Cortisone
Synonyms
Cortisone, glucocorticoids, cortisone therapy, side effects of cortisone
What is a hormone?
Cortisone (cortisone) is a hormone. Hormones are the body's own substances that are made in various special places. They are transported to their respective destinations through the bloodstream. There they trigger certain reactions through their presence or their absence. That is why hormones are also referred to as messenger substances. What reactions cortisone (cortisone) triggers in the human body and why it is so important is described below.

What is cortisone?
Cortisone (also: cortisone) is colloquially a collective term for a group of substances that are similar in structure and effect, the so-called Glucocorticoids.
Many people are familiar with “cortisone” as a drug. Glucocorticoids can be produced chemically and serve the body as effective ones Medication in a variety of diseases. What is less well known is that the glucocorticoids are endogenous substances and have a vital function in the human body as messenger substances (hormones). In medical parlance, the term cortisone still stands for a very specific endogenous hormone, the first glucocorticoid to be discovered.
Why is cortisone essential for the body?
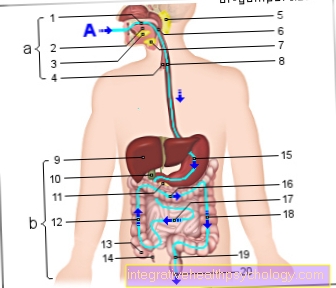
Cortisone (Cortisone) is a hormone that affects the metabolism. It causes the release of energy from the body's reserves. In some situations the body needs energy quickly. The fastest available, but only available in limited quantities, is the Blood sugar (Glucose). First and foremost is the supply of heart, brain and Muscles. Cortisone causes the other organs to temporarily change their energy consumption. These now get their energy primarily from body fat or protein instead of blood sugar. The glucocorticoids got their name from their effect on the glucose (sugar) content of the blood.
"Cortisone" is particularly important in Inflammatory reactions. Inflammation can be caused by injuries, bacteria or intense solar radiation (sunburn) arise. Recognizable and noticeable reactions of the body are usually reddening (rubor), swelling (tumor), heat generation (calor) and pain (dolor) in the affected region. However, the inflammatory reaction is important for the body because it destroys pathogens that have penetrated and renews damaged tissue. The side effect of any inflammation is that surrounding, previously healthy tissue is always affected.
The NF-KB molecule plays the central role in the development of inflammation. It directs u. a. Reactions such as increased blood flow to the affected region (reddening), constriction of the vessels (swelling) and sensation of pain in the way. This is where cortisone comes in. It puts NF-KB out of action. Without NF-KB, pronounced inflammation cannot occur. Thus the destructive dimensions and the pain usually associated with it are kept within limits. That is why the use of cortisone as a drug is of great importance, especially for all types of inflammation.
Furthermore, cortisone plays an important role in the functionality of the body Defense system. If a person is under stress for a long time and has to remain fully operational, his body must not allow itself to become ill. For this reason, cortisone can, to a certain extent, affect the body’s defense system (immune system) suppress. Pathogens may be in the body, but the immune system does not recognize them.
Furthermore, cortisone also has an influence on blood pressure (high blood pressure), the sleep-wake rhythm and is therefore vital for humans.
Cortisone as a drug
Because of their effect on the immune system and on inflammatory reactions, the glucocorticoids are very effective drugs in a variety of diseases that are associated with inflammation, pain or overreactivity of the immune system.
Supplied to the body from the outside as a drug, glucocorticoids strengthen the effect of the body's own cortisone. The higher the dose, the stronger the effect.
Effects of cortisone

Cortisone acts on the DNA and activates or inhibits certain genes that control processes in the body. It therefore takes a little time before the desired effect occurs at the destination. This must be taken into account when using cortisone as a drug. Depending on the preparation, the onset of action can be between 15 minutes and days. But the effect is all the more sustainable.
Overview: areas of application
- All kinds of inflammation
- Inflammatory rheumatic (joint) diseases
- Skin diseases
- asthma
- Allergies
- Autoimmune diseases
- In high doses as emergency medication allergic shock
- Malfunction of Adrenal gland
- Insect bites
- Transplants to suppress the Immune system
Instructions for use
It is best to take the medication early in the morning (6 a.m. - 9 a.m.). This corresponds to the natural rhythm, since the body's own hormone production is at its highest during this period.
Therapy with cortisone (cortisone), especially long-term therapy, should never be stopped without consulting a doctor. The reason is, on the one hand, that the body's own cortisone production can decrease through the supply from outside. If the treatment with cortisone is stopped abruptly, the body cannot start producing again as quickly. Most of the time, this makes the disease worse. Depending on the patient's state of health, cardiac arrhythmias and circulatory problems can occur if the patient is stopped suddenly.
What should you know about taking cortisone?
Cortisone (cortisone) is a very powerful drug. Since its discovery and the resounding success associated with it in the treatment of many previously untreatable diseases, cortisone has hit the headlines, particularly because of its serious side effects. It has now been recognized that dosage and duration of treatment are critical to the occurrence of side effects.
Info: stopping cortisone
The withdrawal of a cortisone preparation takes place gradually in order to stimulate the body to produce again and to prevent withdrawal symptoms.
If you have the feeling that your cortisone preparation is not the right one for you or if you have problems with the application / dosage, please consult your doctor!
Please also read our topic: Discontinuation of cortisone
When are side effects to be expected?
In general, the following applies to treatment with cortisone: As much as necessary, as little as possible! The risk of side effects increases
- the longer the treatment period
- the greater the distribution in and on the body
- the higher the dosage
Short-term treatment (3 - 4 weeks) is usually harmless. The same applies to long-term (i.e. more than 4 weeks) but low-dose use. The likelihood of undesirable side effects occurring is relatively low. The risk increases if long-term use in high doses is required, depending on the severity of the disease.
When cortisone is administered in tablet form or as an injection into the bloodstream, it is desirable to have an effect in many areas of the body. However, side effects can occur due to the large-scale distribution. This also applies to external use of cortisone preparations. Therefore, a cortisone cream should only be applied to the affected areas of the skin and not generously on the peripheral areas.
In cortisone treatment, it is therefore desirable to place the lowest possible but effective dose exactly in the diseased region. Nowadays there is a multitude of modern forms of application available that make this possible and make therapy efficient.
Whether a dosage should be assessed as “high” depends on the type of glucocorticoid chosen for therapy. A wide range of glucocorticoids have now been artificially produced. This enables your doctor to tailor the drug therapy exactly to your illness and thus to keep the side effects low.
Application forms
The application can be internally and externally as
- Tablets
- Injections into the bloodstream
- Asthma sprays / inhalers for lung diseases
Read more about this under: Cortisone spray - So-called crystalloid injections for joint diseases
- Ointments / creams for skin diseases
- Nasal sprays
- Eye drops / eye ointments
- as a cortisone spray
- Cortisone injection
Cortisone ointment
Cortisone ointment is used for numerous skin diseases. However, the cream, known colloquially as cortisone ointment, is usually an ointment that does not contain cortisone but other active ingredients from the group of corticosteroids.
An example of such an active ingredient is mometasone. Ointments containing mometasone are used for skin diseases such as psoriasis or eczema and are used for relief. As an example, Momecutan 1mg / g ointment should be mentioned here, which can be purchased in pharmacies with a prescription.
Ointments that actually contain hydrocortisone are used for mild skin irritations, for example for mild allergic reactions. Possible side effects of ointments containing cortisone or stronger agents from the group of corticoids are slight burning when applied to the affected area, thinning of the skin with regular use, tingling sensations in the area where the ointment was applied and red spots or streaks on the skin. Discoloration of the skin (purple or dark blue) can also occur.
Furthermore, bacterial superinfections can occur. This means that after some time of use, in addition to the inflammation, bacteria will settle in the area and an infection will occur. In addition, the skin can dry out and hair growth can increase.
Read more on the topic: Cortisone ointment
Nasal spray with cortisone
Similar to ointments, nasal sprays contain various active ingredients from the group of corticosteroids in spray form. For example Mometason nasal spray, better known under its trade name Nasonex®. It can be used to treat allergic rhinitis, for example in the context of hay fever or polyps in the area of the nose and sinuses. With polyps, 2 sprays per nostril should be taken twice a day, with hay fever once a day two sprays per nostril.
Another example of a cortisone derivative in nasal spray form is fluticasone. It is used for hay fever. Again, 1-2 puffs are recommended once a day. The nasal spray is available from the pharmacy without a prescription.
When using a nasal spray with ingredients similar to cortisone, side effects can occur. These include irritation in the nose and throat, dehydration of the nasal and pharyngeal mucous membranes, nosebleeds, the formation of ulcers in the nasopharynx, headaches and odor or taste disorders. It should not be used with known hypersensitivity to any of the ingredients.
Read more on the topic: Nasal spray with cortisone
Cortisone used to treat allergies
Cortisone is mainly used to treat inflammatory reactions. But it is also used for some forms of allergy. In local form, cortisone or similar active ingredients are used, for example, for allergic skin reactions as a skin ointment or as a nasal spray for hay fever. However, this does not cure the underlying disease, but rather serves to contain the symptoms such as itching, burning eyes and allergic rhinitis.
Cortisone derivatives are also used to curb strong acute allergic reactions. An example of this is allergic shock. This can be triggered, for example, by an insect bite or food. In such situations, rapid action is required, as so-called anaphylactic shock can occur, which is life-threatening. With strong allergic reactions, cortisone or prednisolone can be used in high doses.
Antihistamines and, if necessary, adrenaline are also used. When using a high dose of cortisone preparations once, there are usually no side effects.
Shock therapy with cortisone
A cortisone shock therapy means that very high doses of cortisone are administered over a period of several days. With classic cortisone shock therapy, this is usually 1000 grams of methylpredisolone. Prednisolone is an active ingredient from the same group of drugs as cortisone. This type of cortisone shock therapy is used, for example, to treat multiple sclerosis. However, lower doses of cortisone derivatives that are administered over a few days can also be referred to as shock therapy in the broader sense.
Indications here are, for example, lung diseases, rheumatic diseases, chronic inflammatory diseases of the intestine such as Crohn's disease or allergic skin diseases. In the first few days, doses such as 100 mg prednisolone are usually used. In the following days the dose is then reduced relatively quickly and then either stopped entirely or continued at a very low dose.
Cortisone preparations cause numerous side effects with prolonged use, but with short use they are relatively well tolerated, even in high doses. However, stomach pain, nausea, vomiting, and restlessness can occur. Such side effects are possible, particularly with very high doses.
Side effects
The occurrence of side effects and their severity depend to a large extent on the nature of your illness, the duration of treatment, the glucocorticoid chosen for therapy and the required dosage. But they can usually be treated well. The nature of the side effects is usually closely linked to the actual function of the cortisone in the body. The following side effects have been observed in association with glucocorticoid therapy:
Possible side effects with internal (systemic) use:
- Sleep disorders, nervousness, mood swings
- a headache
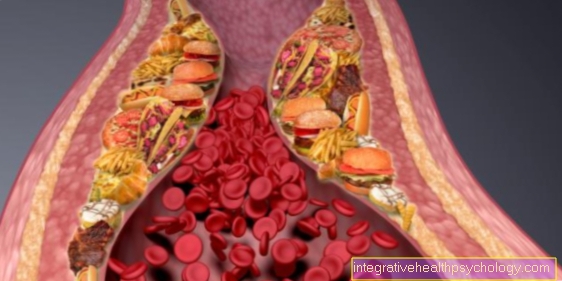
- Increased blood sugar level, diabetes: Cortisone promotes the breakdown of body reserves for blood sugar. Sometimes the pancreas is overwhelmed and cannot provide enough insulin to break down blood sugar. Therefore, pay attention to increased thirst and urination and, if necessary, consult your doctor!
- Weight gain: Long-term use can result in increased appetite. To prevent weight gain, pay attention to your weight and a balanced diet.
- Osteoporosis: You can prevent this by eating a calcium-rich diet. With long-term cortisone therapy, the additional intake of calcium tablets and vitamin D3 makes sense.
- increased susceptibility to infection
- Stomach and intestinal ulcers
Side effects when using inhalers:
- hoarseness
- Infections: Long-term use of inhalers can cause fungal infections and / or bacterial infections in the mouth and throat. As a preventive measure, rinse your mouth after using an inhalation spray.
Side effects when used on the skin:
- the skin layer becomes thinner and more sensitive (skin atrophy)
- small blood vessels just under the skin expand and become visible (telangiectasia)
- Steroid acne, similar to common acne
- delayed wound healing
Side effects when used on the eye:
- slight burning of the eyes
- Veil vision
- increased intraocular pressure (green star = glaucoma))
- Cornea becomes thinner
- Cataracts
For long-term, high-dose use, please visit an ophthalmologist occasionally.
Read more on the topic: Eye ointment with cortisone
Side effects when injecting into joints (intra-articular injection) e.g. in knee osteoarthritis, back pain, facet syndrome and on tendons and ligaments e.g. Tennis elbow, heel spur:
- Feeling of pressure at the injection site
- Injury to nerves and vessels from the injection
- Injury to ligaments and tendons (risk of rupture)
- Development of an infection in the treated joint
Read more on the topic: Side effects of cortisone
Withdrawal from cortisone- what should be considered and what are the consequences?
The discontinuation of cortisone becomes a problem primarily if it has been taken over a long period of time, in high doses and systemically. Systemic means that the application takes place in such a way that it affects the whole body. This is the case, for example, when taking cortisone preparations in tablet form.
When used locally, for example as a nasal spray or ointment, discontinuation is not that big a problem.
However, if cortisone preparations have been taken over a longer period of time and in higher doses than tablets, the tablets should not be discontinued immediately but the dose should be slowly reduced.
The reason for this is as follows: The body produces cortisol itself in the adrenal cortex. If, in addition to the body's own production, cortisone is supplied from the outside, i.e. in tablet form, the body believes there is too much or enough cortisone and reports this to a control center in the central nervous system. This message means that the body's own cortisol production is significantly reduced.
If this is the case over a longer period of time, for example with cortisone therapy over months or years, the adrenal cortex slowly recedes because the cells that produce cortisol become less and less. So what is known as adrenal cortex atrophy occurs.
If the cortisone tablet is suddenly discontinued, there is an acute shortage of cortisone because the “sleeping” adrenal cortex cannot react as quickly. This can have life-threatening consequences. It is therefore important to get the adrenal cortex used to the fact that it has to start producing again. For this, the dose of cortisone tablets is slowly and gradually reduced.
The attending physician must decide how and at what intervals the dose is reduced. If cortisone is tapered off slowly enough, there should be no undesirable side effects as part of the withdrawal. If it is tapered off too quickly or even stopped abruptly, it can lead to circulatory crises with possible fatal consequences. Therefore, patients who have been taking cortisone preparations over a long period of time should never stop taking their tablets on their own initiative.
Cortisone and alcohol - are they compatible?
Basically, the rule applies that with regular medication consumption, alcohol consumption should only be very controlled.
For drugs from the group of corticosteroids, including cortisone, the higher the cortisone dose, the lower the alcohol consumption should be, as otherwise cortisone can cause undesirable effects or a weakened effect.
Since the long-term intake of higher doses of cortisone is already fraught with numerous possible side effects, alcohol consumption should therefore be avoided or severely restricted as possible. In addition, many patients who have to take cortisone or prednisolone report that they suddenly no longer taste the alcohol at all or that they can no longer tolerate it well. In principle, the treating family doctor should be asked whether alcohol consumption is permitted in moderation, as it also always plays a role which medication is taken in addition to cortisone.
Read more on the topic: Are cortisone and alcohol compatible?