Inflammation of the optic nerve
definition
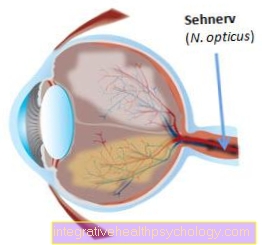
Inflammation of the optic nerve is called Optic neuritis designated. The optic nerve is the second cranial nerve, so it is part of the central nervous system, the brain. It starts at the retina of the eye and forwards the information that was picked up by the eye to the brain. Because of this, the condition often comes with other symptoms that affect the brain.
Inflammation of the optic nerve is most common in people between the ages of 18 and 45 and affects women more often than men. The causes of the disease can be very different and either one or both eyes are affected.
causes

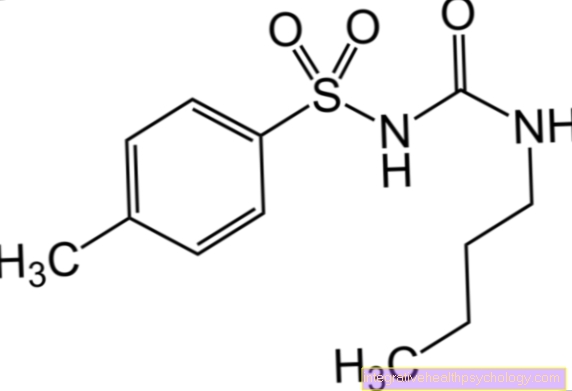
Many underlying diseases can cause inflammation of the Optic nerve to lead. The most common cause (around 20-30% of cases) is autoimmune disease multiple sclerosis (MS). In this disorder are made by the body Antibodies against the envelope structures of the annoy (Myelin sheaths) are formed so that they become inflamed and the conductivity of the nerves is reduced. Gradually, more and more nerves perish. In a typical course of the disease, the myelin sheaths of the optic nerves are first affected. Here comes the Inflammation of the optic nerve both sides (bilateral).
Also the systemic lupus erythematosus (SLE) as another autoimmune disease can cause optic nerve inflammation. This is a systemic disease, which means that the whole body is affected. The formation of antibodies leads to tissue damage, which initially appears as Rashes express. In addition, many organs, e.g. the lung, the heart and the Kidneys be harmed. The central nervous system is also often affected.
In principle, diseases that specifically affect the central nervous system can also lead to inflammation of the optic nerve, as this is part of it. These include e.g. a Meningitis (meningitis) or a brainabscess, so an inflammation in the brain.
Infectious diseases caused by bacteria can also cause the Optic nerve affect. A Lyme disease, by Ticks is transmitted, has severe effects on the central nervous system in the chronic course, e.g. in the form of inflammation of the optic nerves. But also for example malaria, typhus, diphtheria or syphilis can lead to it.
Viral infections can cause optic nerve inflammation more often in children than adults. This is triggered by measles, mumps, rubella, chickenpox, whooping cough or through the Ebstein-Barr viruswho that Pfeiffer's glandular fever evokes.
Inflammation of the Sinuses can also access the bone and from there to Optic nerve and lead to inflammation here.
In addition, poisoning can also result from excessive consumption of alcohol or quinine cause inflammation of the optic nerve. Quinine is used as a remedy against malaria used and is also used against in some drugs flu-like infections in front.
Also Hereditary diseases can lead to optic nerve inflammation, but are comparatively rare.
Symptoms

First, the inflammation of the optic nerve leads to a loss of visual acuity (visual acuity). If the progress is slow, this is usually not noticed immediately by the patient. Most of the time, however, central visual field deficits, the so-called deficits, then occur suddenly, i.e. in the course of a few hours (sometimes even days) central scotoma. This is to be understood as the fact that in the middle of the field of vision, that is, in the area that is captured with one eye, no more visual perception can take place. The person concerned then sees a black point in the middle of his picture of the environment. Depending on whether one or both eyes are affected, this can be noticed on one or both sides. In extreme cases, this visual field loss can get worse and worse, until it leads to complete blindness. However, this is extremely rare and the impairment of vision usually declines over time.
Often, however, pain occurs when pressure is exerted on the affected eye and when the patient moves the eye when turning. Often perceived as an eye socket headache, these are persistent but worsen when pressure is applied.
Sometimes the pupil reflex is impaired in the course of the disease, that is, the narrowing of the pupil when exposed to light and the enlargement in the dark no longer work properly. The red-green perception can also be disturbed.
As a rule, an improvement in symptoms occurs after about 2 to 4 weeks. However, it can be that a slight contrast disturbance remains in the vision.
If the disease recurs again and again, it is called a chronic course. It can happen that the loss of vision continues to decrease and the optic nerve is increasingly irritated by the inflammation and then atrophied. In this case vision cannot be completely restored.
Read more about the topic here: Pupillary reflex
Diagnosis

An ophthalmologist should be consulted with existing visual field deficits or headaches in the area of the eye socket. This examines the fundus of the eye (ophthalmoscopy) by shining a certain lamp into it and reflecting it. Here he can see the exit of the optic nerve from the eye (blind spot). In spite of the existing inflammation of the optic nerve, this examination is often normal, as only the exit point and not the entire course of the nerve can be recognized. Only in rare cases, when the inflammation affects precisely this starting point of the nerve, the ophthalmologist can see a swelling, the so-called papillary swelling. This swelling can also be a sign of increased intracranial pressure, which is why the cause must urgently be clarified with this finding.
One speaks either of an intrabulbar inflammation, i.e. an inflammation in the eyeball or, in contrast, of a retrobulbar inflammation in the case of damage behind the eyeball.
The ophthalmologist also checks visual acuity by reading out numbers, for example, from a distance with one eye at a time. The field of view is also determined in order to identify possible failures. This procedure is called visual field perimetry and is based on the fact that the patient is supposed to recognize one point of light that is approaching him from the side.
In addition, the pupil reflex is tested by the ophthalmologist shining a small lamp into each eye and observing the reactions of the pupils. Normally, when shining into one eye, the pupils of both eyes should narrow (consular pupillary reaction). If, however, the optic nerve in one eye is inflamed, this means that both pupils do not narrow enough. The Swinging Flashlight Test offers a more detailed examination.
If the ophthalmologist finds abnormal findings, these should be clarified further. Magnetic resonance tomography (MRT) of the brain with a contrast agent can be helpful here, as this can be used to identify the areas that may have defects in their envelope structures. These areas are known as foci of demyelination and they can indicate multiple sclerosis. In addition, the nerve conduction velocity can be measured by a neurologist. If this is reduced, this is an indication of an inflammation of the optic nerve.
When making a diagnosis, it is very important to check for neurological diseases such as multiple sclerosis. In addition, attention should be paid to whether a fever or a rash is added to the visual problems, as this indicates an infection.A blood test may also be necessary to detect any changes in the blood count or to determine whether there are any bacteria in the blood.
therapy
Mostly one shows Inflammation of the optic nerve even without therapy spontaneous healing and the Visual acuity improves by itself.
However, the underlying disease should still be identified in order to treat it. In about two thirds of those affected this is multiple sclerosis which cannot be cured, but medication can improve symptoms. Anti-inflammatory drugs are used that cortisone contain.
Is infection through bacteria Cause of the disease so need special Antibiotics are used that are accessible to liquor, that is, the Blood-brain barrier can overcome and also im brain can develop their effect.
In children who have a Viral infection a Optic nerve inflammation no further therapy is usually necessary and the loss of vision is on its own.
Exertion and heat should definitely be avoided. Driving a vehicle is also not advisable in the case of optic nerve inflammation, as that Very limited eyesight is and one high risk of accidents consists.