Can I breastfeed if I have a fever?
Fever per se is not a reason against breastfeeding. In each individual case, however, it depends on why the mother has a fever. With a slight flu-like infection, a woman can continue to breastfeed her child without hesitation and should only pay more attention to the observance of simple hygiene measures such as frequent hand washing. However, if the mother suffers from a fever as a result of a serious consuming illness that requires special drug therapy, she may not be able to breastfeed her child for the duration of the treatment. In general, affected women should consult their gynecologist if they are unsure whether or not they can continue breastfeeding their child.
You might also be interested in this topic: How dangerous is a cold while breastfeeding?

Can I breastfeed if I have a fever?
In principle, mothers with a fever are allowed to breastfeed. From a purely objective point of view, fever is only an increase in body temperature above an average normal value and not a disease. Rather, it is to be seen as an indication or a symptom of a disease. Breastfeeding women do not have to worry about whether or not they are allowed to continue breastfeeding if they have a single fever. As long as they do not classify themselves as seriously ill, mothers can and should breastfeed their children, as experience shows that the child, like the mother, has come into contact with pathogenic bacteria or viruses and valuable antibodies and trace elements are transmitted from the mother through breast milk.
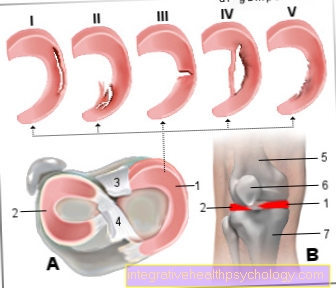
It only becomes critical when other symptoms such as painful swelling and redness appear on the chest. Then a nursing mother should go to the gynecologist and have a specialist clarify whether or not further breastfeeding with the affected breast is possible. Self-experiments with regard to therapy should be avoided here, as the glandular tissue of the breast is very sensitive to bacteria and external manipulations during breastfeeding. In addition, the breast is the contact point for the child, where it ingests the maternal pathogens from the normal skin flora with its mouth. If this is changed by an infection or an independent application of ointment, the child is exposed to an unnecessarily high level of pathogens or foreign substances.
Another reason not to breastfeed if you have a fever is taking medication at the same time. Especially when treating a bacterial infection with antibiotics, women should express and discard the milk, as the active ingredient can pass into the breast milk. Depending on the age of the child, the breast milk can be dangerous for the affected child, as its liver may not be mature enough and cannot metabolize the active ingredient. The effect on the child would therefore be potentially toxic or, in other words, organ damage. Substitute milk should therefore be given for the duration of the intake. Regular expressing of the breast milk is very important, despite the discarding, so that breastfeeding can continue after the end of the therapy. For example, if a breastfeeding woman does not pump for the period of antibiotic therapy (based on experience up to about a week), milk production will dry up. Even by breastfeeding again, milk production can no longer be increased.
You might also be interested in this topic: Maternal problems while breastfeeding and breastfeeding despite a sore throat
Which antipyretic drugs can I take?
In general, it is recommended to breastfeeding mothers first of all to lower the fever with non-drug measures, as these have the fewest side effects for themselves and their child. However, should a woman feel the need to reduce her high fever with medication, she should choose an active ingredient that is not only temperature-lowering, but ideally also anti-inflammatory, as she is most likely suffering from a high fever due to an infection. Ibuprofen is most likely to be recommended for this. However, breastfeeding mothers should adhere to the exact dosage and not exceed the recommended daily dose. In addition, the drug should not be taken longer than absolutely necessary.
Further information at: Ibuprofen while breastfeeding
If there is an allergy to ibuprofen or if the temperature cannot be reduced sufficiently with it, paracetamol can serve as an alternative. However, it is more of the second choice, with the same conditions of use as for ibuprofen. If the above medication does not lower the fever, you should not take other active ingredients on your own. Then it is important to find out the cause of the fever during a medical examination and to adjust the therapy as required.
Read more on the topic: Medication during breastfeeding
Paracetamol
Paracetamol in itself is a pain reliever. It can also be used well to lower fever. The usual form of administration are tablets with a dose of 1000 mg per tablet. A daily dose of 4g (4000mg = 4 tablets per day) should not be exceeded, as this can lead to liver damage. For breastfeeding mothers, it is advisable to take 500mg if there is a fever and possibly to take it again at a time interval of six hours in order to keep the active ingredient from getting into breast milk as little as possible.
Breastfeeding for chest pain
"Puerperal mastitis" is a common disease in breastfeeding women and occurs preferably in the second week after giving birth. Often the affected woman first notices reddening and swelling of the affected breast, whereby the symptoms are supplemented by pain during breastfeeding. In the further course, fever often occurs. With this disease, it is particularly important that there is no accumulation of secretion in the affected breast. For the nursing mother, this means consistently and regularly expressing and discarding the milk from the affected breast.
However, she may continue to breastfeed her child on the unaffected breast. The reason for discarding the breast milk on the affected breast is the possible high germ content. Bacteria on the skin are responsible for the inflammation of the mammary gland, which infect the glandular tissue through small microtraumas in the skin on the breast. During the breastfeeding process, the pathogens are flushed out of the milk duct system. If the child were to drink this milk, it would be exposed to a high level of pathogen. If the symptoms in the breast have subsided, the mother can also breastfeed with this breast again.
Find out more about the topic: Inflammation of the nipple
Can I breastfeed if I have a cold?
A cold is usually caused by viruses and is limited to a few days to a maximum of two weeks if the course is mild. As long as a breastfeeding mother has no evidence of an unusually long or serious course of the disease, she can continue to breastfeed her child. Accompanying symptoms such as a sore throat, headache or tiredness are also no reasons to pause breastfeeding. Rather, the breastfeeding woman should be aware that she is supplying important antibodies to the child through her breast milk despite the common cold.
With these antibodies, the child can cope better with an existing infection and possibly be protected from it. A child simply cannot be protected from all pathogens in the environment or in the immediate vicinity. It is even part of the maturation of his immune system to deal with various pathogens. A mother should just not provoke contact with pathogens and should react appropriately to signs of illness in the child and consult a doctor if necessary.
Find out all about the topic here: Breastfeeding with a cold.
What can I do to avoid infecting my baby?
A baby gets infected from its mother the same way that the mother infected herself from someone else. Thus, every breastfeeding woman who has a feverish infection is recommended to observe simple hygiene measures. The mother should therefore not sneeze at or cough at her child directly and should not leave used handkerchiefs in the immediate vicinity of the child. Regular hand washing is also recommended in order to minimize the possible attachment of the pathogen to the palms of the hands. However, pathogens are also found in the nose and mouth area, especially in colds. Kissing the baby or “rubbing their noses together” should therefore be avoided while the patient is suffering from acute symptoms. This keeps the risk of droplet and smear infections as low as possible.
Nevertheless, the child should continue to be treated lovingly and breastfeeding should be continued with the necessary and desired physical contact. It should just be clear that the child should not be brought into contact with pathogens unnecessarily often and too much. In any case, the child will come into contact with the pathogens, which also leads to the training of his immune system. In addition, breastfeeding mothers must not assume that they only transmit the pathogens to the child through their breast milk. In the breast milk they also give the child antibodies that protect it from the pathogen.
Read more on the subject at: How dangerous is a cold while breastfeeding?
Additional information
- Problems in breastfeeding in the child
- Problems during breastfeeding in the mother
- Medication during breastfeeding
- Alcohol while breastfeeding
- How should I behave while breastfeeding?



.jpg)