inflammation
introduction
Inflammation can be understood as a sign of the activation of the immune system.
The reason why the immune system is activated varies from person to person. Pathogens, foreign substances, injuries and the presence of an autoimmune disease are possible causes which can be responsible for the occurrence of inflammation.
The immune reaction, which usually manifests itself with symptoms such as swelling, reddening, overheating and pain, is supposed to eliminate the cause of the inflammation. This is a very complex process which involves the activation of different systems.
Almost every part of the body and organ can be affected by inflammation. A distinction is made not only between the different localizations of inflammation, but also according to the time course (chronic vs. acute) of the disease. The different components of the inflammatory fluid also serve to differentiate between the types of inflammation.

What is inflammation?
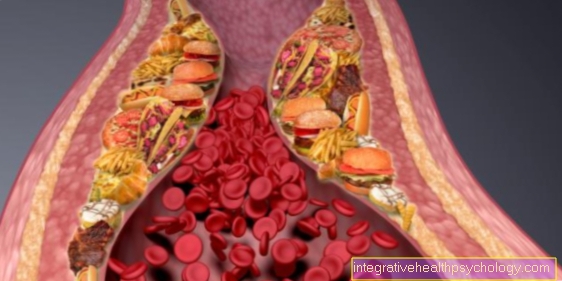
An inflammation, in medical parlance marked with the ending -itis (Hepatitis, tonsillitis), is a naturally occurring reaction of the body to a harmful external or internal stimulus with the aim of eliminating this influence. It is an expression of a pronounced activation of the immune system and is intended to initiate the healing process. The background to this is that the inflammatory reaction slows down the blood flow in the affected area and increases the permeability of the vascular walls, so that immune cells can flow into the affected area and fight the trigger. This can be seen in the swelling and reddening, and the overheating also improves blood circulation. Pain ensures that the damaged part of the body is further spared. These mechanisms are supported by a very complex interaction between messenger substances and cells of the immune system.
Inflammation can be localized to a part of the body, an organ or a body region, or it can run systemically throughout the body. Inflammation can be differentiated into bacterial, viral or abacterial according to the triggering factors. In addition, it is divided into acute or chronic inflammation according to the time course and according to the type of fluids that leak into serous, purulent or fibrinous.
In general, any stimulus that goes well beyond normal levels can cause inflammation, such as also extreme temperatures or trauma. The most common is bacterial inflammation. Bacteria could get into the body through wounds or other body openings, multiply and cause inflammation. Sometimes they get to other areas via the blood. The bacterial inflammation is characterized by the formation of pus, which mainly consists of destroyed bacteria and burst immune cells, especially macrophages. Examples are inflamed cuts or otitis media, but pneumonia or urinary tract infection is usually a bacterial infection.
Viruses can also cause inflammation, which is often less acute than bacterial, but sometimes more difficult to treat because viral inflammation does not respond to antibiotics. Examples are inflammation of the eye and in the ENT area. An acute cold with runny nose and sinusitis is mostly viral. A well-known internal viral inflammation is hepatitis. If the inflammation is abacterial, or better said sterile, no pathogens are responsible for the damage. Causes such as heat, cold, bruises or allergic reactions to foreign material in the body come into consideration. Basically, any excessive stimulus can activate the immune system and trigger inflammation.
Levels of inflammation in the blood
In addition to the externally visible signs, inflammation also causes changes in certain blood values. A doctor can usually use these values to determine whether there is inflammation in the person's body.
A well-known blood value, the concentration of which is always checked in the blood if there is a suspicion of inflammation in the body, is the so-called C-reactive protein (CRP value).
It is a protein that is formed in the liver and, as part of the immune system, increases in the body when there is inflammation. The CRP is a relatively unspecific value, since the CRP can be used to identify whether an inflammation is present in the body, but it is hardly possible to differentiate between the causes of the inflammatory reaction and their location.
Would you like to know how you can lower your CRP value? - Then read the following article How can I lower my CRP value?
The sedimentation rate (ESR) can also help determine inflammation of a non-specific nature. The time it takes for the solid blood components to drop in a standardized test can provide an indication of an existing inflammation.
A detailed examination of the white blood cells (leukocytes) can be more specific. These are an important part of the immune system. In addition to the absolute number of these cells, the distribution of the number of different leukocytes can provide an indication of whether, for example, parasites or bacteria are responsible for the inflammation.
Finally, the so-called procalcitonin can also provide an indication of the cause of the inflammation. If this value rises sharply, this indicates the presence of an inflammation of a bacterial origin.
Read more on the topic Levels of inflammation in the blood
Signs of inflammation
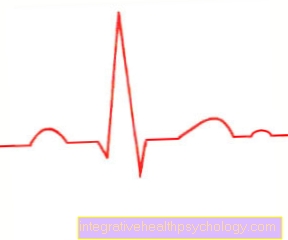
The classic way of inflammation is the 5 signs of inflammation redness (Rubor), Overheat (Calor), Swelling (tumor), Pain (Dolor) and limited function (Functio laesa) noticeable.The following can be observed: One of the first signs of inflammation is a rapidly developing reddening of the skin, which is a sign of increased blood flow. Due to the better blood circulation, you can detect overheating of the affected area with your bare hand. Over time, the affected tissue swells quickly, a partially visible bump develops and the skin begins to stretch. As a further sign of inflammation, inflammation sometimes causes severe pain, which is sometimes described as throbbing / stabbing at the same time as the pulse. Eventually the sign of inflammation of the functio laesa develops. This means that due to the pain and swelling, the affected area can no longer be used to the normal extent, which is to be understood as a protective function of the body. For example, if you cut your finger and develop a local inflammation, you can no longer use this finger fully, as pressure and movement trigger pain, and speaking is difficult in the context of a sore throat. This is to prevent an increase in the damage.
In addition to these typical signs of inflammation, there are other symptoms that can occur in parallel with the inflammation. This can lead to the visible formation of pus from a wound, which drains or can be squeezed out. If the inflammation is major or internal, the result is fever in most cases. This can e.g. severe pneumonia also exceed 40 ° C. In addition to these clinical signs, other signs of inflammation can be determined in the doctor's office or in the hospital. The blood test reveals an increased number of white blood cells, which represent the body's defense cells. These are increasingly produced to fight inflammation. A commonly used marker for inflammation that is not obvious is C-reactive protein (CRP), a routine parameter in internal medicine. Pro-calcitonin (PCT) is specific for bacterial inflammation.
What are anti-inflammatories?
The concept of the so-called Anti-inflammatories describes a Drug group, which can relieve the symptoms of inflammation. Those contained in the medication Active ingredients differ but sometimes very different from each other, which is why the way in which the drugs inhibit the inflammation is very different. The areas of application can also differ from one another, depending on the active ingredient group.
The number of different anti-inflammatory drugs is very long. Best known are anti-inflammatories of the group called non-steroidal anti-inflammatory drugs, too NSAIDs called. These drugs belong to their group acetylsalicylic acid (Aspirin®), Ibuprofen or Diclofenac count, inhibit the production of certain substances which, among other things, are responsible for the symptoms of inflammation. If the inflammation is severe, immunosuppressants can be used, which inhibit different components of the immune system.
When is it necessary to take antibiotics?
At Antibiotics are drugs which either the Inhibit bacterial growth or the Attack bacteria themselves. Antibiotics can therefore help treat a number of different inflammations successfully. However, care must be taken to ensure that antibiotics only help if the inflammation is caused by bacteria.
If not bacteria, but for example a Virus or foreign matter responsible for the inflammation taking antibiotics will not help treat them.
To find out whether it is actually a bacterial infection you should Consulted a doctor become. With the help of the anamnesis as well as the physical examination and the analysis of specific inflammation values in the blood, this can determine whether it is a bacterial inflammation and whether it makes sense to take antibiotics in the individual case.
There Antibiotics always require a prescription Once the diagnosis has been made, the attending physician can prescribe a suitable drug. If necessary, a sample of inflammatory cells must be taken in order to adjust the antibiotic medication during the course of treatment.
Inflammation in the human body
In addition to an externally visible inflammatory reaction, inflammation can also take place in the body. Depending on how and where the inflammation takes place, this can be an expression of serious clinical pictures, or it can be more insidious and without clear symptoms. Almost every organ system in the body can be affected, the urinary tract, lungs, intestines or joints are often affected. The inflammation can also spread to other systems. In addition to the specific symptoms in each case, inflammation in the body also manifests itself through symptoms such as fever or chills, and patients feel sick and poor performance. A severe course of inflammation in the body is that sepsis. This is an inflammatory reaction that occurs throughout the body and is caused by bacteria and can be potentially life-threatening. To clarify whether there is inflammation in the body, the doctor can consult parameters from the blood in addition to the clinical examination. Inflammation is shown here by an increase in white blood cells and an increased C-reactive protein (CRP), chronic inflammation can also lead to anemia.
Inflammation in the mouth
Inflammation in the mouth can occur in different places and can be caused by a number of different causes.
Often it is inflammation of the gums and mucous membranes that occur in the mouth. Any inflammation in the mouth can be caused by bacteria, viruses or certain fungi.
Injuries and allergic reactions can also cause inflammation of the oral cavity. There is also often inflammation of the mucous membrane, which becomes noticeable with the development of so-called canker sores. These are very painful, white-yellowish spots on the oral mucosa. Aphthae are very painful to the touch, you can see a small local reddening with a grayish center. It is not known exactly how it develops; some people suffer more from canker sores than others. This inflammation in the mouth is harmless and will heal on its own after a few days. Ointments or lozenges that contain local anesthetics can relieve the pain.
Infection with a herpes virus can also cause uncomfortable inflammation in the mouth.
Read more on the topic Herpes in the mouth
In order to prevent inflammation in the oral cavity, good oral hygiene should generally be observed and injuries within the oral cavity avoided. Depending on the underlying cause, inflammation can be treated with antibacterial drugs, antiviral therapy or symptomatically.
Since inflammation of the oral cavity is usually associated with severe pain, pain-relieving medication can alleviate the symptoms. You should also avoid very acidic or spicy foods, as these can aggravate the pain.
Furthermore, other pathogens can cause inflammation in the mouth, above all fungi. Here you can see a whitish coating in the mouth. Fungal infections in the mouth should always be examined and treated by a doctor as they can be the expression of an underlying, more serious illness.
Inflammation of the gums
In addition to the development of tooth decay, inflammation of the gums is a relatively common reason for a visit to the dentist. The main cause of the inflammation on the gums is poor oral hygiene. Dental plaque or tartar can settle in places that are difficult to reach with a toothbrush, which serve as a good breeding ground for bacteria and can lead to gum inflammation. Gum infections are usually caused by bacteria and affect the externally visible tissue that surrounds the tooth. Inflammation of the gums typically shows signs of inflammation such as redness and swelling, and frequent bleeding of the gums, for example when brushing your teeth, can also occur. On the other hand, gingivitis is usually painless.
Even without bacterial overgrowth, the plaque causes the surrounding tissue to be affected and an inflammation of the gums due to chronic irritation develops. Symptoms of inflammation in the gums include pain and a noticeable reddening, and in some cases the gums may start to bleed.
Removing food particles from between the teeth and maintaining regular oral hygiene can help prevent gum infections. In addition to brushing your teeth, you should regularly floss the spaces between your teeth to clean hard-to-reach areas. In the event of inflammation, antibacterial mouthwashes are also used. In addition, a six-monthly visit to the dentist and a tartar removal should not be missing. Professional teeth cleaning, as well as the removal of tartar, can be suitable therapy methods to prevent the inflammation from recurring.
Viruses, fungi and injuries to the gums are less often responsible for inflammation of the gums.
Read more on this topic at: What helps with inflammation of the gums?
Inflammation of the pancreas
Inflammation of the pancreas, known as pancreatitis in medical terminology, can take an acute as well as a chronic course.
Acute inflammation of the pancreas is often caused by diseases of the gallbladder, such as the presence of gallstones. In acute inflammation of the pancreas, the ducts of the gland are blocked. The enzymes that the pancreas normally secretes into the intestines now remain in the gland and the organ starts to digest itself. Since the pancreas can be severely damaged in an acute inflammation, an acute pancreatitis is a life-threatening disease which must be treated acutely.
Chronic pancreatitis, on the other hand, is largely caused by excessive alcohol consumption. However, since not all alcohol-dependent people suffer from chronic inflammation of the organ, alcohol abuse is only believed to be part of the causes of the inflammation. The exact background of the development of the disease The symptoms of pancreatitis have not yet been fully clarified. are primarily severe pain, nausea and vomiting, sudden food intolerance, pain after eating, changes in stool and diarrhea. In the chronic course these symptoms are milder, but there is always recurring pain. Chronic inflammation of the pancreas in particular can also lead to a loss of function of the pancreas, leading to fatty stools, diarrhea and various food intolerances. These patients can also develop diabetes mellitus.
Read more on this topic at: Symptoms of inflammation of the pancreas
One of the main causes of inflammation of the pancreas, especially in the chronic form, is excessive and long-term alcohol consumption, while acute pancreatitis is often caused by an obstruction of the ducts of the pancreas, e.g. gallstones. But infectious, autoimmune or genetic causes can also cause pancreatitis. The diagnosis is made clinically and by imaging procedures such as ultrasound or CT, and the measurement of enzymes such as amylase and lipase supports the diagnosis. The acute inflammation of the pancreas is treated with intravenous fluids and painkillers, gallstones may be removed or antibiotics given if infected. The therapy of the chronic form consists mainly of alcohol abstinence, painkillers and the administration of pancreatic enzymes should the production of these be restricted.
Read more on this topic at: Therapy of pancreatitis
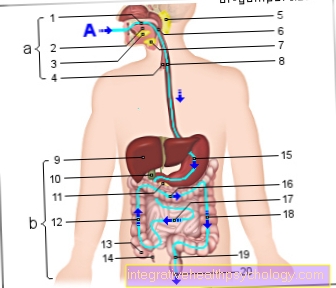
Inflammation in the intestines
Inflammation in the intestine is a very common occurrence that can be caused by various clinical pictures. The best known is inflammation of the small intestine, which is also known as enteritis. Viruses or bacteria, but also fungi or the ingestion of toxic substances are often the cause of the inflammation of the small intestine. Diarrhea, nausea, and vomiting are typical symptoms of bowel inflammation. Children are more often affected than adults.
The most common inflammation in the intestine and one of the most common reasons for a doctor's visit is acute appendicitis. It is noticeable by pain in the right lower abdomen and requires rapid intervention; the appendix is usually removed surgically. Strictly speaking, it is not the appendix, a part of the intestine shortly after the transition from the small intestine to the large intestine, that is inflamed, but an intestinal appendage of it. The equivalent of inflammation in the intestine to that in the left lower abdomen is diverticulitis, which mainly affects the elderly. The inflammation takes place in pouches in the large intestinal wall, since bacteria can settle here particularly well. This type of inflammation in the intestine is treated conservatively with antibiotics.
In addition to acute inflammation, there is also chronic inflammatory bowel disease (IBD), which is not uncommon in an internal medicine ward and increasingly affects young women. These include Crohn's disease and ulcerative colitis. These are autoimmune diseases in which the immune system is directed against the body and causes inflammation in the intestines for reasons that have not been fully understood. While ulcerative colitis is limited to the large intestine, Crohn's disease can theoretically affect the entire digestive tract from mouth to anus. Abdominal pain, sometimes bloody diarrhea and, if the disease progresses, fistulas, intestinal obstruction or colon cancer can occur. IBDs are treated with medication with steroids and immunosuppressants, ulcerative colitis can even be cured by removing parts of the intestine. However, this is the last resort.
Inflammation of the eye
A wide variety of inflammations can affect the eye. The eye is made up of a number of different structures, and inflammation can affect one or more of these structures.
The causes are often bacteria or viruses, but also allergic reactions. Probably the most common inflammation of the eye is the so-called conjunctivitis (conjunctivitis). It is usually characterized by pronounced itching, redness and a strong sensation of foreign bodies in the eye. If the cornea is inflamed, visual impairment can also occur.
Inflammation of the eyelid is colloquially known as stye (hordeolum) or, if a sebum gland clogs up in the area of the eyelid, it is known as hailstone (chalazion). The hailstone is a slowly developing inflammation of the eye with swelling without pain, which usually does not require any specific treatment. The stye, which is painful in contrast, is caused by bacteria and should be treated with an antibiotic ointment. Allergic reactions are often associated with reddening of the eye and increased tear production. In general, inflammation of the eye of unknown cause should be clarified by an ophthalmologist in order to avoid serious complications.
The lacrimal glands can also be affected by inflammation in the eye. Bacteria are also the cause here; mumps, mononucleosis or flu can also lead to inflammation of the lacrimal glands.
Some diseases such as inflammatory bowel disease or rheumatic events are often associated with inflammation of the choroid membrane on the eye, one speaks of Uveitiswhich can lead to some complications and should therefore be treated by a doctor. It can be subdivided into anterior, intermedia and posterior uveitis and can be viral or bacterial. Symptoms are dull pain, a red eye and photophobia, and visual acuity may decrease.
What might also interest you: Pain in and around the eye
Inflammation in the knee
An inflammation in the knee is a common reason for a visit to the family doctor or an orthopedic department, med. Called gonarthritis.Inflammation of the knee is the description of a large number of different diseases. A number of different structures in the knee joint area can be affected by inflammation. In many cases, the causes of inflammation in the knee are previous interventions such as a jointoscopy or knee operation, which can result in bacterial inflammation in the knee as a complication with non-sterile work. After excessive strain on the knee, the bursa in the knee that serves as a cushion can become inflamed (bursitis), in some cases the gout is noticeable as an inflammation in the knee.
If the joint is inflamed, doctors speak of so-called arthritis. Both pathogens such as bacteria and non-infectious causes can be considered for the occurrence of joint inflammation. These usually include rheumatic diseases, which can be accompanied by inflammation in the knee.
The so-called arthrosis is to be differentiated from arthritis. Arthrosis of the knee joint refers to the wear and tear on the articular cartilage in the knee joint. This can also lead to inflammation in the knee and cause pain.
The bursae of the knee joint can also become infected. The inflammation known as bursitis (inflammation of the bursa of the knee) often arises from excessive strain on the knee joint and manifests itself in the typical signs of inflammation on the knee joint.
For diagnosis and therapy, a jointoscopy must be carried out immediately to see the extent and to rinse the joint. Antibacterial therapy is then initiated with immobilization. In the event of overuse, the focus is on protection; gout is treated with a low-meat diet and allopurinol in the long term. If rheumatism is the cause of the inflammation in the knee, a combination of cortisone, ibuprofen and other immunosuppressants is used. In all cases you should see a doctor as soon as possible if pain develops along with reddening and swelling of the knee.
What might also interest you: Pain in the knee
Inflammation in the ear
In most cases, inflammation in the ear is caused by bacteria. A distinction is made between inflammation of the outer ear (External otitis) and otitis media (Otitis media), the separating structure being the eardrum. External otitis affects the auricle and the external auditory canal, causing sharp pain and possibly itching. In addition to bacteria, an ear canal clogged with wax can also cause this inflammation in the ear. Therapeutically, the cleaning of the ear canal and the application of local antibiotics are the main focus.
Acute otitis media is an inflammation in the ear that occurs more frequently in childhood and is favored by ventilation disorders in the middle ear. It is also very painful and can be accompanied by a fever. Hearing is partially impaired. This inflammation in the ear is treated with decongestant nasal drops and painkillers, and oral antibiotics are also used to combat the inflammation. The otitis media must be treated, otherwise complications such as a perforation of the eardrum or spreading to the inner ear can occur.
Inflammation of the shoulder
Inflammation of the shoulder joint as well as the structures surrounding the shoulder joint can be caused by various causes. A general distinction must be made between inflammations, which are due to certain Pathogens such as bacteria or viruses and between inflammations, which have so-called non-infectious causes.
Bacteria or viruses usually do not have the opportunity to infect the shoulder joint and cause inflammation. At a Injury to the joint or one Opening through medical intervention However, pathogens can get into the joint and cause inflammation.
Non-infectious inflammation the shoulder can be caused by different diseases. ly are diseases of the so-called rheumatic form circle responsible for this form of inflammation. A Overload and anatomical factors of the shoulder may be responsible for inflammation of the structures involved in the shoulder joint.
Depending on the cause of the inflammation, taking anti-inflammatory drugs, certain surgeries, physical therapy and muscle building can all help treat the inflammation and prevent it from reoccurring.
Inflammation in the foot
Inflammation of the foot can occur in different places and be caused by different causes.
Both the joints of the foot as well Tendons, Tapes and Muscles can catch fire. Superficial inflammation on the foot is also relatively common. Inflammation on the foot is usually caused by the typical signs of inflammation noticeable. Inflammation on the foot often results in visible reddening and swelling as well as pain and overheating of the affected area. It may also be that normal walking or standing on the affected foot is no longer possible due to the inflammation and pain.
Superficial inflammation of the skin can partially spread to the bone and is usually caused by bacteria. Especially people who suffer from diabetes mellitus should check their feet regularly for superficial inflammation and injuries.
A Attack of gout expresses itself especially on Big toe joint and also causes severe pain. At a Overload inflammation of the foot can also occur.
Recommendations from the editorial team:
Do you already know our articles on the subject of inflammation?
Find out more here!
- Levels of inflammation in the blood
- Inflammation in the intestines
- Inflammation of the pancreas
- Inflammation in the knee