Therapy of purulent meningitis
Synonyms in a broader sense
Bacterial meningitis, hood meningitis, convexity meningitis, leptomeningitis, meningococcal meningitis, antibiotic
Medical: purulent meningitis
English: meningitis, encephalitis, brain inflammation, brain-fever
definition
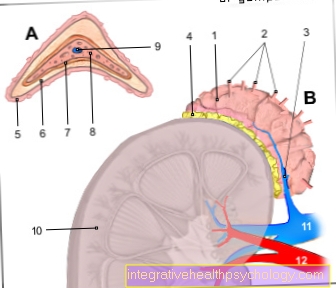
The term purulent meningitis (purulent meningitis) describes a purulent inflammation (-itis) of the meninges and spinal cord membranes (meninges), which can be triggered by different pathogens.
Purulent meningitis (purulent meningitis) is usually caused by bacteria. It is associated with a high fever and severe general clinical picture such as clouding of consciousness and represents an absolute emergency that must be treated immediately.
General information
General information on "What is meningitis?" can be found under our topic:
- Meningitis and
- purulent meningitis
Preface
The therapy of purulent meningitis is usually carried out first, if the pathogen is not known, against the suspected / most likely pathogen and after microbiological detection of the bacterium (this takes a few days until the bacterium can be grown and determined) and an antibiogram (resistance test of the Germ against various antibiotics).
The dosages mentioned are examples that can be treated differently in individual cases.
Despite all the care taken, the drugs mentioned below can contain errors in the dosage or other types of content.
Note: Compliance
Never change the dosage or antibiotic without consulting your doctor. This can permanently damage your health.
Therapy of purulent meningitis
Therapy meningococci
Penicillin G (G = intravenous, i.v.) 4x / day 6-10 mega or
Ampicillin 3x / day 5 g i.v. or
Cephalosporin (Ceftriaxone, Cefotaxime) 3x / day 2 g i.v.
Therapy pneumococci
Penicillin G (if sensitive): 4x / day 6-10 mega or
Cephalosporin (Ceftriaxone, Cefotaxime): 3x / day 2 g i.v. or
Ampicillin: 3x / day 5 g i.v.
Meropenem: 3x / day 2 g i.v.
Penicillin-Resistant Pneumococci
Cephalosporin plus Vancomycin 3x / day 2 g i.v. 2 g / day every 6 - 12 hours
Cephalosporin plus Rifampicin 3x / day 2 g i.v.
Therapy Haemophilus influenzae
Cephalosporin (Ceftriaxone, Cefotaxime) 3x / day 2 g i.v.
alternatively
Ampicillin plus chloramphenicol 3x / day 5 g i.v.
Therapy Listeria monocytogenes
Ampicillin plus gentamycin 3x / day 5 g i.v. or
Trimethoprim-sulfamethoxazole 1x / day 360 mg IV, max. 6 mg / kg or
Meropenem 3x / day 2 g i.v. or
Co-trimoxazole 2x / day 960 mg i.v.
Therapy staphylococci (methicillin-sensitive)
Flucloxacillin 4 - 6x / day 2 g i.v.
alternatively
Vancomycin 2g / day i.v. (every 6 - 12 hours 0.5 - 1 g) or
Fosfomycin 3x / day 5 g i.v. or
Rifampicin 1x / day 10 mg / kg IV, max. 600/750 mg or
Cefazolin 3 - 4x / day 2 - 3 g i.v. (max. 12 g / day)
Therapy staphylococci (methicillin-resistant)
Vancomycin 2g / day i.v. (every 6 - 12 h 0.5 - 1 g) or
Rifampicin 1x / day 10 mg / kg IV, max. 600/750 mg or
Trimethoprim-sulfamethoxazole or
Fosfomycin 3x / day 5 g i.v.
Therapy of Pseudomonas aeruginosa
Ceftazidime plus aminoglycoside 3x / day 2 g i.v. or
Meropenem plus aminoglycoside 3x / day 2 g i.v. or
Cefepime plus aminoglycoside 3x / day 2 g i.v. or
Ciprofloxacin 3x / day 400 mg i.v.
Therapy anaerobes
Metronidazole 2 - 4x / day 500 mg (max. 2 g / day)
Meropenem 3x / day 2 g i.v.
Therapy group B streptococci
Penicillin G plus gentamicin 4x / day 6-10 mega 1x / day 360 mg i.v. or
Ampicillin plus gentamycin 3x / day 5 g i.v. 1x / day 360 mg i.v. or
Ceftriaxone plus gentamicin 3x / day 2 g i.v. 1x / day 360 mg i.v. or
Vancomycin 2g / day i.v. (every 6 - 12 h 0.5 - 1 g)
Therapy Gram-negative intestinal bacteria
Ceftriaxone plus aminoglycoside 3x / day 2 g i.v.
Meropenem plus aminoglycoside 3x / day 2 g i.v.
Source
Poeck / Hacke: Neurologie, 12th edition, 2006 were used as sources.
Despite all the care that we take before a topic is published, we can take care of the information no guarantee take over.