Risperdal
Explanation / definition
Risperdal® is a so-called “atypical neuroleptic”, ie a very modern drug against psychoses. In addition, it is also used in the treatment of mania.
Risperdal® is one of the few drugs that can also be used as a so-called "depot". With such a depot medication, the daily tablet intake is omitted and the patient is instead given an injection at a certain interval (2-4 weeks).
Trade names
Risperdal®

Chemical name
Benzisoxatol (piperidine)
Active ingredient
Risperidone
application areas
Schizophrenia - both in acute and further treatment
Mania - both in acute and further treatment
Dementias - but only with psychotic symptoms such as Delusion, hallucinations or aggressive behavior
Borderline disorder - in the case of repeated self-injurious behavior or behavior that is dangerous to others
Intellectual disability - for impulse breakthroughs and chronic aggressiveness.
Please also read: Neuroleptics
effect

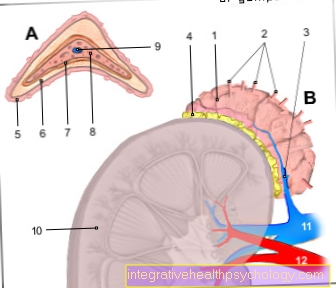
The main effect of Risperdal® is that it dampens the oversupply of the transmitter substance "dopamine". This oversupply is now seen as the main cause of psychotic perception (e.g. hallucinations).
Basically, the system of the transmission of messages between nerve cells works using a “key and lock principle”. A nerve cell releases a messenger substance (e.g. dopamine). This messenger substance fits like a key to various other nerve cells. The messenger substance “lays” itself in this lock (the so-called dopamine receptor) of the nerve cell and unlocks it. Biologically, this process of unlocking means that the unlocked nerve cell becomes active (it fires an impulse). Once the dopamine has done its job, it returns to its original cell like a car in the garage. One can now easily imagine that an oversupply of messenger substance can result in constant "unlocking" and the unlocked nerve cell constantly firing impulses. If this happens in all important areas of the brain, it comes to a pathological perception.
Risperidone (Risperdal®) now (like all other antipsychotically effective neuroleptics) blocks the dopamine receptors to such an extent that an excess of dopamine no longer leads to such a pathological change.
dosage
In schizophrenia: start with 2-4 mg divided into 1-2 doses per day. The maximum dose here is 8 mg.
Author's note
There are statements that put the maximum dose at 16 mg per day. Experience has shown that Therapy for schizophrenia however, an increase beyond 8-10 mg no longer has an additional positive effect. However, the risk of side effects increases immensely with such a dosage.
You can also find more information under our topic: Schizophrenia
At Mania: A dose of 3-4 mg per day is recommended. The dosage of 6 mg should not be exceeded.
You can find further information under our topic: Therapy of mania
At a Dementia disease: Here you should enter the medication very carefully. An initial dose of 2x0.25 mg is recommended. If there are no side effects, the target dose should be 2x0.5 mg. In individual cases you can continue to dose more in 1 / 4mg steps.
Further information on this topic can also be found at: dementia
In the Depot medication Nowadays you start with 25 mg every 2 weeks. However, depending on the severity of the disorder, doses of 37.5 mg and 50 mg (maximum dose) are also possible.
In the Borderline disorder: Unfortunately, both self-harm and “psychosis-related” states are not uncommon in borderline illnesses.
In my experience, dosages between 1-3 mg Risperdal® are helpful in order to get a grip on the pressure of self-harm as well as any "psychosis-like" misperceptions. Of course, drug therapy alone can never be Borderline replace oriented psychotherapy.
In individual cases, the dosage can also be higher (depends on the severity or the likelihood of relapse). During the switch from tablets to depot medication, simultaneous treatment must take place for about 3 weeks, as the depot has no immediate effect.
Side effects
The so-called EPS (extrapyramidal disorders) are most common (in up to 20% of patients) with Risperdal®. This includes side effects that have to do with motor skills and movement in the broadest sense.
The EPS is basically divided into:
Early dyskinesia: These include symptoms such as physical restlessness, muscle twitching, involuntary sticking out of the tongue, eye cramps. These disorders regress after stopping the drug.
Tardive dyskinesia: These symptoms can occur after years of taking neuroleptics. The symptoms are similar to those of early dyskinesias. In addition, there are typical movement patterns and facial movements. These disorders are permanent.
Author's note: In my medical career to date, I have never met anyone with tardive dyskinesia that can be traced back to Risperdal®.
Parkinsonoid: These symptoms are reminiscent of the clinical picture of Parkinson's disease. This leads to a limitation or loss of fine motor skills, small steps, tremors (tremor), general rigidity (rigor) and loss of facial muscle movements (amimia).
Akathesia: This is used to describe a very agonizing unrest. Despite their best efforts, the patients cannot sit still, but typically “rock” up and down.
Other common side effects are:
Insomnia, headache, drop in blood pressure and dizziness
Less common side effects are:
Potency disorders (erectile dysfunction), nausea, milk flow
In individual cases (epileptic) seizures and a drop in white blood cells (leukopenia) can occur.
Please also read our topic: Risperdal® side effects
Interactions
If clozapine is administered at the same time, the concentration of clozapine in the blood may increase.
With simultaneous administration of Carbamazepine Risperdal® in the blood drops.
Drugs against high blood pressure can have an increased effect in combination with Risperdal®.
Risperdal® and alcohol
Risperdal® is a Psychotropic drug, a drug that is used in mental illness again schizophrenia, of the mania or other mental illnesses in order to reduce the symptoms of the illness.
In which Psychotropic drug Risperdal® is a drug that is only very bad with alcohol tolerates why alcohol while taking Risperdal® advised against becomes. The problem is that, on the one hand, both the drug Risperdal® and the alcohol over the liver is broken down and then eliminated from the body.
This can lead to the liver breaking down the drug Risperdal® and not being able to break down and excrete the alcohol at the same time. This can cause the Effect of alcohol intensified or the opposite scenario, it happens that the liver cannot break down the Risperdal® and it therefore remains in the body longer, which then happens increased side effects can lead.
Furthermore, Risperdal® just like alcohol in the brain acts on different receptors. You have to imagine this receptor like an office chair. Risperdal® can only develop its effect when it is on this receptor, i.e. on the office chair. However, if a molecule of alcohol blocks this receptor, i.e. the office chair, Risperdal® cannot work.
This leads to the positive effect of Risperdals® not applicable while the Side effects of the Risperdals® reinforced by the alcohol become.
So while taking Risperdal®, alcohol should be avoided if possible to do without completely, as otherwise undesirable side effects and a weakening of the actual effect can occur.
Stop using Risperdal

Many patients want or have to stop Risperdal® after a while. This can have different causes. On the one hand, it may be that the patients should only take Risperdal® temporarily, for example if they were in an aggressive phase, or the side effects of Risperdal® are too high so that the patient would like to stop Risperdal®.
If a patient wishes to discontinue Risperdal®, they should first talk to their treating psychiatrist about it so that he can assess whether the patient is stable enough not to have any problems with a reduced dose of Risperdal®.
It is always important to keep in mind that the patient had to take Risperdal® for a specific reason, such as schizophrenia or mania. If the patient now stops Risperdal®, the symptoms of schizophrenia or mania may intensify again.
In addition, various side effects such as restlessness or insomnia occur when you stop taking Risperdal®. It is therefore important to discuss the exact steps with the psychiatrist, as he can best assess when the patient can start reducing the dose of the drug without too great side effects.
It is crucial that the dose of Risperdal® is reduced in small steps and over a long period of time, up to a year, until the Risperdal® is then completely discontinued. On the other hand, if a patient rushes to discontinue Risperdal®, the side effects are very severe and the likelihood that the patient will revert to the original illness is much greater. It is therefore extremely important to develop a plan together with the psychiatrist as to when and how the best time is to discontinue Risperdal® in stages.
This step-by-step withdrawal from Risperdal® or psychotropic drugs in general is referred to as tapering off and is the gentlest and least side-effect method to be able to stop a psychotropic drug such as Risperdal®.
Read more on the topic: Stop using Risperdal
price
Since there is always talk of cost pressure in the healthcare sector, we believe it is important to also find out prices for drugs (prices are exemplary and not recommended):
Risperdal® Tablets 2 mg 50 tablets (N2) € 123.11
Risperdal® Tablets 4 mg 100 tablets (N3) € 450.76
Risperdal® Depot preparation 25 mg 1 bottle € 139.87
Risperdal® Depot preparation 50 mg 1 bottle € 270.34
Status: January 2004
Prescription requirement
It exists for all Dosages Prescription requirement!