Post-nasal drip syndrome
What is Postnasal Drip Syndrome
In the case of postnasal drip syndrome (PNDS), fluid drips down from the nasopharynx into the throat ("postnasal" lat. = Coming towards the nose, "drip" = drip). It is a runny nose, so to speak, except that the secretion does not come out of the nose in the front, but in the back towards the throat. Postnasal drip syndrome is often caused by a stuffy nose and is associated with a runny nose. PNDS is not an independent clinical picture, but a syndrome that can occur in the context of a wide variety of diseases.

treatment
Treatment for postnasal drip syndrome depends on the triggering factor. If you have a cold, a decongestant nasal spray can relieve the blocked nose and ensure that the mucus can drain out of the front of the nose. Usually a cold is caused by viruses, which is why antibiotic treatment makes no sense. However, a harmless cold often heals on its own within a few days and does not require any explicit treatment. Green nasal secretions may indicate a bacterial infection that may need antibiotic treatment. The doctor can prescribe expectorants to counteract the build-up of mucus and dry coughs. If an allergy is the cause of PNDS, antiallergic drugs such as antihistamines or glucocorticoids can help.
Depending on the cause of the disease, surgery may also be necessary to remove constrictions and the resulting nasal congestion. The surgeon will try to be as minimally invasive as possible so as not to leave any scars on the face. During the operation, the paranasal sinuses are opened in an attempt to restore the normal function of the mucous glands. After the operation, patients have to use cortisone-containing nasal sprays for several weeks and regularly rinse the nasal mucosa with sea salt water.
Read more about this topic at:
- Nasal spray with cortisone
- Nasal spray for an allergy
Home remedies
A number of different home remedies have proven themselves in the treatment of postnasal drip syndrome and can be used to loosen mucus. An effective way to treat nasal congestion is a nasal douche or gargling with a salt water solution. The salt water solution can easily be prepared by yourself by dissolving a teaspoon of salt (preferably sea salt) in 250 ml of warm water.
Another expectorant option is to inhale essential oils or herbs (e.g. peppermint, chamomile or lavender) over hot steam.
During the illness, patients should take care to drink enough fluids in the form of warm tea and water. On the other hand, milk should be avoided, as this leads to increased mucus production. By drinking the mucous membranes are moistened and the viscous mucus can more easily loosen. In addition, moist air has a similar effect on the mucous membranes. This can be achieved by ventilating the rooms regularly or with the help of an air humidifier.
homeopathy
Homeopathy can be used for postnasal drip syndrome. Which globules or drops are best suited depends on the cause of the disease and the exact symptoms. Your pharmacist or a homeopath can help find a suitable homeopathic remedy.
Duration of a PNDS
The duration of a postnasal drip syndrome depends not only on the cause of the disease and its course, but also on the therapy used. If the cause of the disease is not treated properly, a chronic cough or bronchitis and, in the worst case, bronchial asthma can develop. If the symptoms are caused by a cyst or tumor in the paranasal sinuses, the PNDS remains until it is surgically removed.
causes
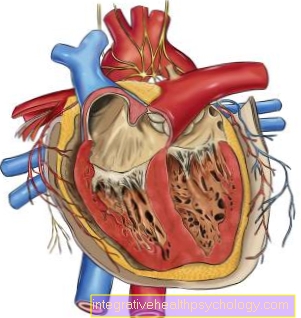
The cause of the development of postnasal drip syndrome is that the mucous glands in the nasal mucosa and the sinuses of the head produce too much secretion. Usually the slimy secretion protects the mucous membrane from the penetration of pathogenic viruses and bacteria. The trigger for the excessive production of mucus is usually an inflammation of the nasal mucous membrane (Rhinitis), the paranasal sinuses (Sinusitis) or a combination of these two forms (Rhinosinusitis).
The postnasal drip syndrome can accordingly occur in the context of a cold, the flu or a sinus infection. But allergies or anatomical misalignments of the nose can also lead to PNDS. Furthermore, some drugs and foods or external stimuli such as chemicals or exhaust fumes (including cigarette smoke) can trigger postnasal drip syndrome. Post-nasal drip syndrome can also temporarily occur during pregnancy due to hormonal changes.
As the mucus leaks into the throat, the secretion drains into the lower airways and can lead to infections of the lungs (e.g. bronchitis) and the throat. This phenomenon is known as "floor change" and is typical of PNDS: although the origin of the disease lies in the upper respiratory tract, it comes to an infection of the lower respiratory tract.
Read more on this topic at:
- cold
- flu
- Sinus infection
These symptoms tell me that I have the disease
The most characteristic symptom of postnasal drip syndrome is the constant flow of mucus from the nose into the throat. Those affected notice that they have to swallow or spit mucus. Clearing the throat and dry coughing attempts to move the mucus up from the lower airways, which is why a chronic cough is often a symptom of PNDS. In this case the cough is a protective mechanism of the body that tries to prevent the slimy secretion from entering the lungs by coughing up. Furthermore, PNDS causes itching in the throat, which occurs mainly at night when lying down, and can lead to hoarseness and a hoarse voice. Typically, the nose is also blocked and nasal breathing is hindered or even short of breath.
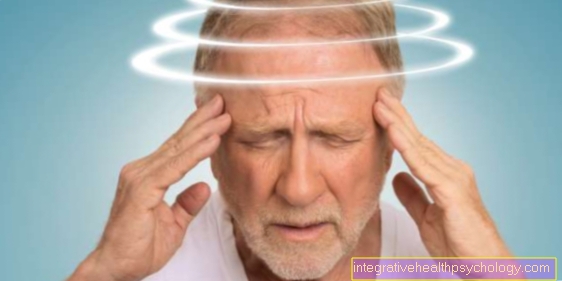
Further symptoms depend on the cause of the postnasal drip syndrome. However, since there is usually an allergic or non-allergic inflammation of the nasal mucous membranes, the result is a runny nose, headache, toothache and impaired smell. The swallowed mucus can also lead to inflammation of the lower airways (acute bronchitis).
You might also be interested in these topics:
- sniff
- Swollen nasal lining
- Burning sensation in the nose
How is PNDS diagnosed?
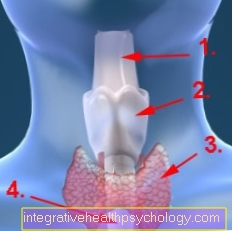
The doctor (preferably an ENT specialist) makes the diagnosis of postnasal drip syndrome in addition to the patient's medical history using a nasal endoscopy (nasal cavity endoscopy). To do this, he inserts an endoscope with a light source into his nose, examines the mucous membranes and looks for causes of the nasal congestion. The patient's throat is then inspected to see if there is an excessive flow of mucus.
These examinations are usually sufficient to diagnose PNDS and determine the underlying disease. In rare cases, when no cause for PNDS can be found, the doctor may order a CT or MRI of the head. These imaging tests can better assess the pharynx and sinuses and diagnose possible causes. If an allergic event is suspected, the doctor initiates an allergy diagnosis (skin test, laboratory test or provocation test).