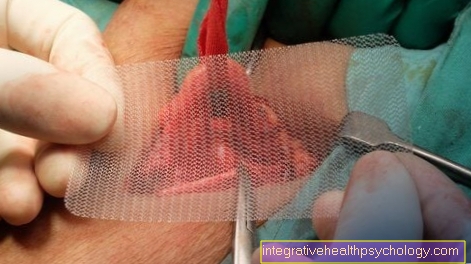
If medication is ineffective, the alternative is surgery. The prerequisite for this is the existence of a for the epileptic seizures responsible focus in the brain or a great deal of suffering on the part of the patient. The fact that at least two drugs have shown no effectiveness is also an indication for an operation.
If there is a focus, it can be surgically removed; if there is no focus, the use of a vagus stimulator is an option. This is a device that stimulates a nerve called the vagus nerve, thereby influencing the development of seizures.
Of the Status epilepticus is treated according to a graduated scheme. First, give for generalized seizures Lorazepam, at focal Conazepam. Should this not be effective, will Phenytoin administered. As a final measure, the patient is intubated and maintained phenobarbital.
Initially, monotherapy is sought. This means the use of only one drug from the group of anti-epileptics / anticonvulsants. If it is not effective, a different representative of this group should be administered first and combination therapy with a second anti-epileptic should only be started if it is again ineffective.
Medication administration in an emergency
Not every epileptic seizure needs immediate emergency medical treatment. Usually an epileptic seizure is not an emergency; it will go away on its own. It is therefore only important for bystanders that seizure-related injuries are avoided. Objects with potential for injury should be removed from the area.
If an epileptic seizure lasts longer than 5 minutes, one speaks of a status epilepticus by definition. This is an emergency. The seizure no longer ends spontaneously and must be interrupted by medication. If you suspect a status epilepticus, the emergency doctor should definitely be notified!
Most often, benzodiazepines are used as emergency medication. They often work within a few minutes. Lorazepam (Tavor expedit 1.0 or 2.5 mg) is the drug of choice for adults. This is placed in the patient's mouth as a readily soluble platelet and then absorbed by the body. Alternatively, you can also use diazepam. The drug is given in a small tube through the anus. It is available in 5mg and 10mg tubes. Emergency doctors or rescue workers usually inject the medication directly into the blood through a venous access.
If the status epilepticus persists despite the (multiple) administration of the above-mentioned medication, the doctor will administer a phenytoin infusion or, alternatively, another anticonvulsant medication.
How quickly do the drugs help in an emergency?
If the above-mentioned benzodiazepines are absorbed through the saliva (e.g. Tavor expedit) or administered rectally using a tube, the effect usually occurs after a few minutes. If the medication is injected directly into the vein, an effect can be seen after just 1-2 minutes. However, it can also happen that the status epilepticus cannot be interrupted despite (multiple) administration of medication.
prophylaxis
The therapy of epilepsy is mainly used prophylactically, i.e. If the prescribed medication is taken correctly, it should avoid further attacks and thus achieve freedom from attacks. In addition to drug prophylaxis, there is a change to a regulated lifestyle, which should eliminate possible triggers of epileptic seizures. Furthermore, there is a driving ban for several months after an attack.
Which drugs can be used in the prophylaxis of seizures?
There are numerous medications that can be used to prevent seizures. These are called anti-epileptic drugs or anticonvulsants. Depending on the type of epilepsy, you need to find the right drug and dosage for each individual patient. The dose is usually increased slowly. If further seizures occur during therapy with an anti-epileptic drug (monotherapy), a combination of several drugs makes sense in rare cases.
Phenytoin is a classic among the drugs for seizure prophylaxis; it has been used in the treatment of epilepsy for many years. However, due to its side effects, it is rarely used. Drugs such as carbamazepine and valproic acid, which have been on the market since the 1970s, are better tolerated. But here, too, there may be interactions with other drugs. Therefore, today mainly "new" anti-epileptic drugs are used, which are characterized by good long-term tolerance. The most important representatives are gabapentin, lamotrigine and levetiracetam (e.g. Keppra ®)
Lamotrigine
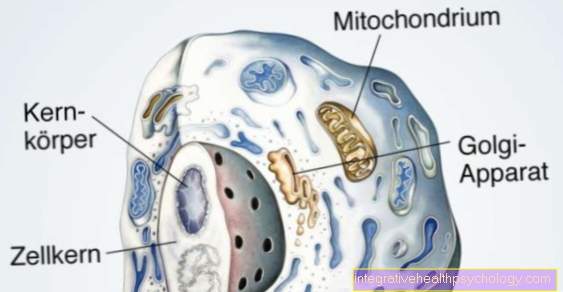
The drug lamotrigine has been used in the therapy of epilepsy since 1993. It is approved for the treatment of children aged 12 and over. The active ingredient is relatively new and there are few comparable drugs. The substance blocks ion channels in the central nervous system that are responsible for releasing the neurotransmitter glutamate. Neurotransmitters are biochemical substances that transmit stimuli from one nerve cell to another. This process is stopped by the lamotrigine. In addition to the treatment of epilepsy, lamotrigine can also be used for seizure prophylaxis in the event of alcohol withdrawal or severe depression. It is usually very well tolerated. An impairment of the ability to think and concentrate is rare compared to other anti-epileptic drugs. Known side effects are widespread skin rashes (exanthema), double vision, dizziness and imbalance. However, if the drug is crept in slowly, i.e. If you only gradually increase the dose, these can usually be avoided.
You can find more detailed information about lamotrigine on the following page: Lamotrigine, side effects of lamotrigine
Keppra®

Keppra® is the trade name for a drug with the active ingredient levetiracetam. It belongs to the group of anti-epileptic drugs and is also used to prevent seizures in epilepsy. It is approved for young people aged 16 and over. The drug can be administered as a tablet or as an infusion.It is metabolized independently by the liver and excreted in the urine. The exact mechanism of action has not yet been finally researched. The drug probably inhibits the transmission of stimuli to the synapses (= the connection point between two nerve cells) and can thus prevent seizures. Side effects include tiredness, headaches and difficulty concentrating. Furthermore, nausea and vomiting can occur. Allergic skin reactions are also typical. The drug must not be taken during pregnancy and in the presence of impaired kidney function.
Read more about epilepsy in pregnancy here
Gabapentin
Gabapentin is another seizure prophylaxis drug. Its mechanism of action is similar to the substances mentioned above; it blocks ion channels in the central nervous system and thus prevents the transmission of stimuli between the nerve cells. It is used as monotherapy for simple epileptic seizures. It can also be used for "nerve pain" (= neuropathic pain), for shingles or for phantom pain. The drug must not be taken during pregnancy and breastfeeding as well as with impaired liver and kidney function. It should be known that gabapentin's effects are increased when it is taken at the same time as alcohol or opioid pain relievers.
You can find out more about gabapentin here.
Valproic acid
Valproic acid is also a well-known anti-epileptic drug. The salt that goes with it is called valproate. The drug is sold commercially under Ergenyl® or Orfiril®. In addition to various forms of epilepsy, valproic acid can also be used to treat mental illnesses such as mania and psychosis. It is also used for Huntington's disease. The drug can be administered as a tablet or directly via the bloodstream. It is metabolized by the liver. Therefore, it must not be taken in the case of liver dysfunction. It is also not suitable as a drug for women of childbearing potential, as it could damage the embryo in the event of an unplanned pregnancy. It should therefore also not be taken during pregnancy.
More information on this topic: Side effects of valproic acid
Phenytoin
The drug phenytoin is a well-effective and well-established drug for the therapy of epilepsy. It is also used to treat cardiac arrhythmias. Similar to the local anesthetic lidocaine, phenytoin blocks an ion channel and thus slows down the transmission of stimuli between two cells. This works both in the central nervous system and in the heart. Known side effects are dizziness, double vision, blood disorders, liver dysfunction and allergic reactions. In addition, the drug often interacts with other drugs. It must therefore be said that it has been used less and less for the treatment of epilepsy in recent years, especially since many newer anti-epileptic drugs with better long-term tolerance came onto the market.
Read more about phenytoin and its side effects and interactions here
Carbamazepine
Another drug for epilepsy is carbamazepine. It can also be used to treat mental illnesses known as bipolar disorder and mania. The drug is also popular with trigeminal neuralgia, facial pain in the supply area of the trigeminal nerve. Like most anti-epileptic drugs, it works on the ion channels in the central nervous system and thus reduces the excitability of the nerve cells. Side effects are allergic rashes, itching, disorders of the blood-forming system and mood swings. However, these can usually be avoided by carefully increasing the dose. It is important to know, however, that metabolism in the liver can lead to interactions with other drugs.
forecast
1. Generalized seizures:
Freedom from seizures in grand mal epilepsy is achieved in around 50% of cases, in absenteeism in around 25% of cases.
The West and Lennox-Gastaut syndrome however, have a bad prognosis.
2. Single partial seizures:
Up to 75% of patients are seizure-free under drug therapy.
3. Complex-partial seizures:
In about 33% of those affected, the seizures stop under therapy.
Summary
epilepsy is a clinical picture that occurs due to uncoordinated discharges of nerve cells in the brain and manifests itself in motor, vegetative, sensitive, sensory or psychological complaints.
The epileptic seizures are treated either with the help of medication or surgery. An operation (removal of parts of the brain, Brain amputation) is only performed in very serious cases. In all cases, an individual therapy decision and a lifestyle that avoids triggers is important.