shoulder dislocated
What is a dislocated shoulder?
If the shoulder is dislocated one speaks medically of a shoulder dislocation (in English: shoulder dislocation).
A distinction is made between different forms and causes of a dislocated shoulder. The therapeutic options are also wide. However, a shoulder dislocation can also lead to some complications.
Read more on this topic: Shoulder dislocation

Symptoms of a dislocated shoulder
If the shoulder is dislocated, pain occurs in the joint area. Some of these occur at rest, sometimes only when moving. In addition, the shape of the shoulder has been changed, and the head of the humerus can be felt outside the pan. The socket is empty.
Read more on the subject at: Symptoms of a dislocated shoulder
Pain
A shoulder dislocation is extremely painful. Even the underlying accident event can lead to severe pain in the shoulder joint area, as well as swelling and bruising from injuries to the capsule, muscle or tendons.
If nerves and vessels are injured or trapped, the pain can also radiate into the hand or cause unpleasant sensations such as tingling or burning.
If you are in severe pain, you should use painkillers, usually the doctor prescribes anti-inflammatory drugs such as diclofenac.
How often does a dislocated shoulder occur?
About 0.4% of the population dislocates their shoulder each year, making this the most common form of dislocation.
Appointment with a shoulder specialist

I would be happy to advise you!
Who am I?
My name is Carmen Heinz. I am a specialist in orthopedics and trauma surgery in the specialist team of .
The shoulder joint is one of the most complicated joints in the human body.
The treatment of the shoulder (rotator cuff, impingement syndrome, calcified shoulder (tendinosis calcarea, biceps tendon, etc.) therefore requires a lot of experience.
I treat a wide variety of shoulder diseases in a conservative way.
The aim of any therapy is treatment with full recovery without surgery.
Which therapy achieves the best results in the long term can only be determined after looking at all of the information (Examination, X-ray, ultrasound, MRI, etc.) be assessed.
You can find me in:
- - your orthopedic surgeon
14
Directly to the online appointment arrangement
Unfortunately, it is currently only possible to make an appointment with private health insurers. I hope for your understanding!
You can find more information about myself at Carmen Heinz.
Causes of a dislocated shoulder
There are several mechanisms that cause the shoulder to dislocate. These include:
-
Traumatic dislocation: Here the joint head is levered out of its socket. This comes about, for example, by falling on the arm stretched backwards.
-
Habitual dislocation: The shoulder is dislocated without the use of force. This can be caused by weak muscles or ligaments, but joint misalignments can also lead to dislocations without trauma.
-
Recurrent dislocation: After a single traumatic dislocation, the shoulder dislocates repeatedly. The first event resulted in changes that lead to reduced stability in the shoulder joint. These include the Bankart lesion (see below), joint capsule enlargements and damaged ligaments.
Diagnosis of a dislocated shoulder
If a patient with a shoulder dislocation goes to the doctor, he should ask exactly how it came about.This is important in order to be able to distinguish between a traumatic and a habitual dislocation. In addition, the supply of blood and nerves to the arm must be checked. Important vessels and nerves that can be damaged by a dislocation run in the shoulder area.
X-rays of the affected area should then be taken. This allows bony injuries to be detected.
If the shoulder has already dislocated several times, a CT (computed tomography) or MRT (magnetic resonance tomography) image of the shoulder is recommended. Here the ligaments and muscles can be better assessed. In an MRI of the shoulder, damage to the joint lip (labrum) as well as the capsule and the rotator cuff can be assessed well.
therapy
The most common measure used when the shoulder is dislocated is straightening (the reduction). Before starting the reduction, injury to bones or vessels and nerves must be ruled out. Then the patient receives medication for pain therapy and sedation (stepping away, leads to forgetting the measure). Sometimes the reduction is performed under anesthesia. There are several ways to put the shoulder back in:
-
Reduction according to ARLT: The patient sits on a chair and hangs his shoulder over the back of the chair. Then there is a permanent train. The back of the chair should serve as a deflection point and push the joint head back into the joint socket.
-
Reduction according to HIPPOKRATES: The arm is pulled and turned while the patient is lying down, while the chest is pressed in the opposite direction.
After the reduction, the arm must be immobilized for about 14 days. This is followed by physiotherapy to prevent the shoulder joint from stiffening.
If there are bony injuries when the shoulder is dislocated or if the vascular / nervous system is affected, the dislocation must be treated surgically.
Read more on this topic: Therapy of a shoulder dislocation
Can I ball the shoulder in again myself?
A dislocated injury should be assessed and treated by a doctor. He can assess injuries to other important structures such as ligaments and capsule that may have long-term consequences. Nerves can also be injured in a traumatic shoulder dislocation. The ball should be done quickly after the injury and, above all, only by an experienced medical professional. Even if you have dislocated your shoulder several times, you should not adjust it yourself. If the shoulder dislocation occurs repeatedly, surgery can be useful.
When do i need an operation?
The indication for surgery is primarily made in patients who are still young and active. In these cases, the aim is for the shoulder to be stable and resilient again as quickly as possible. In many younger patients, after a conservatively treated dislocation, chronic instabilities in the affected shoulder appear over the years. Surgery is not necessarily recommended in older patients, as there are significantly fewer chronic instabilities after dislocation. However, it is also indicated in this group of patients if further damage has occurred in the joint, such as tears in the rotator cuff, bone and cartilage damage or nerve and vascular damage.
Further reasons to perform an operation are so-called recurrent dislocations. This means that the shoulder dislocates not just once, but often or regularly. In extreme cases, patients may dislocate the shoulder several times a day by making small movements. An important and relevant indication for surgery is also present when nerves or vessels are damaged. Therefore, after a dislocation, a doctor must urgently check the sensitivity (i.e. the perception of sensations) and the blood flow to the arms and shoulder region. In patients with recurrent or one-time dislocations, injuries to the labrum (part of the joint socket) are possible - the so-called Bankart lesion. But injuries to the humerus head (Hill-Sachs lesion) can also occur. These two types of damage can be detected by an X-ray and an MRI.
If there is only minor damage, then the operation can be performed arthroscopically. This means that only 2-3 small holes have to be made in the shoulder, through which a camera and surgical equipment can then be advanced. In this way, minor injuries can then be repaired and the ligaments and the capsular apparatus tightened.
If major injuries are seen, an open operation usually has to be switched to.
A shoulder brace or sling must be worn for approx. 4 - 6 weeks after the operation. Movements may only be performed with a physiotherapist. After about 6 weeks, careful muscle building and further physiotherapy can begin. Sport is generally possible. Sports that put pressure on the shoulder and that run the risk of a new dislocation should only be started again after approx. 6 - 9 months.
Unfortunately, an operation does not only bring advantages. The operation can damage the surrounding tissue. Then the arm must be kept completely still for a significantly longer time. The risk of a so-called frozen shoulder syndrome is higher after an operation than if no operation is performed. It should be noted here, however, that arthroscopic operations cause fewer problems than open operations.
Read more on this topic: Reasons and course of an operation for a shoulder dislocation
Which doctor treats the dislocated shoulder?
In the event of a shoulder dislocation, a doctor should be consulted quickly, even in an emergency. Even a general practitioner can assess the severity of the injury and possibly refer it to the specialist. A dislocated shoulder is best treated by a specialist in orthopedics and trauma surgery. They may order additional tests and procedures to assess shoulder joint stability and assess the need for surgical care.
Taping a dislocated shoulder
Taping the shoulder after a dislocation can be helpful. On the one hand, it can promote the healing process and, on the other hand, it can have a preventive effect and protect against further dislocations. The aim is that the tape absorbs forces that counteract the healing process. The basic principle is that a strip of tape is attached to the shoulder (from the front over the collarbone and shoulder to the back) and around the upper arm. Then an X is glued over the shoulder from two strips that start on the previously glued strips. Here the X is then fixed with additional tapes. With all tapes it is important that they are not glued too tightly. The execution should be done by an expert so that the taping does not have any negative consequences.
Read more on this topic: Tape bandage
Bandage for a dislocated shoulder
There are various bandages available on the market that are offered to protect the shoulder from being dislocated again. After the operation, wearing a bandage is indicated for 3 to 6 weeks. It must always be worn at night for this period. During the day, however, from about the 3rd week onwards, only when the shoulder cannot be put down.
A frequently used bandage is, for example, the OmoLoc®. In the long term it is important that the shoulder is not held in the bandage, as this can stiffen the shoulder. There are different bandages for strength and contact sports. Whether and how these can be used individually for the person concerned should be discussed with the attending physician.
A so-called Gilchrist bandage is used for both conservative and surgical treatment of a dislocated shoulder. This is a sling bandage used to immobilize and fix the shoulder joint. The so-called Desault Association is even more stable. Sling and bandages to immobilize the shoulder should not be worn for too long to prevent the joint from stiffening. During shoulder surgery, an abduction pillow is worn for three more weeks after the Gilchrist bandage. This stabilizes the shoulder joint in a slight abduction position, away from the core of the body.
Kinesio tape
A dislocated shoulder should first be treated by an experienced doctor. They will put a bandage on for a short time to keep the shoulder still. After removing the bandage, the shoulder can be taped. The deltoid muscle is followed by two strips of tape, and finally a strip is attached below the roof of the shoulder. The correct attachment of the tape is usually done by a doctor or physiotherapist. A shoulder dislocation, however, often leads to permanent instability of the joint, the tape cannot replace a stable ligament apparatus. In the case of recurring shoulder dislocations, only an operation can lead to permanent healing.
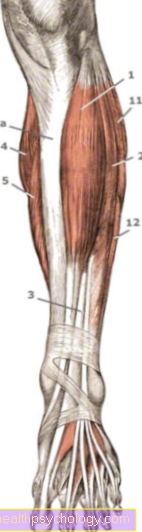
Which exercises can help me stabilize my shoulder?
After a traumatic dislocation of the shoulder joint or in the event of general instability, it is necessary and useful to carry out stabilization exercises in order to reduce the risk of re-injury. It is important to ensure that the exercises are carried out correctly under the supervision of a doctor or physiotherapist. Weights should be avoided immediately after the accident, later on you can use aids such as Thera bands, Pezzi balls or weights. In general, you should strengthen the shoulder joint in every direction of movement of the so-called rotator cuff and initially only use light weights. Exercises are, for example, dumbbell presses while lying down and sitting, side raises, dumbbell rows, rotation exercises on the cable pull or with the Theraband, or the shoulder-width armrest with a Pezzi ball to relieve the legs. In addition to strengthening exercises, stretching exercises from yoga practice can also strengthen the shoulder girdle and prevent injuries. All of these exercises should be carried out under the direction of a trained physiotherapist, trainer or physician and the intensity should only be increased slowly.
Duration and healing for a dislocated shoulder
In many cases, a single traumatic shoulder dislocation leads to permanent instability of the shoulder joint. After a shoulder dislocation, it is important that a shoulder bandage is worn for several weeks. Depending on the type of treatment and the follow-up treatment plan, this can be anywhere from 10 days to 6 weeks. With conservative treatment it is often only 2-3 weeks, with open operations it can be 6 weeks.
The shoulder bandage should also be worn at night for the first 4-6 weeks. It is important that you do not make any active movements of the shoulder joint on your own during this time. The mobilization takes place after consultation or together with a physiotherapist. Above all, abduction (spreading apart) and external rotation movements, as well as movements of the arm behind the body, should not be actively carried out, as this increases the risk of a new dislocation or the outcome of the operation can be damaged.
After approx. 6 weeks with conservative treatment, active movements can be started carefully. First of all, you have to refrain from using and carrying weights! Basically, weights over 10kg should not be lifted with this arm, even in the long term, as there is a risk of them being dislocated again. After an operation, depending on the type of intervention, active movements may only be started from the 7th to 12th week. Previously, only passive and active training with assistance is allowed. Weights over 5kg should be avoided here.
A cure is often only possible through an operation. Weight training can be resumed from the 3rd month after the operation.
How long have I been on sick leave?
If a shoulder dislocation is treated conservatively, i.e. non-surgically, it must then be immobilized for a while and treated with physiotherapy. Especially with physical work, the doctor can put the patient on sick leave for several weeks. A shoulder dislocation can lead to chronic instability, which is why excessive strain should be avoided initially. Recommendations are 6 weeks, during which no weights over 2 to 3 kg should be carried. Shoulder surgery requires immobilization with a sling for about three weeks. Here, too, physiotherapy, strengthening and coordination exercises should be carried out consistently.
In the following weeks, the focus will be on regaining free mobility and strengthening the shoulder muscles. Since healing can take a different course in each patient, the course must be observed individually with the doctor and physiotherapist. Weight training and overhead sports should definitely be avoided in the first 6 months. Ideally, the shoulder can be used almost completely again after half a year. Nevertheless, during shoulder-stressing activities, attention must be paid to pain or unpleasant sensations in the shoulder area, as these can be signs of excessive stress or a possible renewed dislocation.
How long is pain with a dislocated shoulder?
A fresh shoulder dislocation is a very painful process for most patients. The shoulder is held in a relieving position by the person affected. If the dislocated shoulder is not an initial event but occurs again and again and the patient may be able to reposition the shoulder himself, some patients no longer experience as much pain.
The course of the pain depends on the severity of the dislocation. If the ligaments are only slightly stretched, the pain is greatly reduced after 3-4 weeks. If, on the other hand, there are injuries to the cartilage or tendons and ligaments, the pain can last for several months.
After the operation, people often have a pain catheter for 5-7 days, which relieves the pain after the operation. In the following weeks during the follow-up treatment period, the pain ideally decreases from week to week. Typical painkillers such as paracetamol, ibuprofen, Voltaren® and Novalgin® can help here. With all of these painkillers, the intake must be discussed with the doctor.
If the pain does not decrease even with painkillers and conscientious physiotherapy, you can check again whether there is any further damage or whether it has occurred. The general rule here is that in the first few weeks, immobilization and still movement by the physiotherapist are the key to promoting healing. There is a risk of long-term damage with major and repeated dislocations. In this case, omarthrosis (osteoarthritis of the shoulder) can be accelerated, which can cause pain and restricted mobility.
How long should a shoulder be immobilized after being dislocated?
In the case of non-surgical treatment of a dislocated shoulder, the shoulder joint must be immobilized using a so-called Gilchrist bandage. In most cases, it is worn for around two weeks. Here you should follow the doctor's instructions. For about 6 weeks you should avoid external rotation and retroversion (movement sequence as with a handball throw over the shoulder) and do not carry weights over 2 kg. Contact sports such as soccer or handball and weight training should only be resumed after 3 months because of the renewed risk of injury. Mobilization and stabilization exercises should, however, be carried out under the supervision of a physiotherapist at the beginning in order to strengthen the shoulder and prevent permanent movement restrictions.
How long can I not do sports?
Athletes in particular are exposed to a high risk of injury. Since chronic instability of the shoulder joint can occur after a single dislocation of the shoulder, contact sports should be avoided for at least three months. In the first six weeks you shouldn't lift weights over two to three kilograms, external rotation and retroversion (such as handball throwing over the shoulder) should be avoided. Exercises that do not affect the rotator cuff, such as leg training, may be done earlier with caution. Here you should adhere to the medical recommendations. If you are a professional athlete, you are advised to have an operation at an early stage, as shoulder dislocations can usually occur again and again.
Complications
The following complications are possible from dislocating the shoulder:
- Bankart lesion: In the course of the dislocation, the rim of the socket is injured (Glenoid labrum). The Bankart lesion is the most common reason for repeated dislocations after a first traumatic event and must therefore be corrected surgically.
-
Tendon rupture or rotator cuff rupture: These injuries should also be treated surgically, as otherwise shoulder mobility is limited and the joint can consequently stiffen.
-
Hill-Sachs lesion: Particularly when dislocated to the front, bone injuries to the joint head can occur, which can lead to restricted movement and premature arthrosis.
-
Injury to the axillary nerve: Neurosurgical treatment of the nerve should be carried out in order to prevent a loss of function of the shoulder lifter muscle.
-
Stiffening and restricted movement: There is a risk of joint stiffening, especially if the patient is immobilized for too long. This mainly applies to towards the elderly.
- Joint arthrosis in the shoulder joint (Omarthrosis)
Numbness in hand
When the shoulder is dislocated, ligaments, tendons, capsules or nerve tissue can also be injured in particularly severe forms. Damage to the nerve bundle or to vessels in the armpit can lead to circulatory disorders, pain and abnormal sensations such as numbness in the entire arm and hand. If the shoulder is not adjusted again promptly, this can lead to permanent damage. A dislocated shoulder should definitely be examined and treated by a doctor, especially with the symptoms mentioned, in order to avoid permanent limitation.
forecast
Young, sporty patients in particular are often affected by recurrences. Up to 60% suffer further habitual dislocations after a traumatic dislocation. After the operation, the dislocated shoulder seldom (5%) occurs again.
Long-term consequences
A shoulder dislocation can also injure the capsule, ligaments and tendons of the shoulder joint. Often the socket edge of the joint is also damaged, this is called Bankart lesion designated. In over 50% of the cases there are recurrences, i.e. recurrence of shoulder dislocations, even with minor injuries or everyday movements. An operation may be necessary here. A shoulder dislocation increases the risk of osteoarthritis in the shoulder joint, especially in older patients. A shoulder dislocation should be treated medically and treated with physiotherapy in order to avoid permanent movement restrictions.
Shoulder dislocated in the child
In children with shoulder dislocation, a distinction must be made between traumatic or post-traumatic and habitual causes.
The dislocations that are not preceded by trauma or accident are described with habitual. The children can dislocate their shoulder with simple everyday movements. Surgical fixation is recommended here to prevent long-term damage.
In the case of dislocations that recur after a trauma or that have left damage to the cartilage, an arthroscopic operation to secure the shoulder ventrally (anteriorly) is recommended. However, operations on the bones should be avoided here because the growth plates are still open. This must be followed by adequate physiotherapy to strengthen the muscles of the shoulder.
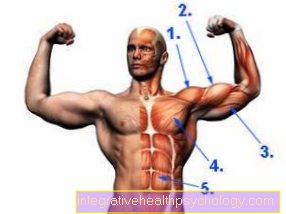
Anatomical basics
The shoulder joint is formed by the upper arm head (joint head), which lies in the joint socket (part of the shoulder blade). The shoulder joint gets its stability mainly from muscles and ligaments. The rotator cuff muscles play a particularly important role here.
However, since the joint head is 3 times larger than the joint socket and there is no bony guidance of the shoulder joint, shoulder dislocation is favored. At the same time, however, this also forms the basis for the large range of motion in the shoulder joint.

- Humerus head - Caput humeri
- Shoulder joint socket -
Glenoid Cavitas - Shoulder blade - Scapula
- Collarbone - Clavicle
- Shoulder corner - Acromion
- Shoulder-collarbone
Joint -
Articulatio acromioclavicularis - Deltoid - M. deltoideus
- Raven beak process -
Coracoid process - Raven beak extension shoulder corner
Tape -
Coracoacromiale ligament - Joint cavity -
C.avitas articularis - Fiber cartilage ring -
Glenoid labrum - Biceps, long head -
M. biceps brachii - Bursa -
Subacromial bursa - Upper arm shaft -
Corpus humeri
You can find an overview of all Dr-Gumpert images at: medical illustrations
Forms of dislocation
A distinction is made between different shapes, depending on how the joint head and socket relate to each other after the shoulder has been dislocated.
Anterior / subcoracoid luxation: The dislocation Forward is the most common form. The head stands in front of the shoulder joint under a protruding bone Scapula (Proc. Coracoideus).
Inferior / axillary dislocation: The head is here below the socket and is towards the armpit postponed.
Posterior / infraspinate dislocation: Here the dislocated shoulder leads to the Joint head behind the joint socket, moved towards the back, stands.
Further very rare forms are: Luxatio superior (up), Erectile luxation (Head is below, arm can no longer be brought to the body), Intrathoracic luxation (Head is pressed into the chest).